I. OVERVIEW
A. From Greek-Ortho: “Straight” or “correct” + Gnath: “jaw”
B. Goals of treatment include restoration of form and function
1. Restoration of ideal facial proportions
2. Restoration of functional occlusion for mastication
II. DENTITION
A. Pediatric: Primary or deciduous teeth
1. Eruption sequence (months)
a. *Incisors: 6 months; first teeth
b. First molars: 12 months
c. Canines: 16 months
d. Second molars: 20 months
2. Nomenclature for the 20 primary teeth
a. Letter system: A–P
b. Mnemonic: All Just Kids Teeth
i. A, right maxillary second molar
ii. J, left maxillary second molar
iii. K, left mandibular second molar
iv. T, right mandibular second molar
B. Mixed dentition: When both primary and secondary teeth are present; age 6 to 9 years
C. Adult: Secondary, permanent
1. Eruption sequence (years)
a. *First molars: 6 to 7; first adult teeth
b. Incisors: 6 to 9
c. Canines: 9 to 10
d. First premolars: 10 to 12
e. Second premolars: 11 to 12
f. Second molars: 11 to 13
g. Third molars: 17 to 21; “wisdom” teeth
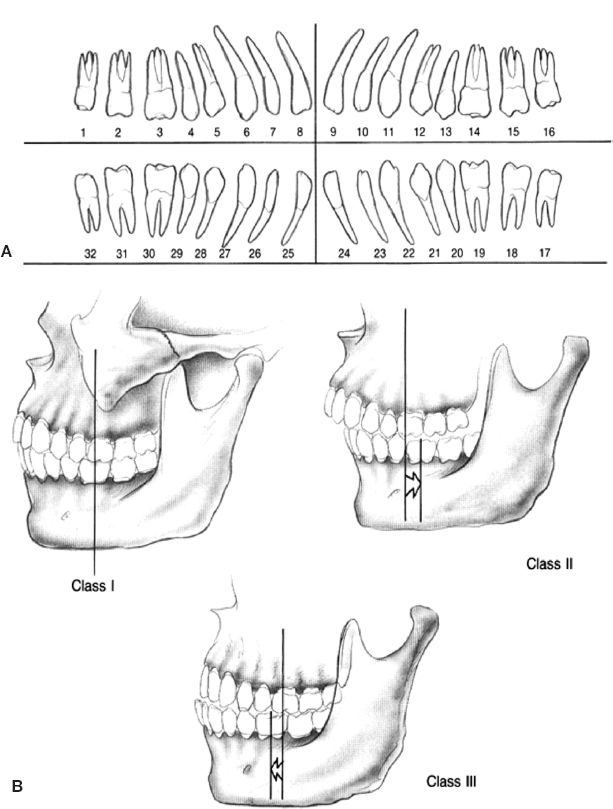
2. Numbering (international standard): 1 to 32 (Fig. 29-1A)
a. 1, right maxillary third molar
b. 17, left mandibular third molar
III. DENTAL ANATOMY
A. Crown: Above the gingiva
B. Root: Within the bone
C. Cusp: Protruding portion of occlusal surface
D. Groove: Intruding portion of occlusal surface
IV. TERMINOLOGY
A. Mesial: Toward midline (e.g., incisors are mesial to molars)
B. Distal: Away from midline
C. Buccal: Toward the cheek
______________
*Denotes common in-service examination topics
Figure 29-1. Teeth (A) and Angle classification of occlusion (B).
D. Lingual: Toward the tongue
E. Overbite: Vertical relationship of the maxillary and mandibular tooth apices
F. Overjet: Horizontal relationship of the maxillary and mandibular tooth apices
G. Proclination: Angulation of apex toward the lips
H. Retroclination: Angulation of apex toward the tongue
I. Apertognathia: Open bite, negative overbite
J. Incisal show: Amount of vertical show of maxillary central incisor in repose
K. Centric occlusion: Maximal intercuspation of teeth
L. Centric relation: Mandibular condyles fully seated in glenoid fossae
M. Open bite: Part of the dentition does not occlude (can be anywhere)
N. Deep bite: A pronounced overbite
O. Crossbite: Can be buccal, neutral (normal), or lingual. Often caused by tilting of the maxillary teeth.
V. *ANGLE CLASSIFICATION (EDWARD HARTLEY ANGLE, “FATHER OF MODERN ORTHODONTICS”)
A. Based on the relationship of maxillary first molar (Fig. 29-1B)
B. Class I: Mesial buccal cusp of maxillary first molar in buccal grove of mandibular first molar
C. Class II: Mesial buccal cusp of maxillary first molar is mesial to buccal grove of mandibular first molar
1. Division 1: Excessive overjet with normal angulation of maxillary incisor
2. Division 2: Retroclination of maxillary incisors
D. Class III: Mesial buccal cusp of maxillary first molar is distal to buccal grove of mandibular first molar
VI. ORTHOGNATHIC SURGERY EVALUATION
A. Close coordination with orthodontist
B. Complete medical and dental history
1. Functional problems: Temporomandibular joint (TMJ) derangement, obstructive sleep apnea (OSA), masticatory difficulty, history of cleft lip/palate
2. Aesthetic concerns
C. Oral exam
1. Occlusion: Number of dental contacts; Angle classification
a. Curve of Spee: AP curvature of occlusal plane
b. Curve of Wilson: Lateral curvature of occlusal plane
2. Midline: Coincidence (alignment) of maxillary and mandibular central incisors
3. Cant: Discrepancy of occlusal plane from horizontal
4. *Ideal incisal show
a. 2 to 4 mm in women
b. 0 to 2 mm in men
5. Restorations and overall oral hygiene health
6. TMJ: Crepitus, subluxation, and pain
D. Aesthetic evaluation
1. Neoclassical canon (see Rhinoplasty, chapter 30)
a. Measure horizontal thirds and vertical fifths
b. Assess nose–lip–chin relationship
2. Determine facial symmetry
E. Radiographic (cephalometric) evaluation
1. PA and lateral cephalogram ± orthopantomogram (Panorex)
2. Determine convexity/concavity
3. Facial divergence
a. Anteriorly divergent: Soft-tissue pogonion anterior to glabella
b. Posteriorly divergent: Soft-tissue pogonion posterior to glabella
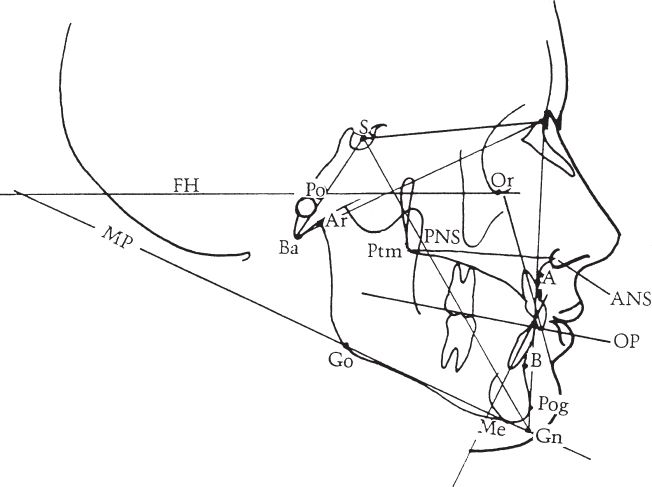
4. *Key anatomic points on lateral cephalogram (Fig. 29-2)
a. Sella: Midpoint of the sella turcica of sphenoid bone
b. Nasion: Most concave point on the nasal bone
c. A point: Most concave point on the maxilla
d. B point: Most concave point on the mandible
c. Normative values (differ based on race/ethnicity, sex)
i. SNA = 82
II. SNB = 80
F. Treatment planning
1. Expansion of the soft–tissue envelope with anterior skeletal movement is generally preferred to the opposite
a. Anterior movements produce a more youthful, rather than aged, appearance
b. Consider but “ignore” normative angles
2. “Decompensate” occlusion
a. Orthodontic correction of proclined/retroclined teeth in preparation for anticipated postoperative occlusion
b. Worsens preoperative occlusion
Figure 29-2. Standard lateral cephalometric tracing with landmarks. FH, Frankfort Horizontal; MP, Mandibular plane; Po, Pogonion; S, Sella; Ba, Basion; A, articulare; Ptm, Pterygomaxillary fissure; PNS, Posterior nasal spine; PO, Porion; ANS, Anterior nasal spine; OP, Occlusal plane; Or, Orbitale; Pog, Pogonion; Go, Gonion; Me, Menton; Gn, Gnathion; A, Point A (most posterior point of maxilla cephalad to teeth); B, Point B (most posterior point of mandible caudal to teeth)
3. Virtual surgery can be helpful in preoperative planning
a. Two-dimensional software (e.g., Dolphin)
b. Predicts soft tissue response to skeletal movement
c. Estimates postoperative SNA/SNB angles
d. Three-dimensional treatment planning is also used (e.g., Medical Modeling)
4. Casts, model surgery, and occlusal splints
a. Dental impressions followed by plaster casts
b. Casts enable determination of maximal intercuspation: Centric occlusion
c. Casts facilitate fabrication of occlusal splint to guide skeletal segments into position following osteotomy
i. For “two-piece” Le Fort I cases (i.e., maxillary arch must be widened with sagittal osteotomy), a splint is required to maintain desired palatal width
ii. For “two-jaw” or “double-jaw” cases (i.e., maxillary and mandibular osteotomies), two splints are required: Intermediate and final
d. In “double-jaw” cases, facebow transfer is required to establish the relationship of the maxilla to the skull base
i. Bite registration needed to then relate mandibular cast to maxillary cast on articulator
ii. Maxillary cast osteotomy (model surgery) performed on articulator to fashion intermediate splint
iii. Final splint fabricated on separate models mounted on Galetti articulator
5. Arch bars or braces with brackets required
A. *Vertical maxillary excess
1. Long face/“gummy smile” with excess gingival show
2. >4 mm incisor show
3. Mentalis strain
4. Flattened midface
5. Class II malocclusion most common, but can have any occlusion
6. SNA and SNB are decreased; ANB increased
7. Etiology: Open-mouthed breathing–nasal airway obstruction, myotonic dystrophy, adenoid hypertrophy, and familial
8. Treatment: Le Fort I impaction, possible mandibular advancement. With maxillary impaction, mandible will autorotate into occlusion with maxillary dentition
a. This will improve SNB angle without mandibular osteotomy
b. Concomitant genioplasty sometimes needed to correct relative chin retrusion or midline menton discrepancy
B. Vertical maxillary deficiency
1. Short face: See very little maxillary dentition in repose and with smiling
2. No incisor show
3. Aged, edentulous appearance
4. Prominent chin with jowling
5. Class II malocclusion
6. Increased SNA and SNB angles
7. Treatment: Downfracture Le Fort I with bone grafting, possible mandibular advancement
8. Orthodontics: Curve of Spee (vertical wave in occlusal plane) is corrected postsurgically
C. Maxillary retrusion/midface hypoplasia
1. Flat or dish face
2. Depressed nasal tip and wide alar base
3. Negative overjet
4. Short upper lip
5. Class III malocclusion
6. Decreased SNA; normal to larger SNB; negative ANB
7. Etiology: Often history of cleft lip ± palate, CPAP (continuous positive airway pressure) during childhood
8. Treatment: Maxillary advancement
a. High-winged Le Fort I
i. Improves malar position with one operation
ii. Obviates need for implants or bone grafts
b. Le Fort I via distraction osteogenesis
i. Used in large advancements (>10 mm)
ii. Requires halo mounted to cranium during initiation, activation, and consolidation phases
iii. Unable to precisely establish final occlusion
c. *Le Fort I advancement changes the nasal appearance
i. Widened alar base
ii. Increased tip projection
iii. Increased nasolabial angled.
iii. Narrowing of upper lip show (smaller vermillion)
d. Soft tissue of upper lip moves 0.5 to 0.9 compared with the bone
D. Retrognathia
1. Decreased mandibular projection
2. Obtuse cervicomental angle
3. May have excessive eversion of lower lip
4. Redundant submental soft tissue
5. Class II malocclusion
6. Decreased SNB angle
8. Orthodontic presurgical management seeks to eliminate crowding (limits the amount by which the mandible can be advanced)
9. Etiology: May have history of Pierre Robin sequence
10. Treatment: Bilateral sagittal split osteotomy (BSSO), possible genioplasty
E. Prognathia
1. Prominence mandible with apparent midface retrusion
2. Mandibular over-rotation
3. Class III malocclusion
4. Increased SNB angle
5. Negative overjet
6. Treatment
a. Consider maxillary advancement only
b. Setback mandible only in severe cases
i. BSSO
ii. Intraoral vertical ramus osteotomy (IVRO)
a) If setback is >10 mm
b) Requires postoperative maxillomandibular fixation (MMF)
F. OSA
1. With severe OSA not amenable to CPAP, “bi-max” advancement is considered
2. Advancement of maxillomandibular skeleton improves airway patency
VIII. OPERATIVE TECHNIQUES
A. Anesthetic considerations
1. Hypotensive anesthesia, and
2. Reverse Trendelenburg positioning (head up) reduces bleeding intraoperatively
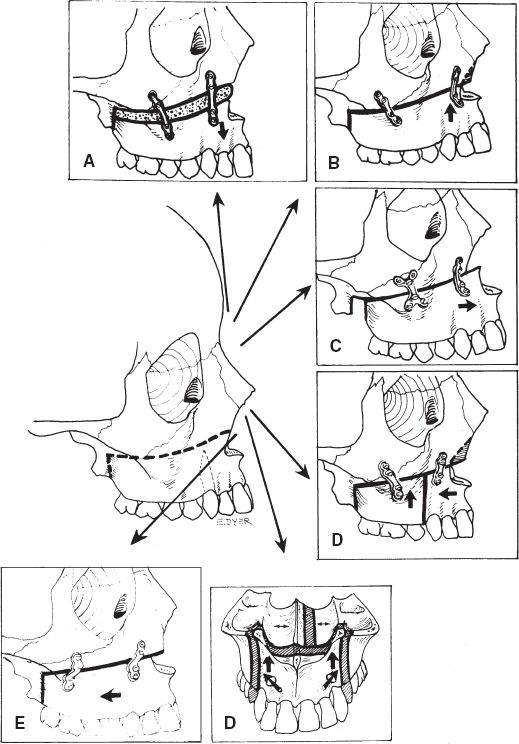
B. Le Fort I osteotomy (Fig. 29-3)
1. Upper buccal sulcus incision
2. Leave 2- to 3-mm cuff of tissue on gingiva for closure
3. Avoid parotid papilla
4. Identify infraorbital nerve in midpupillary line
5. Dissect along buttresses in subperiosteal plane
6. Elevate mucosa from nasal floor, septum, and sidewalls
7. Buttress osteotomies
a. Nasomaxillary: Reciprocating saw directed from piriform aperture medial to lateral in horizontal plane
b. Zygomaticomaxillary: Reciprocating saw directed from lateral to medial in horizontal plane
c. Pterygomaxillary: Curved (e.g., Kawamoto) osteotome placed behind maxillary tuberosity into pterygomaxillary fissure
d. Nasal septum divided using double-ball, guarded osteotome
e. Check lip–tooth relationship with acrylic splint in place
f. Plate fixation at piriform ± maxillary buttress
g. V-Y vestibular closure to prevent excess nasal widening, thinning of upper lip, and downturning of the corner of the mouth
h. Check occlusion and revise hardware if incorrect
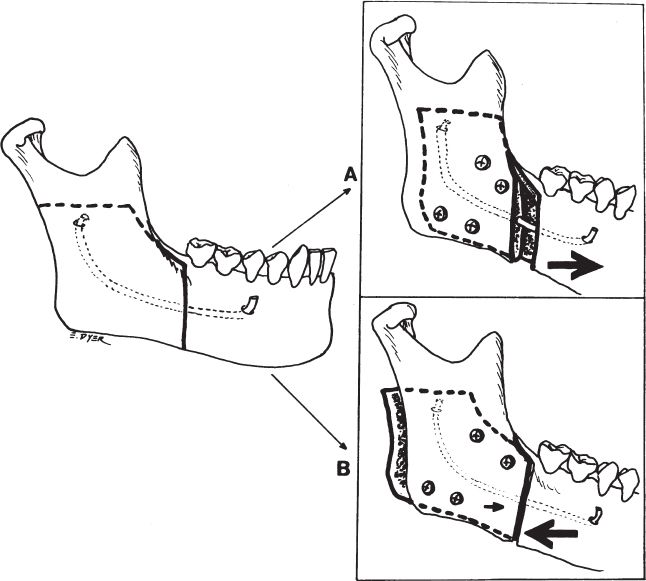
C. Bilateral sagittal split osteotomy (BSSO) (Fig. 29-4)
1. Requires removal of third molars ~6 months preoperatively
2. Intraoral incision over ascending ramus and external oblique ridge
3. Subperiosteal dissection on medial surface of ramus
a. Above the level of occlusal plane at lingula
b. Point where inferior alveolar nerve enters the mandible
4. Step-wise osteotomy in sagittal plane
5. Segments mandible into three segments
a. Proximal (two segments, bilateral): Contains ramus and condyle
b. Distal (one segment, central): Contains body, both branches of inferior alveolar nerve
6. Acrylic splint guides the distal segment into occlusion
Figure 29-3. Versatility of the Le Fort I osteotomy. The LeFort osteotomy can be varied to position portions of the maxilla in various ways. A: Inferior displacement (with bone graft) to increase vertical length. B: Impaction to reduce maxillary height. C: Anterior movement of the maxilla is possible. D: The surgeon may adjust the width of the maxilla as needed. E: Posterior movement of the maxilla is possible as well.
7. Transbuccal trochar is used to assist in bicortical screw fixation of both mandibular segments
8. Seat condyles in glenoid fossa (centric relation) during fixation
9. Check occlusion on release of MMF and revise hardware if incorrect
D. Intraoral vertical ramus osteotomy (IVRO)
1. Intraoral incision over ascending ramus and external oblique ridge
2. Subperiosteal dissection on lateral surface of ramus
a. Posterior to entrance of inferior alveolar nerve
b. Splits mandible in coronal plane between condyle and coronoid (sigmoid notch)
c. Internal maxillary artery traverses this bony interval
Figure 29-4. The sagittal split osteotomy. It may be used to move the anterior mandible into a more anterior position (A) or, more rarely, into a more posterior position (B).
3. Less favored technique of mandibular osteotomy
4. Used when large mandibular setback is required (i.e., Class III malocclusion)
5. No osseous fixation employed; requires MMF postoperatively
E. Genioplasty
1. Lower buccal sulcus incision
2. Leave the cuff of mucosa and mentalis muscle for two-layer closure
3. Subperiosteal dissection centrally and along inferior mandibular border to reveal mental nerves
a. Located between first and second premolars
b. *May course ~2 mm beneath the mental foramen before exiting
4. Transverse osteotomy with sagittal saw
5. Measured step plates may be used to achieve fixation at desired location
F. “Double-jaw” surgery
1. Le Fort I
2. BSSO or IVRO
3. Performed in series, beginning with Le Fort I osteotomy
4. Intermediate and final occlusal splints used to establish occlusion
IX. POSTOPERATIVE CARE
A. Use of elastic bands
1. Temporary elastics used to secure desired occlusion during fixation
2. Often removed prior to extubation
3. May be left in place as “guiding elastics”
i. Used to “correct” a class II malocclusion
ii. Vector from anterior maxilla to posterior mandible
b. Class III elastics
i. Used to “correct” a class III malocclusion
ii. Vector from anterior mandible to posterior maxilla
B. MMF
1. Used in cases of suboptimal fixation or in large/unstable skeletal movements
2. May be kept in place for several months
3. Wire cutters required at bedside in cases of airway compromise and/or emesis
C. Steroid (fluocinolone) cream used for labial swelling
D. Peridex mouth rinses
E. Soft diet
F. Elevate head of bed and employ cool compresses
X. COMPLICATIONS
A. Relapse
1. Surgical: Loss of plate fixation (malunion)
2. Dental: Malpositioned teeth; requires appropriate decompensation
3. Condylar
a. Resorption of bone at condyle (progressive condylar resorption)
b. Related to residual apertognathia and unfavorable TMJ dynamics
4. Soft tissue: Recoil forces from “Moss’ functional matrix”
B. *Paresthesia
1. Risk of inferior alveolar nerve injury in BSSO is 10%
2. About 90% of patients have temporary postoperative symptoms
C. Infection: May require abscess drainage, but not removal of hardware in most cases
D. Hemorrhage
1. Le Fort osteotomy may damage internal maxillary artery branches and pterygoid venous plexus during pterygomaxillary disjunction
a. Maintain subperiosteal dissection
b. Ensure osteotome placement in pterygopalatine fossa
2. Use hypotensive anesthesia (SBP ~80 mmHg) and reverse Trendelenburg position
E. Ischemia
1. Rare occurrence in Le Fort I advancement, presents as dusky, violaceous mucosal appearance
2. More common in
a. Large anterior movements
b. Cases of cleft lip and palate, and/or
c. Two-piece movements with osseous discontinuity
3. Blood supply to Le Fort I segment
a. Interruption of descending palatine a. after osteotomy
b. Maintained on ascending palatine branch of facial a
c. Anterior branch of ascending pharyngeal a., through mucosal attachments
QUESTIONS YOU WILL BE ASKED
1. The location of the mental and infraorbital foramina and nerves
a. Mental n.: Between first and second mandibular premolars
b. Infraorbital n.: ~1 cm below rim in midpupillary line
2. The course of the inferior alveolar nerve within the mandible
a. Enters mandibular foramen at lingula on medial surface of ramus
b. Moves from medial to lateral cortex distally
c. Curves below mental foramen prior to exiting
3. Characteristic nasolabial changes following Le Fort I advancement
a. Alar widening
b. Increased tip projection
c. Vertical lip shortening
4. The difference between centric occlusion and centric relation
a. Centric occlusion: Maximal intercuspation of the teeth in wear facets
b. Centric relation: Normal resting relationship of mandibular condyle in glenoid fossa
c. CO-CR shift
i. Sacrifice of centric relation in order to obtain occlusion and increase mandibular projection
ii. Common in class III malocclusion
Recommended Readings
1. Legan HL, Burstone CJ. Soft tissue cephalometric analysis for orthognathic surgery. J Oral Surg. 1980;38(10):744-751. PMID: 6932485.
2. Panula K, Finne K, Oikarinen K. Incidence of complications and problems related to orthognathic surgery: a review of 655 patients. J Oral Maxillofac Surg. 2001;59(10):1128-1136; discussion 1137. PMID: 11573165.
3. Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996;11(3):191-204. PMID: 9456622.
< div class='tao-gold-member'>