CHAPTER 58 Nipple–areola reconstruction
Physical evaluation
• Unilateral reconstruction, anatomic symmetry (opposite nipple position and size; opposite NAC texture and color and size), need for secondary contralateral surgery.
• Previous breast mound scars (from mastectomy, biopsy, reconstruction).
• The vascularity and thickness of breast mound.
• The size of the reconstructed breast.
• The presence or absence of a well-defined fold.
• The desired final breast appearance.
• Medical history: specifically diabetes/vascular disease/smoking and other co-morbidities.
• Body and breast morphology (breast dimensional analysis).
• Size of opposite breast/plan of opposite breast (prophylactic mastectomy).
Technical steps
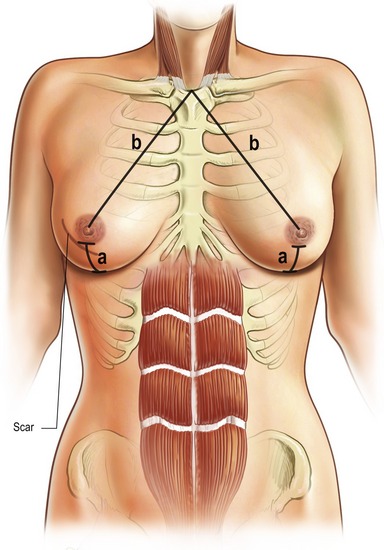
When the patient has agreed to proceed with nipple–areola reconstruction, the patient and the plastic surgeon must determine the optimal position. Specific identifiable landmarks help to determine the proper nipple areolar position visually and geometrically. These include the level of the nipple areola, the triangles with the sternal notch and the umbilicus and the nipple areolar position relative to each breast and to the inframammary fold (Fig. 58.1).
The nipple–areola position is determined visually with the patient in a standing position and the shoulder relaxed without abduction. In addition to measurement, visually the NAC is centered on the breast at the point of maximal convexity and projection, symmetric with the opposite NAC. This is why simultaneous contralateral surgery is not recommended as final shape and NAC position of the contralateral breast will change again.
Nipple–areola reconstruction is usually performed as a delayed procedure and can be either under local or general anesthesia and it is done on an outpatient basis. Several technical options are available for nipple and areolar creation. The method selected depends on the size and color of the opposite nipple and areola, the type of breast mound on which it is placed and the patient’s and surgeon’s preference (Table 58.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree