Introduction
Nonmelanoma skin cancer (NMSC) is the most common malignancy amongst Caucasians and occurs sporadically in all other populations. NMSCs are comprised predominantly of basal cell (BCC) and squamous cell (SCC) carcinoma, among other rarer types of cutaneous malignancy. UV radiation exposure initiates approximately 90% of NMSCs, resulting in malignant transformation of keratinocytes. Despite improvements in public awareness and warnings of the harmful effects of excessive ultraviolet (UV) exposure, the incidence of NMSC has risen by 3%–8% per year since 1960 with an almost 300% increase in the past two decades in the United States. This trend is predicted to continue as populations age worldwide. Fortunately, NMSC mortality is reducing due to a combination of earlier diagnosis and advances in treatment. While traditional treatment modalities once centered on surgical excision, there have been steady advances in nonoperative modalities, resulting in a broader spectrum of treatment options. As leaders in surgery of the skin and related tissues, it is essential that plastic surgeons have a thorough understanding of NMSC, including both current and future management options, so that the important trend of improved survival continues long into the future.
Basal Cell Carcinoma
Epidemiology
Keratinocyte tumors make up 90% of all malignant skin diseases and basal cell carcinomas comprise approximately 70% of keratinocyte tumors. BCC makes up over three-quarters of all NMSCs and affects 1 million people in the United States each year. It is rarely metastatic, however it can cause significant morbidity via local invasion. While the pathogenesis is attributed to an interplay between patient exposure to environmental factors and patient-derived characteristics, most BCCs are sporadic. Environmental exposures are the major etiological factor, with a latency period of anywhere between 20 and 50 years from point of exposure to the development of the BCC. As such, most sporadic BCCs occur in older males (>50 years of age) with fair complexions, typically classed as Fitzpatrick skin types 1 and 2.
Risk Factors
BCCs can develop early in life, but age is an independent risk factor whereby the incidence rate doubles from 40 to 70 years of age. Intensive, intermittent UV exposure (particularly UVB rays) resulting in sunburn and blistering (particularly during childhood and adolescence) is a major risk factor for BCC. Fair skin types (Fitzpatrick skin types 1 and 2) and individuals in hot climates are at greater risk of incidental intermittent sunburn. In Australia, which experiences the greatest UV solar irradiation per area of any continent, these factors combine to produce the highest incidences of NMSCs and melanoma in the world. Additional environmental factors include tanning bed use, chronic inflammation (burns), ionizing radiation, arsenic and hydrocarbon exposure. Immunosuppression poses an elevated risk of BCC development, particularly among human immunodeficiency virus (HIV)-positive patients (fivefold greater incidence) and organ transplant recipients using photosensitizing antifungal prophylaxis such as voriconazole. The association between human papillomavirus and BCC is not yet clear.
Genetics
Multiple genes have been implicated in the development of BCC, including tumor suppressor genes, DNA repair genes, and genes involved in skin and skin appendage pigmentation. Approximately 90% of sporadic BCCs have activating mutations in the Hedgehog-signaling pathway, resulting in uncontrolled proliferation of epidermal basal cells. This pathway was identified by studying patients with basal cell nevus syndrome (BCNS), also referred to as Gorlin syndrome, an autosomal dominant disease with constitutive mutations of the Hedgehog pathway. The specific gene involved in the majority of cases is the tumor suppressor Patched gene ( PTCH1 ) (chromosome 9q), mutations of which lead to an increased risk of developing multiple BCCs from a young age, as well as a cluster of: keratocystic odontogenic tumors (KCOTs) in 75% of patients; palmar and plantar pits ( Fig. 9.1 ); multiple skeletal abnormalities (e.g., bifid ribs, frontal bossing); and calcification of the falx cerebri. Approximately 10% of BCNS patients do not develop BCCs, indicating the involvement of multiple genes. The tumor-suppressor gene p53 and melanocortin-1 receptor gene ( MC1R ) are also important for the development of BCC, but much less specific to this tumor. Those with pigment disorders and defects in DNA repair mechanisms, such as albinism and xeroderma pigmentosum, respectively, are also more susceptible to NMSC development.

Pathogenesis
BCC is a cutaneous malignant proliferation which is derived from basaloid cells. Basal cell carcinomas grow slowly, whereby the doubling time is 6–12 months. Individuals presenting with a BCC are at increased risk of having more lesions at the time of diagnosis and a 3-year cumulative risk for a second primary of 44% (10-fold increase over the general population). They can be locally invasive, involving subcutaneous tissue, muscle, and bone ( Figs. 9.2 and 9.3 ). Micronodular, morpheaform or infiltrative BCCs are more likely to recur after treatment. Long-term follow-up and annual skin examinations are warranted in those with a history of BCC, as they are also at an increased risk of developing other skin cancers. BCCs exhibit stromal dependence where tumor cells cannot engraft elsewhere without being transplanted along with adjacent stromal cells. Correspondingly, the incidence of metastasis is reported to be less than 0.55% and is associated with larger primary tumor size, greater depth of invasion, previous irradiation and central facial position rather than tumor subtype. When metastasis occurs, lymph nodes and lungs are the most commonly involved. Since 1981, 238 cases of metastatic BCC have been reported, most of which occurred in middle-aged men with an average tumor size of 7.5 cm and a median time of 9 years between primary tumor and first sign of metastasis. Once metastasis does occur, the median survival is 10 months.

Clinical Presentation and Classification
BCCs usually present on sun-exposed areas, such as the head and neck, however they can occur in more occult photo-protected sites, particularly in the immunosuppressed. Due to its prevalence, multiple BCC classification systems have been developed, however a clinicopathological method is the most common in clinical use.
Commonly described subtypes include: superficial; nodular; micronodular; morpheaform/desmoplastic; infiltrating; pigmented and mixed ( Table 9.1 ). A more simple, management-oriented approach is to classify BCCs as either discrete or diffuse, referring directly to how easy it is to judge their margins. This approach groups poorly circumscribed lesions (e.g., micronodular, morpheaform, infiltrative) on the basis that wider margins of excision are necessary to achieve clearance when compared with discrete lesions (such as superficial and nodular types). The anatomic location of BCCs may also favor the development of a particular subtype.
| Subtype | Clinical Features | Histopathological Features |
|---|---|---|
| Superficial | Typically appear on the trunk as single or multiple well-defined erythematous finely-scaled patches or plaques with pearly rolled edges | Multifocal nests of atypical basiloid cells arising from basal layer of epidermis. These remain confined to the papillary dermis |
| Nodular | Typically a pearly papule or nodule with raised, rolled edges and telangiectasia. To assess: put lesion under tension to demonstrate pearling and then release to show refilling of telangiectasia. Ulceration occasionally present | Discrete nests of malignant basiloid cells in the dermis. Peripheral palisading. Mucoid stroma containing plump spindle cells |
| Micronodular | Multiple erythematous macule or thin papule/plaques most commonly found on the back. Nodules do not appear to be contiguous | Multiple small basaloid nests within the dermis. Individual nests are part of a complex network of intercommunicating tumor processes. May exhibit infiltration into surrounding tissues |
| Morpheaform/Desmoplastic | Appear as depressed, scar-like, ill-defined, indurated plaques often with focal penetration of tissues. Direct perineural invasion can occur | Thin strands of basiloid cells surrounded by a sclerotic collagenous stroma |
| Infiltrative | Similar clinically to morpheaform subtype as are clinically diffuse, indurated and poorly defined. Can resemble a skin reaction or scar presenting as a depressed whitish plaque most commonly on upper trunk and face | Demonstrate nests and cords of tumor invading the surrounding tissues. Unlike morpheaform there is minimal to absent desmoplastic stromal response (the surrounding tissues can look relatively bland) |
| Pigmented | Pigmented variants of the other subtypes, including nodular, micronodular, multifocal and superficial BCC. Difficult to differentiate from seborrheic keratosis and malignant melanoma. The color varies from dark brown to black | Nests of basaloid cells, with an abundance of melanin and melanophages, and a moderate inflammatory infiltrate |
| Infundibulocystic | Well-defined pearly papule commonly on the head and neck | Anastomosing strands of basaloid cells with multiple infundibulum-like cystic structures |
| Basisquamous | Uncommon and unusual tumor that shares features of both basal cell and squamous cell carcinoma. Distinguished from BCC by their potential for metastasis and therefore clinically should be managed as though they are a SCC | Well-defined nodular or superficial BCC component overlying an invasive front showing BCC and SCC histological features |
Diagnosis and Staging
Dermoscopy
Dermoscopy aids with evaluation of pigmented cutaneous lesions and can be used to help differentiate pigmented BCC from melanoma. Typical findings of BCC on dermoscopy include the absence of a pigment network and at least one of the following: ulceration, multiple blue-gray globules, leaf-like areas, arborizing vessels, large blue-gray ovoid nests, and spoke wheel areas.
Biopsy
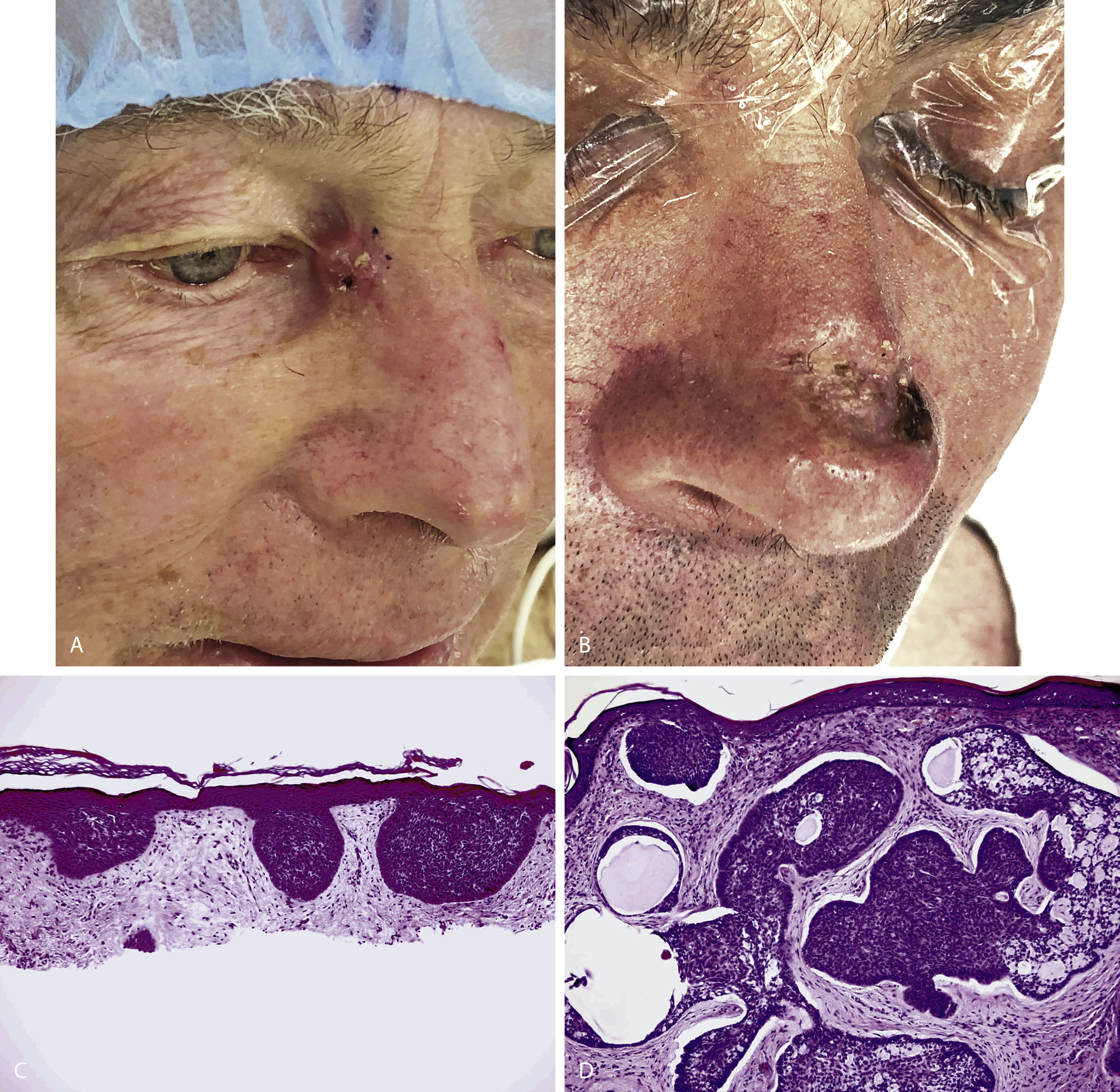
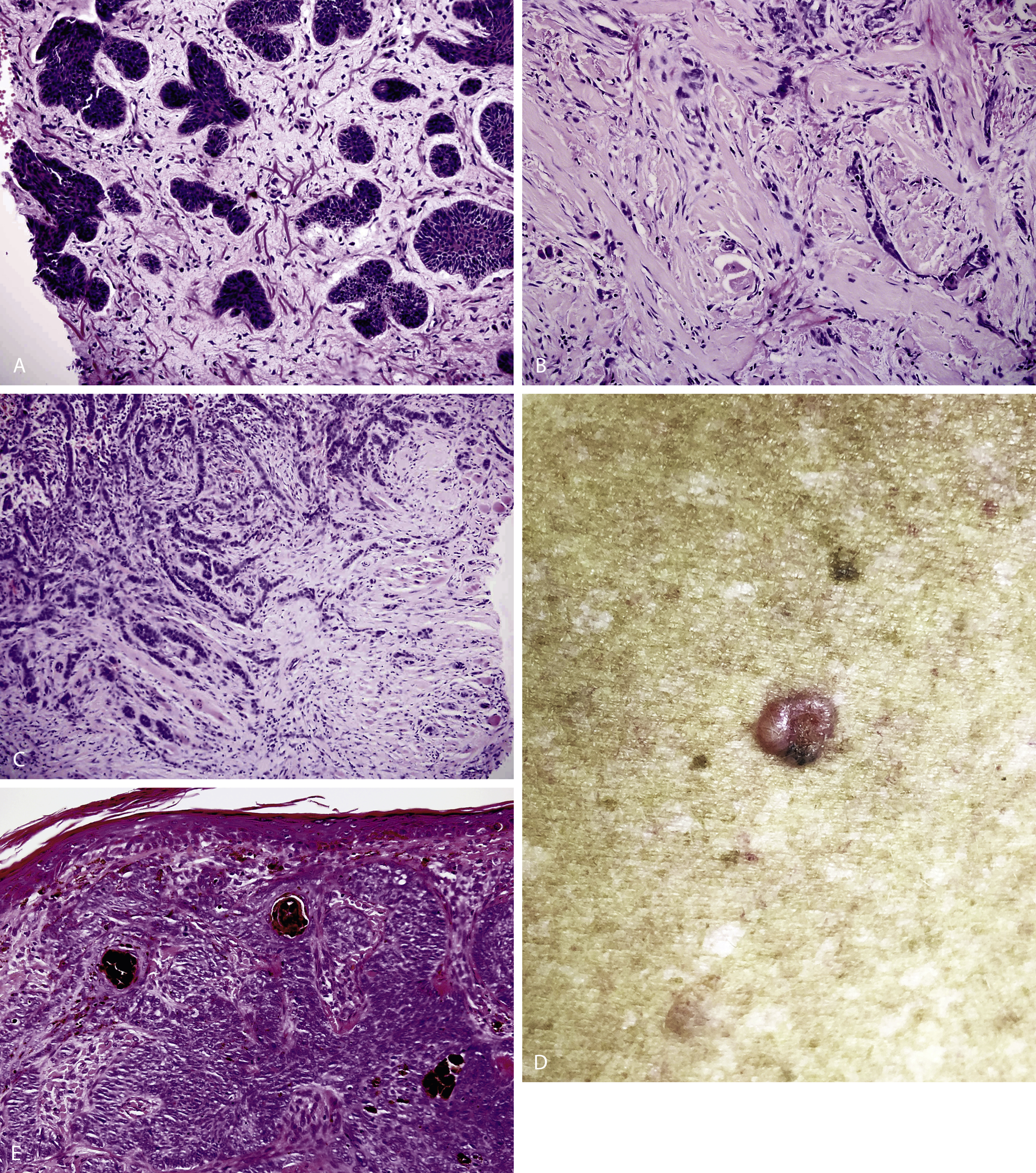
Definitive diagnosis is made on histology following a punch, shave or excisional biopsy of the lesion. Histology of superficial BCC ( Fig. 9.4C ) usually reveals a basophilic tumor (blue) on standard hematoxylin and eosin staining. Buds of basaloid cells extend from the epidermal basal layer into the reticular dermis. Nodular BCCs ( Fig. 9.4D ) have nests of large basaloid cells with peripheral palisading in the papillary or reticular dermis. They may demonstrate peri-nest clefting consistent with retraction from surrounding stroma but this is usually a processing artifact. Micronodular BCC ( Fig. 9.5A ) is composed of multiple microscopic nodules smaller than 15 μm making it difficult to interpret tumor clearance when there are close margins. Tumors become infiltrative ( Fig. 9.5C ) when basaloid islands lose their epidermal connections and invade the underlying dermis, often as sheets or finger-like projections of tumor cells without much stromal reaction. In contrast, morpheaform BCC ( Fig. 9.5B ) consists of strands of tumor cells extending deeply into the dermis embedded within a dense fibrous stroma. Pigmented BCCs ( Fig. 9.5E ) have similar histology to the nodular subtype with numerous melanocytes among the tumor nests and melanophages in the stroma
Staging: TNM and Imaging
See below under Squamous Cell Carcinoma.
Management
Complete surgical excision with pathology confirmation remains the gold standard in the management of basal cell carcinoma. Their abundance in clinical practice, slow doubling time, stromal dependence, and significant rates of spontaneous regression (most studies demonstrate at least some degree of regression in around 20% of lesions ) have prompted the development of numerous treatment options, each with their relative merits. However, their potential to display a mixed clinicopathologic picture, variability in aggressiveness based on type, site, and patient factors and the fact that recurrent BCCs tend to demonstrate poorer prognosis, should prompt management based on the most effective modality in the individual to achieve complete removal or destruction of the tumor. As a result, treatment varies depending on anatomical location, BCC subtype, tumor size, depth of invasion, and patient co-morbidities ( Table 9.2 ).
| Treatment Modality | Indication |
|---|---|
| Topical Cryotherapy Imiquimod a 5-Fluorouracil a | Small superficial BCC Biopsy-confirmed nonfacial superficial BCC <2 cm Nonfacial superficial BCC <2 cm |
| Oral Vismodegib | Locally advanced and metastatic BCC Neoadjuvant use prior to surgery to reduce surgical defect size of all subtypes |
| Photodynamic therapy | Multiple superficial or thin nodular BCCs |
| Radiotherapy | Primary BCCs in those unwilling or unable to undergo surgery; adjuvant therapy post-surgery for remaining positive margins |
| Operative standard excision | Workhorse. Surgical management of BCC, useful for all tumor types in all areas but clearest benefits in nonaggressive primary BCCs in non-high-risk locations |
| MMS | “Gold standard.” Selective application: primary facial morpheaform or infiltrative BCC; recurrent BCC; any BCC in a high-risk location |
| Electrodessication and curettage | Nonaggressive primary BCCs <3 cm in low-risk locations; unable or unwilling to tolerate surgery |
| Pulsed dye laser b | Superficial and nodular BCCs <1.5 cm |
a Can be tried for the off-label use of small nodular BCC.
Nonoperative Management
Topical Therapies
Topical therapies provide a minimally invasive approach to BCC management in specific contexts. The success of this mode of therapy centers on the ability of the topical agent to reach the tumor in its entirety, the tumor response, and the compliance of the patient.
Cryotherapy utilizes liquid nitrogen to destroy superficial basal cell carcinomas. It requires a minimum of two freeze–thaw cycles achieving temperatures of −50°C to destroy the tumor with treatment of a margin of normal tissue to ensure destruction of subclinical extension. This method lacks histological tumor confirmation but cure rates are reported to be over 95%. Care must be taken when treating BCCs near the eye. Adverse outcomes include scarring, hypo- or hyperpigmentation and the possibility of obscuring tumor recurrence by scar tissue. Some have reported greater patient satisfaction with surgical excision compared to cryotherapy due to the superior cosmetic result.
Imiquimod 5% cream is an immune response modifier that increases the T-helper response by inducing interferon-α, tumor necrosis factor-α, and cytokines to destroy dysplastic keratinocytes by acting on Toll-like receptor 7 (TLR7). Although it is only FDA-approved for biopsy-confirmed nonfacial superficial BCCs <2 cm in size, some have shown efficacy in the treatment of nodular BCCs. However, care should be taken with off-label treatment due to reports of recurrences with increased subclinical extension due to selective clearing of superficial tumor. Furthermore, there is significant genetic variation in Toll-like receptors between individuals, with some individuals being unable to respond to imiquimod therapy as a result. Adverse reactions include local skin irritation (the severity may or may not correlate with histological clearance) and hence it should not be applied near the eye. 5-Fluorouracil has also been used for superficial and nodular BCCs. A systematic review found clearance rates of up to 90% for superficial BCCs. However, adverse reactions of erythema, pruritus, and pain limit its use. Imiquimod and 5-fluorouracil treatment should be restricted to small tumors in low-risk locations in patients who will not or cannot undergo treatment with more-established therapies of known long-term clearance rates.
Oral Therapy
The FDA-approved oral Hedgehog pathway inhibitor vismodegib has shown efficacy in the treatment of locally advanced and metastatic BCCs and in reducing the size of existing BCCs and development of new BCCs in those with BCNS. The recent VISMONEO study demonstrated its potential as a neoadjuvant therapy to reduce tumor size or provide a complete response (>50%) prior to surgery for inoperable (or functionally-inoperable) BCCs of all histologic subtypes. However, histologic changes to the tumor with the use of this drug may result in difficulty determining clear margins during Mohs surgery. In addition, the optimal duration of neoadjuvant treatment has not yet been determined as patients underwent surgery once vismodegib-related tumor changes plateaued. Adverse effects are the main limiting factor to continued use of vismodegib, including muscle cramps, hair loss, dysgeusia, weight loss and fatigue. With drug discontinuation the adverse events resolve but tumor regrowth occurs within months. Prolonged use may result in secondary acquired resistance.
Photodynamic Therapy
Photodynamic therapy (PDT) involves the topical application of a photosensitizing agent to the desired treatment area with subsequent activation of the drug by visible light to create reactive oxygen species which destroy neoplastic cells. Topical δ-aminolevulinic acid or methylaminolevulinate produce the photosensitizer protoporphyrin IX semi-selectively within tumor cells. In 2005, an international consensus on the use of PDT for NMSC recommended it as first-line treatment for superficial BCC. It is less effective in nodular BCC subtypes due to the thickness of the tumor limiting absorption of the topical medication into the dermis. Although studies have demonstrated superior cosmetic outcomes of PDT compared to surgical excision, some tumors do not respond to treatment and it is associated with higher recurrence rates than surgery with long-term cure rates for superficial BCC of approximately 75%. Adverse reactions include erythema and pain. The inconvenience of multiple hospital visits makes it unsuitable for some patients. PDT should generally be reserved for those with tumors not amenable to other established-treatment methods or for those with multiple BCCs, such as BCNS patients.
Radiotherapy
Radiation therapy can be used for primary BCCs in those unwilling or unable to undergo surgery or as an adjuvant therapy post surgery for remaining positive margins. Control rates of over 90% have been reported, although there may be potential for aggressive recurrences post treatment. Disadvantages include lack of histologic verification of tumor removal, prolonged treatment course and poor cosmetic outcomes. Radiotherapy is contraindicated in patients with BCNS or xeroderma pigmentosum, as ionizing radiation can induce development of new BCCs within the radiation field.
Operative Management
Significant debate remains as to the most appropriate definitive treatment modality for BCC, especially whether standard surgical excision or Mohs micrographic surgery (MMS) is the most appropriate definitive surgical treatment. The two modalities use different processing techniques to determine margins, which can make direct comparison difficult. Compounding this in the literature is the variable use of clinical versus pathological margins, lack of direct comparison between these modalities in clinical trials and a paucity of appropriate outcome measures and suitable long-term follow-up. One example is the use of incomplete excision to suggest MMS provides better outcomes. Incomplete excision is an uncommon outcome following standard surgical excision using an appropriate margin. In specific instances, further resection may be halted and the defect dressed or skin grafted for definitive reconstruction once surgical clearance has been confirmed, referred to as a delayed reconstruction after pathology evaluation, or DRAPE procedure. This minimizes the loss of important anatomical structures and has been referred to as “slow Mohs.” If incomplete, then further resection is undertaken.
MMS provides the benefit of being able to undertake multiple cycles of resection and microscopic evaluation in real time, but the number of cycles is not generally included in statistics for comparison. While DRAPE procedures may be inconvenient for the patient, this approach provides excellent, cost-effective clearance while preserving important structures to aid the postoperative outcome and retains the histology blocks and sections for future review and additional tests such as immunohistochemistry should an atypical tumor be identified.
Standard Surgical Excision
Surgical excision for basal cell carcinoma produces cure rates in excess of 90%. A meta-analysis (89 studies and 16,000 lesions) identified that a 3-mm clinical margin for non-morpheaform BCC resulted in a cure rate of over 95% for lesions <2 cm in diameter. Incomplete excision in this study was associated with a 27% recurrence rate. While this is somewhat high, incompletely excised lesions often do not show any additional tumor on re-excision and such re-excision usually results in cure in this rarely metastatic tumor. Standard surgical excision is one of the most widely used and reliable approaches to achieve definitive tumor excision with confirmatory histopathology in a relatively cost-effective manner. However, incomplete excision rates for aggressive subtype primary BCCs or recurrent BCCs have been shown to be higher with this method compared to MMS, with over 10% incomplete excision rates in some reported studies. While this may reflect the clinical practice of staged excision/DRAPE, proponents of MMS correctly identify the capacity of MMS to produce equivalent or higher cure rates in a single visit. A wider radial margin (4–5 mm) is typically used for diffuse lesions up to 2 cm in diameter for this reason. This wider margin may increase the defect size relative to MMS with potential significance for esthetically or functionally sensitive areas such as in the central face. Reconstruction of these areas is commonly undertaken as esthetic units for improved postoperative appearance with MMS demonstrating benefit if the excision can be contained within a specific subunit. Standard surgical excision remains the workhorse for definitive BCC excision and is one of the most cost-effective means to manage the millions of BCCs that occur worldwide every year.
Mohs Micrographic Surgery (MMS)
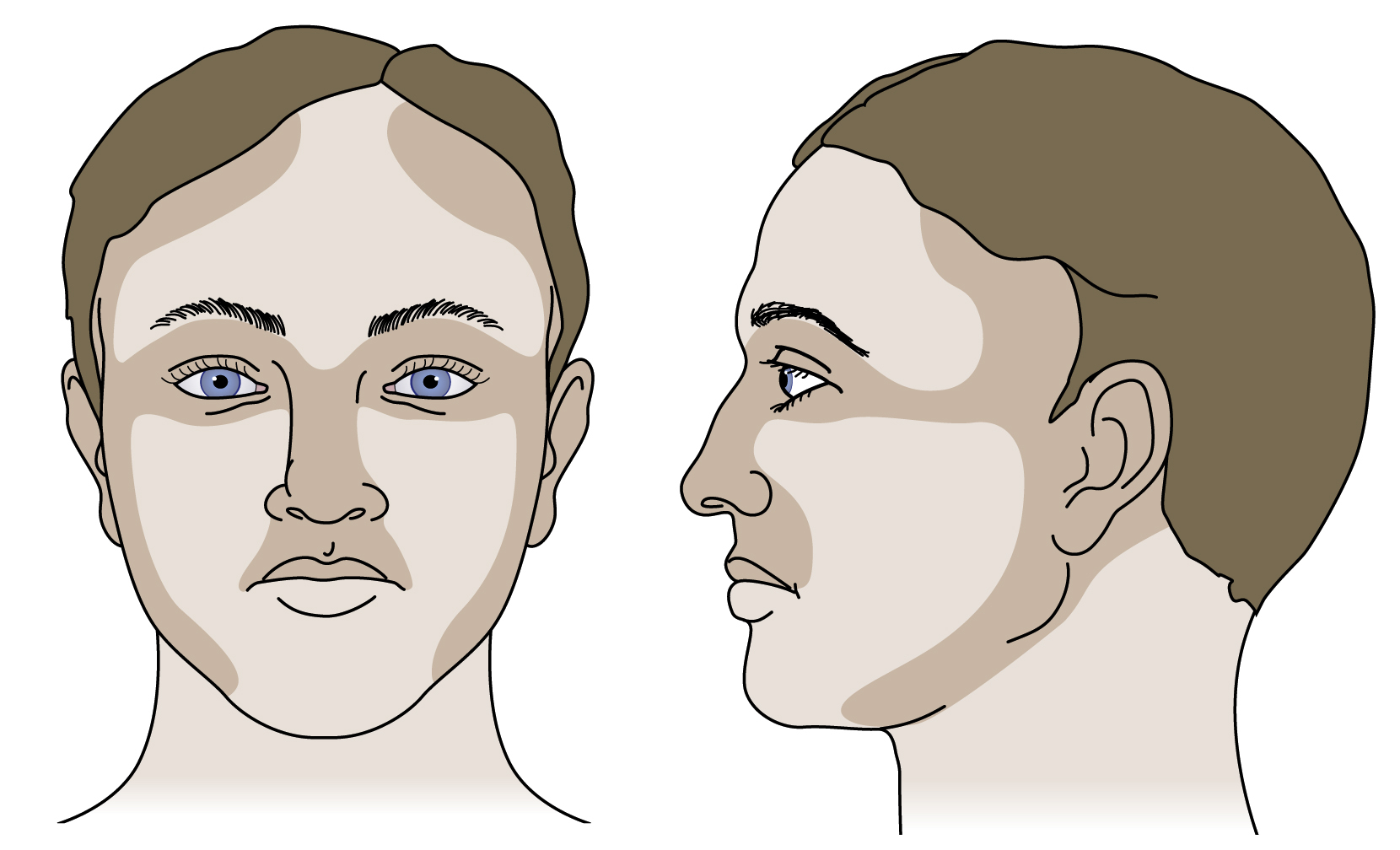
MMS is considered by many as the gold standard in BCC removal by providing equal or higher rates of tumor clearance when compared with other modalities. MMS involves histological analysis of tissue margins and therefore provides tumor clearance with maximal tissue conservation in areas of high risk for recurrence (periorbital, periauricular, and central face, see Fig. 9.3 ), resulting in smaller surgical defects compared to standard surgical excision. Five-year recurrence rates for primary and recurrent BCCs treated by MMS are approximately 1%–2% and 4–7%, respectively. Therefore it is especially useful for primary facial BCCs with aggressive clinicopathologic subtypes (morpheaform or infiltrative), recurrent facial BCCs and any BCC in a high-risk location. The use of MMS to treat the majority of BCCs is probably inappropriate however. The process can be lengthy for the patient and the Mohs practitioner as a number of cycles of excision, processing, and interpretation may be necessary to achieve clearance. The histology slides and blocks are not retained for subsequent review and this can be particularly problematic when an atypical tumor is identified within the lesion, thereby making diagnosis of the mixed tumor difficult. From a health economics perspective, MMS is significantly more expensive than standard excision and for nonrecurrent disease it has not been shown to produce better 5-year outcomes. For these practical reasons, MMS is applied selectively in centers that offer it as a treatment modality. It is likely that formalized criteria for its use will be required into the future as populations age, rates of NMSC increase, and health budgets become tighter.
Electrodessication and Curettage
Electrodessication and curettage is an efficacious and cost-effective treatment modality, however, it is operator-dependent. Its use should be limited to small (<3 cm) non-morpheaform primary BCCs in low–moderate risk locations. Larger (>2 cm) and more aggressive tumors are associated with lower clearance (84%), when compared with the excellent clearance rate (98%) achieved in tumors <1 cm.
Pulsed Dye Laser
Pulsed dye laser (PDL) 595 nm has shown some efficacy for superficial and nodular BCCs. It targets the vascular network of these tumors leading to size reduction and complete regression in some cases. Clearance rates up to 90% with four treatments have been reported for small superficial and nodular BCCs (<1.5 cm). Cure rates were lower with larger tumors. The use of larger spot sizes and double-stacked pulses may allow single treatments to clear BCCs but only a limited number of studies have been performed and the long-term effectiveness is unclear. Adverse events include hypopigmentation and scarring.
Squamous Cell Carcinoma
Epidemiology
Squamous cell carcinoma (SCC) is the second most common type of skin cancer, with an estimated annual incidence of 250,000 cases in the United States. It is the second most common cancer in the Caucasian population. Although less common than BCC, SCC has a greater potential for metastasis and is associated with a higher risk of mortality. Data from skin cancer studies external to national surveys have confirmed a high incidence of SCC at tropical and subtropical latitudes in Australia. According to the Cancer Council of Australia, the overall incidence rate of SCC in Australia is increasing, with an estimated 387 per 100,000 in people aged 14 years and over being affected – more than double the estimated incidence in 1985.
Risk Factors
In patients who received long-term therapy with psoralen and ultraviolet A (PUVA) for psoriasis, there is a 30-fold increased risk of NMSC, particularly SCCs. Additional risk factors include male gender, low Fitzpatrick skin type, albinism, epidermolysis bullosa, human papillomavirus (HPV) infection, smoking, previous ionizing radiotherapy treatment, chronic inflammation and irritation, and chemical carcinogens, such as arsenic and aromatic hydrocarbons. Immunosuppressed individuals, particularly organ transplant patients or those with leukemia and lymphoma, have a significantly increased risk of SCC, mainly in sun-exposed sites, with tumors typically developing 3–7 years after the onset of chronic immunosuppression. One-third of individuals with epidermodysplasia verruciformis develop SCCs due to chronic HPV infection. When SCC develops in an area of chronic inflammation and scarring, it is termed a Marjolin’s ulcer. This diagnosis should be considered in any nonhealing wound as it carries a 50% risk of metastasis. SCC occurs commonly in xeroderma pigmentosum, a rare autosomal recessive genetic disorder characterized with marked hypersensitivity to ultraviolet rays appearing in early childhood. This results in a 10,000-fold increased risk of skin cancer on sun-exposed sites in this population. As such, these SCCs particularly involve the face, head, neck, and scalp.
Genetics
Increasing age and chronic UV exposure, including tanning bed use, are the most significant risk factors for SCC development, with a sharp increase in incidence over the age of 40. Approximately 90% of SCCs and over 75% of actinic keratoses have inactivation of the tumor suppressor gene p53 secondary to UV damage. p53 usually induces apoptosis of UV-damaged cells, thus preventing the development of dysplastic keratinocytes.
Mutational profiling of cutaneous SCC has evolved over the past decade in an effort to understand SCC biology and thus identify molecular targets for novel therapeutics. Mutations involving the family of Ras proto-oncogenes, which are commonly implicated in a variety of tumors, are one of the more common targets of therapy, specifically, HRAS and KRAS . Others include TP53 , CDKN2A , PIK3CA , MYC , FGFR3 , and VHL . Of note, the use of Raf inhibitors in melanoma patients has resulted in the development of cutaneous SCC with a strong association with Ras mutations and epidermal growth factor receptor (EGFR) mutations are present in over half of all aggressive SCC.
Pathogenesis
Squamous cell carcinoma is a malignant neoplasm of suprabasal epidermal keratinocytes with full-thickness epidermal dysplasia. These may arise de novo or from precursor lesions such as actinic keratosis (AK), which have partial-thickness epidermal dysplasia. AKs are not considered to be a premalignant lesion, but rather as an important sign of UV-induced photo-damage that signals an increased risk of NMSC. Their estimated progression rate from AK to SCC is 0.025%–16% per year.
Bowen’s disease is the eponymous name for squamous cell carcinoma in situ (SCCIS) and once the dysplastic keratinocytes have invaded the basement membrane, it becomes an invasive SCC. Although less common than BCCs, SCCs carry a risk of metastasis and death. Despite the rising incidence of SCC, there is a 20% reduction in mortality due to increased public awareness and more aggressive treatment of highly invasive tumors.
Clinical Presentation and Classification
Clinical Presentation
SCCs typically arise in sun-exposed sites, namely the head, neck, ears, dorsal hands, lips, and legs. The head and neck are the most common sites of occurrence for SCC in men, while the upper limbs followed by head and neck are the most common sites in females. In those with higher Fitzpatrick skin types, they may arise on both sun-exposed and protected sites. SCCs usually present as a changing solitary lesion developing from a pre-existing AK or Bowen’s disease. AKs ( Fig. 9.6A ) appear as multiple ill-defined scaly erythematous macules, papules or plaques ranging in size from 2 mm to >2 cm, whereas Bowen’s disease ( Fig. 9.6B ) is usually a well-defined solitary patch/plaque. Both of these precursor lesions can be confused with eczema or psoriasis, however they are typically asymptomatic and do not respond to topical steroids. The development of tenderness, increased size or scale and erosions may represent progression to SCC. In the setting of immunosuppression, multiple SCCs may develop in an eruptive fashion.











