I. FACTORS AFFECTING FACIAL AGING
A. Chronic sun exposure
1. Ultraviolet (UV) radiation causes DNA damage and production of free radicals resulting in collagen and elastin damage, diminished dermal robustness, loss of skin elasticity, and increased risk for development of skin cancers
2. Elastic fibers rearrange in abnormal distribution
3. Overall decrease in collagen fibers
4. Creates fine rhytids and skin laxity
B. Chronologic aging
1. Diminished collagen and elastin deposition with increasingly disorganized structure
2. Fewer fibroblasts and diminished supply of blood
3. Fewer elastic fibers
4. Thinning of the dermis due to these effects ultimately results in the development of wrinkles
5. Aging is related with time-dependent exposure to gravity, which results in the development of deep rhytids
6. Sebaceous glands produce less oil resulting in decreased skin moisture
7. The subcutaneous fat thins, resulting in a more hollowed appearance
C. Other exposures
1. Cigarette smoke results in fine rhytids secondary to local irritants from smoke and systemic hypoxia. Cigarette smoke induces production of matrix metalloproteinases and inhibits procollagen synthesis through its effects on transforming growth factor beta.
2. Radiation therapy can induce DNA damage and free radical production similar to UV light.
3. Weight gain can result in dermal thinning, which is persistent and can be prominent in patients who have subsequently lost this weight. The result is excess skin with little support and the development of fine and deep rhytids.
II. STIGMATA
A. Rhytids
1. Fine rhytids are caused by facial muscle forces and chronic changes in dermis described above
2. Deep rhytids are caused by the effects of gravity pulling soft tissues downward against fixed structures, such as retaining ligaments.
B. Dyschromia
1. Changes in the coloration of the skin
2. In older patients, the number of melanocytes decreases causing the skin to appear pale. However, the remaining melanocytes increase in size resulting in patchy appearance and development of pigmented spots.
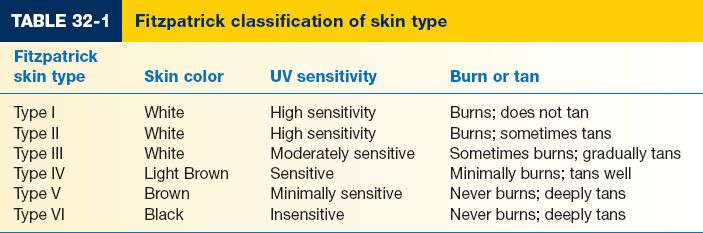
III. FITZPATRICK SKIN TYPE CLASSIFICATION
A. Higher Fitzpatrick have higher resistance to photoaging (Table 32-1)
______________
*Denotes common in-service examination topics
1. Describes skin types in relation to skin color, sensitivity to UV light, and whether the skin type characteristically burns or tans with sun exposure.
2. Photoaging refers to the changes associated with UV exposure (see above).
IV. CHEMICAL PEELS
A. Background
1. Chemically induced injury to epidermis and superficial dermis (Fig. 32-1)
2. Healing via epithelial advancement from skin appendages
a. Epidermal regeneration begins at 48 hours and is complete by 7 days
i. Cellular uniformity, columnar shape (vertical polarity), mild increase in the number of melanocytes, decrease in the amount of melanin granules in basal layer of epidermis
b. Collagen deposition in the dermis begins 2 weeks after peel application; this effect lasts up to 1 year. Homogenization of dermal collagen, dense parallel collagen bundles.
B. Pretreatment
1. Generally, pretreatment is indicated in patients undergoing medium (trichloroacetic acid) or deep (phenol) peels.
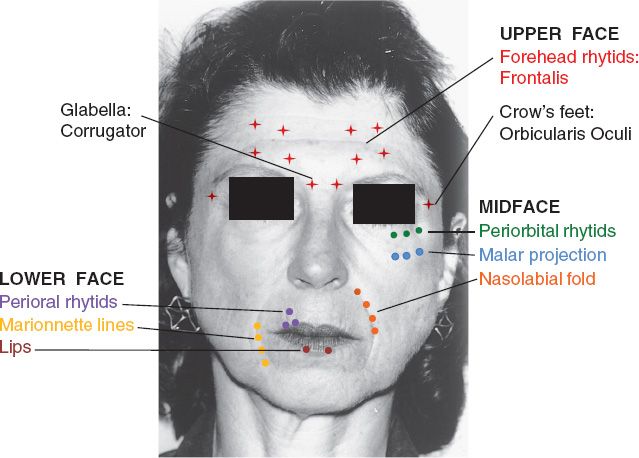
Figure 32-1. Common injection sites for Botox (crosses) and fillers (circles). (Adapted from Mulholland MW, ed. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
2. Use of pretreatment is variable but may be performed with tretinoin and/or hydroquinone (4%) at some institutions starting 2 weeks to 3 months prior to performing peel.
a. Tretinoin
i. Stimulates papillary dermal collagen synthesis and angiogenesis.
ii. Enhances basement membrane structure by inducing increased deposition of glycosaminoglycans.
iii. Increases depth of penetration of actual peel by exfoliating the stratum corneum.
b. Hydroquinone
i. Tyrosinase inhibitor
a) Blocks tyrisonase (enzyme that produces melanin)
b) Helps prevent post-peel hyperpigmentation
3. May also pretreat with keratinolytics such as Jessner solution, salicylic acid, lactic acid, and resorcinol.
C. Pre-peel set up
1. The patient cleans their skin, removing all makeup the night before peel.
2. Clean and degrease skin with soap and acetone or isopropyl alcohol immediately prior to application.
3. Use sedation for full-face peel.
4. Sterile water for eye irrigation if eye exposed
5. Patients with a history of herpes require acyclovir prophylaxis prior to and for up to 5 days after peel is performed.
D. Factors to change depth of penetration
1. Peeling agent characteristics
a. Concentration
b. Type of formula
c. Storage and age of acid
2. Skin preparation
a. Degreasing
b. Skin cleansing
c. Abrasion
3. Method of application
a. Number of coats
b. Occlusion
E. Superficial peel
1. Affects upper epidermis
2. Use for mild dyschromia
3. Alpha hydroxy acid (AHA) peel
a. Primarily used as exfoliant
b. May include acids such as lactic acid, glycolic acid, tartaric acid, or malic acid
c. Advantages
i. May be used as pretreatment for peels/laser therapy
ii. May help decrease the risk of post-laser hyperpigmentation by “down-regulating” melanocytes
d. Disadvantages
i. Multiple treatment sessions are required for maximum benefit
ii. Does not address deep wrinkling
e. Indications
i. Fine wrinkles, dry skin, mildly irregular pigmented ares
f. Mechanism
i. Concentrations ranging from 30% to 70%
ii. Lower concentrations decrease keratinocyte cohesion
iii. Higher concentration cause epidermolysis
g. Application
i. AHAs are often simply combined with mild facial creams or cleansers and applied according to the manufacturer’s directions
h. Tretinoin can be used to increase depth of penetration and accelerate wound healing
a. Similar to AHA in effect of depth
b. Advantages
i. Also a mild peel
ii. Not likely to injure from overtreatment
c. Disadvantages
i. Like AHA peels, does not address deep wrinkles
b. Mechanism
i. Consists of resorcinol (14 g), salicylic acid (14 g), lactic acid (14 cc), and ethanol (1000 cc)
ii. May disrupt cohesion of keratinocytes’ cell-cell linkages
c. Application
i. Number of applications determines depth of penetration
d. Can be used as pretreatment for trichloroacetic acid (TCA) peel
5. Salicylic acid
a. Advantages
i. Compared to other acids, there is decreased pain/erythema
ii. Very safe / low toxicity
iii. Safer for most Fitzpatrick skin types than other peels
b. Disadvantages
i. Contraindicated in patients with aspirin sensitivity
c. Mechanism
i. As a keratolytic agent, salicylic acid, like AHAs, reduces contact between keratinocytes
d. Application
i. Kits are available in varying concentrations (2–30%)
ii. salicyclic acid is applied to the face and the precipitate forms a white “pseudofrost”
iii. May repeat after a few weeks
F. Medium depth peel
1. TCA
a. Derivative of acetic acid
b. TCA peels can be medium or deep depending on the concentration used
c. Advantages
i. Low risk for systemic toxicity
ii. Does not require cardiac monitoring (unlike phenol peel)
iii. Decreased risk for hypopigmentation as compared with deeper peels
iv. Neutralized by dermis.
d. Disadvantages
i. When compared with deeper peels, medium depth TCA peels have half the neocollagen formation and half the dermis penetration.
ii. As a result, they are less effective on coarse wrinkles or sun-damaged skin.
iii. Can cause hyperpigmentation.
e. Mechanism
i. Causes protein denaturation and cell death resulting in coagulative necrosis.
ii. Over 5 to 7 days, the epidermis and superficial dermis will slough.
f. Application
i. Wash/degrease the skin with acetone or isopropyl alcohol
ii. Stretch skin to remove wrinkles
iii. Some advocate applying Jessner’s solution prior to applying the TCA peel in order to increase penetration. Retin-A may also be applied to increase depth of penetration by causing dekeratinization.
iv. Apply TCA peel at concentration ranging from 20% to 35%. Concentration determines depth of peel. 10% to 25% concentration will yield a light peel with epidermal penetration only. 30% to 35% concentration will yield an intermediate peel with penetration into the papillary dermis. 45% to 55% concentration has a higher risk of scarring.
v. Erythema indicates superficial depth of effect. Pink-white frosted skin indicates intermediate depth of effect. Uniform, dense, white-colored frosted skin indicates a deeper depth of effect. Finally, a grayish-white color indicates an effect that is too deep.
g. Post-medium peel care
i. The patient is instructed to use ointment to the treated area (such as bacitracin, petrolatum, lidocaine jelly, or a mixture).
ii. At 48 hours, expect desquamation of the coagulated epithelium (brown color)
a) May use moisturizer or hydrocortisone-based cream
b) Peaks at 72 hours
c) No makeup
iii. At 4 to 7 days, skin is healing and peeling. Wash face several times per day and may resume makeup after peeling is completed.
iv. At 7 to 10 days, start tretinoin and hydroquinone after peeling has stopped. Use sunscreen to avoid hyperpigmentation.
v. Wait 3 months prior to additional peels.
G. Deep peel
1. Phenol
a. Baker–Gordon peel
i. 3 cc phenol
ii. 2 cc tap water
iii. Eight drops liquid soap
iv. Three drops croton oil—vesicant that enhances keratolytic and penetrating action. It is believed that the croton oil is the active ingredient, not the phenol.
v. Number of coats does not affect depth of penetration as in TCA peels.
b. Advantages
i. Long-lasting results, safe, and effective
a) Causes rapid denaturation/coagulation of keratin
ii. Controlled partial-thickness chemical burn with depth of penetration to upper reticular dermis
iii. Hypertrophic scarring is rare
c. Disadvantages
i. Most patients experience redness for two months, but are able to go back to work at two weeks
ii. Potential for significant hypopigmentation
iii. Requires continuous EKG, pulse oximetry, IV access due to risk of cardiac dysrhythmia.
iv. Metabolized by the liver.
d. Indications
i. Coarse wrinkles, perioral rhytids
ii. Facial hyperpigmentation
iii. Actinic keratoses
iv. Lentigines on hands or fingers
e. Patient selection
i. Good for type I–III skin (less risk of hypopigmentation)
ii. Not suitable for acne, telangiectasia, and skin grafts
iii. Contraindicated in patients with cardiac disease
f. Mechanism
i. Penetrates into papillary dermis
ii. New collagen is deposited in the dermis in compact, parallel bundles, resulting in improved skin extensibility
iii. Early changes: Keratocoagulation necrosis of epidermis into papillary dermis
iv. 48 hours: Epidermal regeneration, complete within 7 days
v. At 3 months, healing is complete
i. Absorbed through skin, metabolized by liver, renally excreted
ii. High risk for cardiac dysrhythmia if >50% of face resurfaced in <30 minutes. For large areas, take 15-minute breaks between subunits or apply slowly over 1 hour.
h. Application
i. Damp cotton swab
ii. On eyelids, use almost dry cotton swab to avoid conjunctival contact. Swab to upper border of tarsal plate on superior eyelid and within 3 mm of lower lid margin to avoid eyelid edema.
iii. Will turn skin frosty gray-white color immediately.
iv. Patient will experience burning until phenol anesthetic activity kicks in. May consider sedation and/or local anesthetic to avoid burning sensation.
v. Apply over 1 to 2 hours to avoid cardiac dysrhythmia.
vi. Stop below mandibular border so that transition is not as obvious.
i. Post-deep peel care
i. Prophylactic antibiotics for 7 days
ii. Anti-viral herpes therapy if history of herpes infection
iii. May apply occlusive dressing for 24 hours, which allows for deeper penetration.
iv. Eyes may swell for 48 hours
v. Wash face with peroxide/water and apply petroleum jelly
vi. Makeup can be used within 10 to 15 days
vii. Sunscreen in 12 to 14 days
viii. Avoid sun exposure
H. Complications
1. Infection
a. Viral: Herpes prophylaxis for peels in individuals with a history of herpes
b. Bacterial: Rare, requires prompt diagnosis and treatment to limit scarring caused by inflammation
2. Scarring
a. Do not resurface people with keloid scar history due to risk of abnormal scarring
b. Constant moisturizing fosters re-epithelization and decreases healing time
3. Pigmentary changes
a. Hyperpigmentation (usually transient) versus hypopigmentation (may be permanent)
4. Milia. Keratin-filled epidermal inclusion cysts
V. LASERS IN AESTHETIC SURGERY
A. Background (see Chapter 10)
B. Ablative lasers
1. Vaporizes the superficial epidermal tissue and coagulates deeper tissues.
2. Proliferation of progenitor cells in hair follicles and sweat glands (adnexal structures) results in re-epithelization.
3. Increased collagen synthesis
a. Type I collagen deposition in subepidermal layer of papillary dermis, known as the Zone of Grenz.
b. Heat-induced collagen contraction.
c. Reorientation of disorganized collagen fibers.
4. Reorganization of elastic fibers to become parallel and more bundled
5. Contraindications
a. Active infection (viral, bacterial, or fungal)
b. *Isotretinoin use in previous 12 months
6. CO2 laser
a. 10,600 nm wavelength
b. *Water is the chromophore
i. Number of passes and cooling time
ii. Deeper thermal heating compared with erbium laser
d. Greatest effect in papillary dermis: Upon healing, disorganized collagen is replaced with normal, compact collagen bundles, which are parallel to the skin
e. Re-epithelialization after 8 to 10 days
f. Fractional photothermolysis devices:
i. Create columns of thermally denatured collagen with islands of intact dermal and epidermal cells.
ii. Uninjured interstices thought to allow for greater tissue regeneration.
g. Side effects
i. Hypopigmentation
a) Most pronounced in Fitzpatrick I/II (opposite from chemical peels)
ii. Erythema for 2 to 4 months after use
iii. Hyperpigmentation
iv. Milia
v. Acne
vi. Infection: Bacterial, viral, or fungal
vii. Hypertrophic scarring
viii. Ectropion
7. Erbium:yttrium–aluminum–garnet (Er:YAG)
a. Rarely used compared to CO2 laser
b. Not as effective at continued collagen remodeling as CO2 laser
c. Does have shorter recovery time than CO2 laser
d. 2,940 nm wavelength
e. *Water is the chromophore
f. Energy absorbed more efficiently and less thermal diffusion than with CO2 laser
g. Depth of penetration, inflammation, and collagen remodeling is less than CO2
h. Useful for thin skin (dorsum of hand, tip of nose)
i. Useful for superficial, fine wrinkles. Need more passes to get deeper effect.
j. Does not coagulate vessels due to less thermal damage. May result in bleeding when encountering larger vessels
C. Nonablative
1. ND: YAG
a. Wavelength: 1064 nm
b. Energy nonspecifically absorbed by target tissue
c. *Targets: Blood vessels, red blood cells, collagen, and melanin
d. Secondary target: Water
e. Greatest effect 1 to 2 mm below skin in dermis
f. Epidermis not ablated
g. 1,320 nm Nd:YAG which targets dermal water also used for nonablative facial rejuvenation
h. Overall Nd:YAG less blistering but less dramatic effect than ablative lasers for facial resurfacing.
D. Post-laser care
1. Most wound environment with lipid-based ointment
2. Valacyclovir or acyclovir for 1 week to prevent herpes simplex activation
3. Hydroquinone and sunscreen to prevent hyperpigmentation
E. Intense pulsed light (IPL)
1. Not a laser
2. Emits photons in the range of 500 to 1,300 nm
3. 550 to 580 nm: Water and hemoglobin
4. 550 to 570 nm: Superficial pigment
5. 590 to 755 nm: Deep pigment
6. Indications: Hypervascularity, telangiectasias or rosacea, solar lentigines, melisma or freckling
7. Contraindications: Isotretinoin, pregnancy, Fitzpatrick VI, and photosensitizing medications
8. Side effects: Redness, scabbing, edema, purpura, hyperpigmentation or hypopigmentation, herpes activation, and scarring
9. Series of four to seven treatments needed
10. Can pretreat with retinoids or hydroquinone
VI. DERMABRASION AND MICRODERMABRASION
A. Dermabrasion
1. Background
a. Method of mechanical abrasion of the epidermis and superficial dermis resulting in improved skin contour and quality.
b. Facial skin is excellent surface for dermabrasion due to increased healing potential from the existence of an abundant vascular network as well as ample adnexal structures.
2. Indications
a. Most commonly used to improve scars from acne.
b. Traumatic scars
c. Perioral and periorbital rhytids
d. Telangiectasia, actinic keratoses, pigmented nevi, and rhinophyma
e. Dermabrasion good choice if deformity is not deeper than dermis
f. Fitzpatrick skin types I and II are best candidates; skin types III and above have a higher risk of dyspigmentation
g. Patients with darker skin who undergo dermabrasion may be given a prescription for topical hydroquinone to reduce the risk of hyperpigmentation.
3. Contraindications
a. Recent or current history of isotretinoin
b. Current outbreak of herpes should not undergo dermabrasion for at least 6 to 8 weeks until after the infection is dormant
c. Patients with a history of herpes should be given acyclovir pre- and post-procedure for up to 2 weeks to reduce the risk of outbreak.
d. History of hypertrophic or keloid scarring
e. Patients with coagulation disorders or taking anticoagulants
4. Pre-procedure preparation
a. Topical tretinoin for up to 1 to 2 months prior
b. Council against direct sunlight for 2 months prior to treatment
c. This procedure involves the removal of living tissue and is therefore painful. Patients require anesthesia which may consist of topical anesthetic cream, IV sedation, regional nerve blocks, and tumescent anesthesia.
d. An ice-pack may be applied to the face 20 to 30 minutes prior to dermabrasion to constrict capillaries and reduce bleeding, and increase the rigidity of skin to assist with procedure.
e. Skin is cleaned with topical antiseptic immediately prior to dermabrasion.
5. Technique
a. Handheld devices such as a rotating wire brush or burr may be used for dermabrasion.
b. Rotational speed of handheld device determines power of the dermabrasion. Increased speed decreases the amount of pressure required to achieve the same depth of dermabrasion.
c. Taut skin surface must be maintained in order to maintain control during the entire procedure. Otherwise, the rotatory device may catch and even tear the skin.
d. Procedure may be performed by holding device at 45 degrees to the skin and dermabrading the area in parallel rows.
e. Following this, one may then dermabrade in an orientation perpendicular to the first set of parallel rows.
f. *Pinpoint bleeding indicates penetration into the superficial papillary dermis and represents a safe endpoint
g. Depth controlled by
ii. Speed of rotation
iii. Coarseness of tip
iv. Length of treatment
v. Patient skin type and texture
6. Post-procedure
a. May apply antibiotic ointment and dressing over the treated area. Dressing may be an occlusive dressing.
b. Skin re-epithelializes in 7 to 10 days
c. Redness will persist for up to 2 to 3 weeks after the procedure.
d. Collagen remodeling occurs over the next 3 to 6 months.
f. Avoid sun exposure to reduce risk of skin hyperpigmentation.
7. Complications
a. Uneven pressure or uneven skin tension may result in streaky or blotchy outcome
b. Abrasion of subcutaneous fat may result in scarring due to dermal discontinuity. Dermis should be re-approximated with suture if subcutaneous fat is entered by the device.
c. Milia formation may occur
d. Hypopigmentation
B. Microdermabrasion
1. Background
a. Noninvasive method of mechanical rejuvenation which does not require the oversight of a physician.
b. Resurfaces photoaged and damaged skin with inert crystal particles (aluminum oxide or sodium chloride) which cause superficial ablation of the epidermal stratum corneum.
2. Indications
a. Patients who hope to improve the tone and texture of already healthy skin.
b. May also be used to correct photodamage, superficial rhytids, actinic keratoses, stretch marks, and shallow acne scars.
3. Contraindications
a. Recent or current history of isotretinoin
b. Facial surgery within the past 2 months
c. History of radiation therapy to the head/face
d. Hypertrophic scarring
e. Bacterial or viral infections of the skin
f. Rosacea and telangiectasias
4. Pre-procedure preparation
a. No need for anesthetic prior to treatment due to only mild discomfort.
b. May give an over-the-counter analgesic prior to procedure.
c. Remove all makeup from skin; wipe oily skin with 70% alcohol solution.
5. Technique
a. Electric vacuum pump sprays inert crystals onto skin and uses suction to remove crystals and associated skin debris.
b. The kinetic energy of the inert crystals sprayed onto the skin removes and dislodges the debris from the stratum corneum.
c. Depth altered by particle flow rate and strength of suction.
d. Perform bimonthly
6. Post-procedure
a. Apply sunscreen to skin and avoid sun exposure for at least 24 hours
7. Complications
a. Extremely rare due to superficial nature of procedure
b. Prolonged erythema may occur
VII. BOTULINUM TOXIN
A. Mechanism
1. Protein naturally produced by bacteria Clostridium botulinum (botulism)
2. *Toxin consists of two parts—heavy chain (binds protein to surface of presynatpic axon terminals) and light chain (translocated across cell membrane, prevents release of acetylcholine at neuromuscular junction)
3. Function restored in 2 to 6 months after new axon terminals sprout and replace deactivated end plates
B. Indications: FDA approved for glabellar frown lines, hyperhidrosis, migraines, and urinary incontinence.
C. Serotypes
1. There are seven different serotypes of the toxin, A–G
2. Type A
a. The most commonly used and most potent
b. FDA approved for glabellar frown lines and hyperhidrosis.
3. Type B
a. Less potent
b. Approved for cervical dystonia
D. Commercially available toxins
1. Botox (onabotulinumtoxinA, type A)
a. Comes in bottle with 100 units
b. Reconstitute in 2.5 to 4 cc to make 2.5 to 4 units/0.1 cc
c. Lethal dose 2,700 units in 70 kg human
d. Once reconstitute should not be any particulate matter
e. Recommend using within 4 units of reconstitution
2. Dysport (abobotulinumtoxinA, type A)
3. Xeomin (incobotulinumtoxinA, type A)
4. Myobloc (rimabotulinumtoxinB, type B)
E. Dose preparation
1. Expressed in mouse units (U). 1 U is the amount that kills 50% of Swiss Webster mice when injected into the intraperitoneal cavity.
2. Relative units: 1 U Botox = 1 U Xeomin = 2 to 3 U Dysport = 50 to 100 U Myobloc
3. Botox/Dysport: Typically diluted 2.5 mL of saline per vial, range 1 to 5 mL; must be refrigerated.
4. Xeomin: Typically diluted 2.5 mL of saline per vial, range 1 to 5 mL; may be stored at room temperature prior to reconstitution.
F. Effect
1. 3 to 6 day latency period until maximal effect (Dysport may have slightly faster onset than Botox).
2. Paralysis lasts 2 to 6 months.
3. Reinjection 2 to 3 months after initial treatment for maintenance
G. Contraindications
1. Disorders of neuromuscular transmission—myasthenia gravis, Lambert–Eaton syndrome, multiple sclerosis, amyotrophic lateral sclerosis.
2. Women who are pregnant or breastfeeding.
3. Patients with allergies to albumin, milk or other ingredients in the formulation.
4. Concomitant use of aminoglycosides and calcium channel blockers can potentiate toxin effects.
5. Do not inject near sites of active infection
H. Complications
1. Bruising: Discontinue anti-inflammatory agents 1 week before injection; avoid prominent veins when injecting; apply pressure and ice after injection.
2. Eyelid ptosis: Avoid injecting too deep as the toxin may penetrate the orbital septum and paralyze the levator palpebrae muscle.
3. Diplopia: Iatrogenic effect on the extraocular muscles—inject outside the orbital rim and avoid deep injection which can lead to oblique or recti muscle paralysis.
4. Pain: Greater pain associated with injection of Type B.
I. Antibody formation
1. Occurs in 5% to 15% of patients receiving repeated injections, leading to reduced toxin effectiveness.
2. Risk increased with receiving more than 200 units in a session or repeat injection within 1 month of treatment; generally wait at least 12 weeks between repeat injections.
J. Clinical uses
1. Wrinkles or rhytides are produced by the baseline contraction of underlying muscles.
2. With aging, ridges or wrinkles appear perpendicular to the muscle fibers.
3. Chemical paresis created by botulinum toxin eliminates muscle contraction, thus decreasing dynamic wrinkles and furrows.
K. Treatment Locations (Fig. 32-1)
1. Forehead: Horizontal lines
a. Target: Frontalis
b. 4 to 6 injection points in the occipitofrontalis muscle in the middle of the forehead, 2 to 3 cm above the orbital rims.
c. 10 to 30 U total
d. Direct injections more medial in women to allow greater lateral eyebrow elevation.
e. Avoid low lateral brow injections to prevent ptosis.
2. Glabella
a. *Target: Corrugator supercilii, procerus, and orbicularis oculi muscles (brow depressors).
b. 3 to 7 injection points, one for procerus, one for each corrugator, consider additional injections laterally on each side with a total of 20 to 40 U
c. All injections should be placed outside of the orbital rim to avoid paralysis of the levator palpebrae superioris.
3. Crow’s feet and lower eyelid
a. Target: Orbital, palpebral, and lacrimal portions of orbicularis oculi.
b. Typically 3 to 5 injection sites above zygomatic arch.
c. 6 to 12 U per side are placed approximately 1 cm lateral to the orbital rim to treat crow’s feet.
d. The lower eyelid is treated with 1 to 2 injections using a total of 1 to 2 U per side infraorbital in the midpupillary line.
e. A snap test of the lower lids should be performed prior to treatment, and if sluggish, lower eyelid injection should be avoided as this may lead to ectropion.
f. Avoid injecting the zygomaticus muscle as this may lead to cheek ptosis and lip asymmetry.
4. Bunny lines
a. Target: Nasalis and procerus
b. Wrinkles that develop on the lateral or dorsal portion of the nose and are primarily
c. Typically one injection is given on each side
d. A total of 2 to 5 U; an additional dorsal injection of 1 to 2 U may also be used
e. Avoid deep injection which causes bruising.
f. Avoid levator labii superioris alaeque nasi and levator labii superioris which will cause external nasal valve collapse.
5. Nasolabial folds
a. This area is primarily treated with dermal fillers but botulinum toxin may be used in conjunction.
b. Muscles contributing to the nasolabial fold include the levator labii superioris alaeque nasi, levator labii superioris, zygomaticus minor, zygomaticus major, and levator anguli oris.
c. The levator labii superioris is the primary target of injection.
d. A single injection of 1 to 3 U is given per side.
6. Perioral wrinkles
a. Target: Orbicularis oris muscle
b. Fine lines of the upper lip can be treated with 2 to 4 injections either limited to the philtrum area or placed along the upper lip within 5 mm of the ver-million border with a total of 1 to 2.5 U per side.
c. Treatment should be limited and lateral injections should be avoided to prevent drooling.
d. Dermal fillers are often used in conjuction
e. Avoid use in patients whose profession relies on fine lip movement such as singers, public speakers, and musicians who play wind instruments
f. Stay within 5 mm of vermilion border
7. Marionette lines
a. The depressor anguli oris muscle draws down the corner of the mouth in conjunction with fibers of the platysma, creating these folds.
b. Two injections are given per side
i. One targeting the depressor anguli oris at least 1 cm away from the mouth.
ii. Second injection more laterally to treat the platysmal bands, for a total of up to 5 U per side
8. Cobblestone chin
a. Target: Mentalis muscle
b. 1 to 3 injection points 0.5 to 1 cm above the chin
c. 2 to 8 U
d. Avoid injection of orbicularis oris by staying low
9. Platysmal bands
a. Target: Platysma
b. Ideal candidates have good skin elasticity and minimal fat deposits
c. 4 to 8 injection points per band, approximately 1 cm apart
d. 2 to 2.5 U per injection
VIII. INJECTABLES
A. Background
1. Beginning with FDA approval of bovine collagen in 1981, a variety of types and brands of dermal fillers have become available, ranging from relatively short acting biologics to nonabsorbable, synthetic materials, as well as autologous injectables
2. Autologous materials include fat, platelet-rich plasma, collagen, fascia, and fibroblasts
3. Biological materials include collagen and hyaluronic acid
4. Synthetic materials include polylactic acid (PLLA), calcium hydroxylapatite, and polymethylmethacrylate (PMMA)
B. Absorbable
1. Autologous fat injection (See Chapter 9 on Fat Grafting)
a. Harvested by liposuction, processed with centrifugation to isolate fat cells.
b. Can be injected into many areas of the face to enhance subcutaneous volume, including the temporal region, infraorbital hollows, malar region, nasolabial folds, and chin, and to fill depressed scars.
c. Overfilling typically performed due to resorption.
d. Degree of fat survival is technique dependent, typically 40% to 80%.
2. Platelet-rich plasma
a. Autologous blood plasma containing concentrated platelets and growth factors prepared from patient’s whole blood.
b. Platelets are activated by the addition of calcium and release a variety of growth factors, cytokines, and chemokines that stimulate collagen production and tissue growth.
c. Typically requires two to three treatments one month apart, several weeks for results to appear.
d. Effects have 6 to 12 month duration, retreatment often performed every 6 months.
3. Collagen
a. Bovine origin: Zyderm, Zyplast
b. Porcine origin: Evolence
c. Human origin: CosmoDerm, CosmoPlast
d. FDA approved to treat fine-to-deep facial wrinkles and folds and acne scars
e. Injected typically into the superficial or middle dermis to treat fine-to-medium lines and soft scars.
f. Deeper rhytids and nasolabial folds may be treated by injection into the middle-to-deep dermis.
g. May also be used for lip augmentation or to enhance definition of the vermilion border.
h. Deeper wrinkles require more material often with short-lived results.
i. Overfilling typically performed due to resorption.
j. 2 to 6 month duration
k. *Allergy skin testing for hypersensitivity reaction performed prior to use of bovine collagen
i. A test dose is administered and the skin site is observed for 48 hours
ii. A second dose is given 2 weeks later, and observed for 2 weeks, prior to treatment.
iii. Observe site for swelling, erythema, induration, and pruritis.
l. Technique
m. Lip Augmentation Technique
i. Lip augmentation can be performed either at the vermilion border or within the muscle. Formulations continue to vary, but in principle, the deficient area can be filled effectively with a variety of techniques.
ii. A fanning technique may be used with a single entry at each oral commis-sure, depositing agent along the entire body of the lip using three passes.
iii. Puncture techniques may be used to add volume to the central lip.
n. Nasolabial fold effacement technique
i. A “threading” technique is used in which multiple passes are used to inject the product into the nasolabial fold
ii. It is important to retain part of the nasolabial fold and not efface all of it
iii. The correct should last about 6–9 months
o. Glabellar folds/scars/other hollow areas
i. Linear threading technique is used, or, for focal wrinkles, a puncture may be used to deposit more product
ii. After injection, massage may be used to partly disperse the product
4. Hyaluronic acid
a. Brands: Restylane, Perlane, Captique, Hylaform, and Juvéderm
b. Hydrophilic glycosaminoglycan synthesized by Streptococcus spp. or derived from rooster comb.
c. Cross-linking improves duration of effect by resisting degradation
d. FDA approved to treat moderate-to-severe facial wrinkles and folds
e. Small particle sizes
i. Restylane Fine Lines, Juvederm 18, and Hylaform Fine Lines
ii. Inject into the superficial dermis or dermal epidermal junction to treat fine lines
f. Intermediate particle sizes
i. Restylane, Juvederm 24, and Hylaform
ii. Inject into middle dermis to treat moderate wrinkles
g. Larger particle
i. Perlane, Juvederm 30, and Hylaform Plus
ii. Inject into the deep dermis to treat more pronounced wrinkles and folds
h. May be used for lip augmentation, often in conjunction with collagen or hyaluronic acid to enhance the vermilion border. Should be injected within vermillion and not above the vermillion to avoid shortening the lip.
i. Higher concentration gels absorb more water and swell more following injection, and care must be taken to avoid over correction
j. 6 to 12 month duration
k. Low risk of immune reaction
l. In the case of an undesired outcome or concern for injection necrosis, hyaluronidase can be injected to break down the hyaluronic acid.
a. Brand: Sculptra
b. Synthetic biodegradable lactic acid polymer prepared as microparticles suspended in a cellulose matrix.
c. Reconstitute in 3 to 5 cc of sterile water 2 hours before injection
d. FDA approved to treat nasolabial folds and deep facial wrinkles
e. Injected into the deep dermal or subcutaneous layers.
f. Volume enhancement effect occurs through fibroblast stimulation of collagen synthesis and replacement of degraded PLLA.
g. Results may not appear for at least 4 weeks, and two to five treatments at least 4 to 6 weeks apart are typically needed.
h. 2+ years duration and degrades and is replaced with collagen.
i. Immunologically inert, sensitivity testing is not required.
j. Delayed appearance of palpable but nonvisible subcutaneous nodules may occur, as well as granuloma formation.
k. *Approved for HIV lipoatrophy
i. Inframalar hollow
ii. Concavities adjacent to zygomatic bone
iii. Zygomatic arch
l. Must be injected deep (deep dermis or periosteum), therefore, do not use in perioral, periorbital, and superficial regions
6. Calcium hydroxylapatite
a. Brand: Radiesse
b. Main mineral component of bone, synthesized as microparticles suspended in a polysaccharide gel that acts as a scaffold for collagen and tissue growth.
c. FDA approved for treatment of moderate-to-severe facial wrinkles and folds and facial lipoatrophy.
d. Injected just below the dermis to treat deep wrinkles, glabellar lines, midfacial atrophy, and nasolabial folds and for cheek and chin augmentation.
e. 6 to 18 month duration
f. Sensitivity testing is not required
g. Nodules may form if injected into the dermis
C. Nonabsorbable
1. Polymethyl methacrylate (PMMA)
a. Brand: Artefill
b. Nonbiodegradable synthetic polymer synthesized as microspheres suspended in a bovine collagen solution.
c. Induces fibroblast collagen synthesis, leading to tissue ingrowth and connective tissue encapsulation of the microspheres.
d. FDA approved only for correction of nasolabial folds.
e. Injected into the deep dermis or subcutaneous layer to treat nasolabial folds, deep wrinkles, and depressed scars.
f. Massage after injection to decrease lumps
g. May take 6 to 8 weeks for results to appear
h. Effects considered permanent, but additional volume may be required after 18+ months
i. Skin testing performed prior to use due to bovine collagen component.
D. Kenalog
1. Triamcinolone acetonide
a. May improve scar contour by inhibiting fibroblast proliferation and promoting collagen degeneration.
b. Used for hypertrophic and keloid scar management.
c. Requires multiple injections; should be spaced out in time by 3+ months to allow for effect.
d. Adverse effects include skin thinning (dermal atrophy), hypopigmentation, telangiectasia, and pain with injection.
PEARLS
1. Increasing Fitzpatrick skin type indicates increasingly dark skin with easier tanning and less burning.
2. Risks of facial peels: Hyperpigmentation (usually transient), hypopigmentation (more likely to be permanent), and infection (Herpes)
3. CO2 and Er:YAG are two laser types which are ablative. They both have water as a chromophore. However, CO2 tends to have a deeper effect.
4. Dermabrasion allows for a more controlled depth of resurfacing compared to peels.
5. Botox is now FDA-approved for chronic migraine headache treatment
QUESTIONS YOU WILL BE ASKED
1. How does re-epithelialization occur after a chemical peel?
Re-epithelialization occurs through the presence of dermal appendages which remain intact due to their location in the deep dermis.
2. Do fine wrinkles generally occur parallel or perpendicular to the orientation of the facial muscle fibers?
Over time, repetitive contraction of the facial muscles results in fine wrinkles. Contraction of these muscles occurs along the length of the muscle fibers. Therefore, the fine wrinkles develop in an orientation perpendicular to the orientation of muscle fibers.
3. What can you do to diminish the risk of hyperpigmentation after a chemical peel?
You can give the patient hydroquinone prior to the procedure. Hydroquinone inhibits tyrosinase, an enzyme that is involved in melanin production. Patients should also use sunscreen after the peel.
4. What is the concern with performing chemical peels or laser resurfacing in patients at the time of operative facial procedures (e.g., face-lift)?
Operative procedures such as face-lift require significant undermining of tissue resulting in loss of some vascular supply. Chemical peels and laser resurfacing cause intentional damage to the epithelial and superficial dermis—without a robust blood supply, these areas can be slow to heal and may even scar.
5. How will injection of Botox into the lateral orbicularis oculi affect brow position?
The lateral orbicularis is involved in lateral brow depression. Paralysis of the lateral orbicularis will result in some lateral elevation of the brow.
6. How many days after injection of Botox can you expect to see a significant change?
Generally, it takes about 3 to 5 days for patients to notice the effects of Botox.
Recommended Readings
AlKhawam L, Alam M. Dermabrasion and microdermabrasion. Facial Plast Surg. 2009;25:301–310. PMID: 20024871.
Beer K, Beer J. Overview of facial aging. Facial Plast Surg. 2009;25:281–284. PMID 20024868.
De Maio M, Rzany B. Botulinum Toxin in Aesthetic Medicine. Heidelberg, Berlin: Springer; 2007.
Goldberg D. Facial Rejuvenation. Heidelberg, Berlin: Springer; 2007.
Nguyen AT, Ahmad J, Fagien S, and Rohrich RJ. Cosmetic medicine: facial resurfacing and injectables. Plast Reconstr Surg. 2012;129:142e–153e. PMID: 22186529.
Roy D. Ablative facial resurfacing. Dermatol Surg. 2005;23:549–559. PMID: 16039434.
< div class='tao-gold-member'>