20 Omentum reconstruction of the breast
Synopsis
 The use of the omentum flap is flexible, safe and provides several operative solutions.
The use of the omentum flap is flexible, safe and provides several operative solutions.
 Videolaparoscopic approach is very safe, takes 60–90 min and provides fast postoperative recovery.
Videolaparoscopic approach is very safe, takes 60–90 min and provides fast postoperative recovery.
 This technique is mainly used in skin sparing mastectomy.
This technique is mainly used in skin sparing mastectomy.
 The omentum flap can be used to create a central volume on the reconstructed breast or to cover a breast implant.
The omentum flap can be used to create a central volume on the reconstructed breast or to cover a breast implant.
 It is a great surgery for repair of a failed reconstruction.
It is a great surgery for repair of a failed reconstruction.
History
Use of an omental flap to reconstruct the breast after cancer surgery was first reported by Kiricuta in 1963.1 Since then, the omentum has been widely used in reconstructive surgery to cover extensive thoracic defects associated with radionecrosis and tumor extirpation.2–13 This flap, whose main blood supply includes the gastroepiploic vessels, was initially used in breast reconstruction to cover an implant, and final coverage was obtained by skin grafting. The aesthetic result was unsatisfactory due to the final shape and quality of the skin coverage. The omentum has previously been employed by Erol14 as a pedicle to vascularize the lower abdominal skin flap, allowing its rotation into the mastectomy site. This was accomplished by a staged procedure, in which the omentum was rotated into the subcutaneous plane and allowed to grow into the subcutaneous fat of the lower abdominal panniculus. The flap was then rotated in a secondary procedure into the mastectomy defect. However, as creative as this technique was, it had the disadvantages of requiring multiple stages and potential complications and risks related to laparotomy.
Treatment/surgical technique
Laparoscopic harvesting of the omental flap
The surgeon, positioned between the patient’s legs, mobilizes the omentum using a forceps and an ultrasound-assisted dissector. Metallic clips are employed for hemostasis of vessels whose diameter exceeds 1 mm. Dissections between the omentum and colon progresses from left to right exposing the posterior portion of the stomach (from the duodenum to the gastric fundus), keeping the omentum connected to the stomach by its gastroepiploic pedicles (Fig. 20.1). The left gastroepiploic pedicle is ligated using a 30-mm linear endoscopic stapler.
The omentum is exteriorized through a 5–6 cm midline incision in the upper epigastric region. The gastric branches of the gastroepiploic arcade are ligated from left to right until the right gastroepiploic pedicle is completely isolated. Extreme care must be taken when exteriorizing the flap to avoid torsion or kinking of the pedicle. The flap is then tunneled subcutaneously toward the mastectomy site (Fig. 20.2). Aponeurosis is closed in the epigastric region using 0 Prolene sutures, leaving a 2 cm opening for the flap’s pedicle. At this moment, the pedicle must be checked once more for kinking, compression, or torsion. The subcutaneous layers and skin are finally closed using Monocryl 4-0 sutures.
Omentum reconstruction
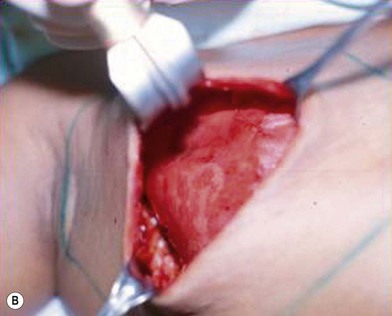
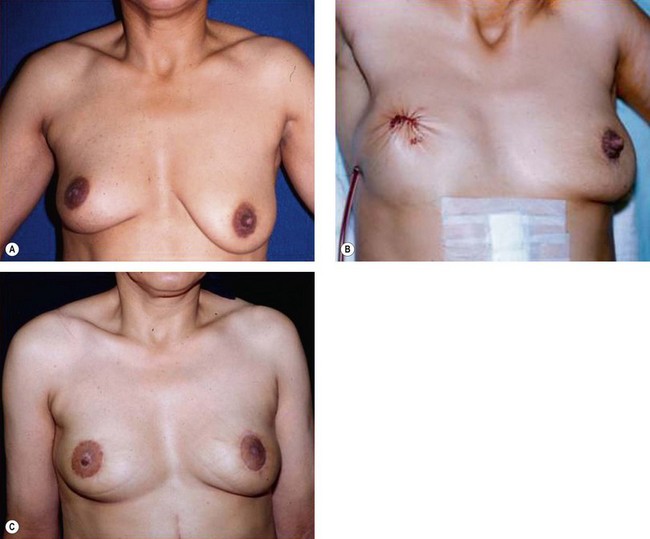
The synthetic mesh is then placed over the omentum to shape and support the new breast. Fixation of the mesh to the pectoralis major muscle is carried out using titanium clips or interrupted nylon 4-0 sutures (Fig. 20.3). Skin closure is performed using a Mersilene 3-0 purse-string suture to completely cover the new breast cone, define its limits and complete the shaping process. Suction drains exteriorized at the level of the anterior axillary line are kept for 5 days or until drainage is <20 mL/day. Figure 20.4 shows the preoperative condition for comparison purposes and Figure 20.4B demonstrates the immediate postoperative shape created.