Electrodiagnostic Testing
I. Introduction
Electrodiagnostic testing is a commonly ordered set of electrophysiologic tests optimally utilized as an extension of the surgeon’s history and physical examination. The objective of testing is to confirm the presence or absence of neuropathy as a cause of the patient’s complaint. Testing evaluates for nerve entrapment or compression, demyelinating processes, and diseases that cause axonal loss in sensory and motor nerves. Testing also evaluates for disease at the neuromuscular junction and myopathies, but these processes are generally not managed by a hand surgeon and will not be discussed.
II. Definitions
Stimulator—Device used to provide electrical stimulation to the tested nerve.
Pick-up—An electrode placed to detect a sensory or motor nerve response to the stimulus. These can be discs of various styles adhered to the skin surface, or rings placed around a digit.
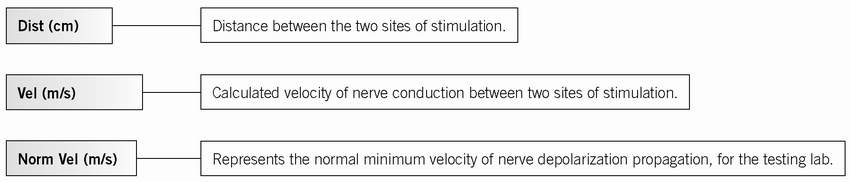
Distal peak latency—Most often reported with sensory nerve studies, it is defined as the time in milliseconds (ms) from the stimulation of a nerve to the peak of the waveform.
Onset latency—Most often reported with motor nerve studies, it is defined as the time in milliseconds (ms) from stimulation of a nerve to the onset of the compound motor action potential (CAMP).
CMAP—The waveform generated by a sum of all motor unit responses in muscle to stimulation of a peripheral nerve.
Sensory nerve action potential (SNAP)—The waveform generated by the depolarization of a sensory nerve in response to stimulation of that nerve.
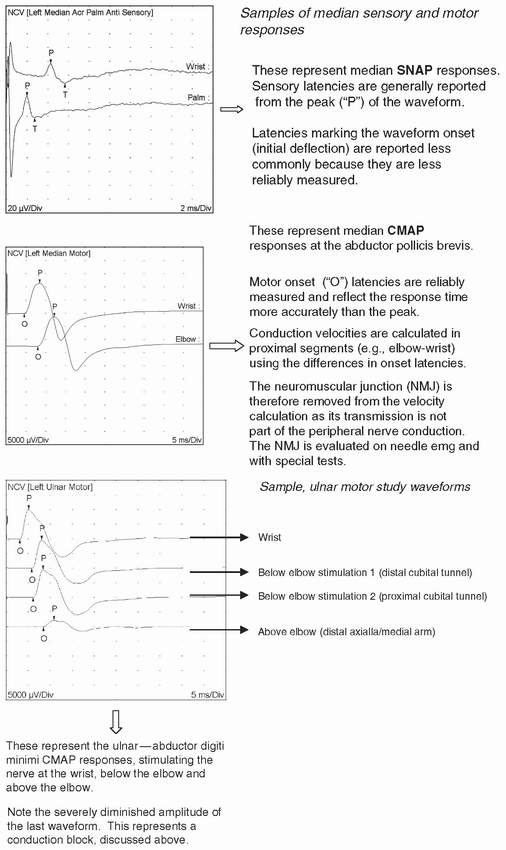
Conduction velocity—The calculated speed of stimulus transmission across a nerve segment, in meters/second. This is most often reported with motor nerve studies.
Conduction block—Observed in conditions of acquired demyelination, it refers to a decrement of decrease in the CMAP amplitude and/or area under the CMAP waveform when a nerve is stimulated proximal to the demyelinated segment. If the lesion is proximal, distal nerve stimulation demonstrates normal action potential size. The decrement required for this diagnosis is always 20% or more compared to the distal segment, but there is increasing evidence that a 50% decrement in area under the waveform is more reliable.
Conduction velocity slowing is more common than conduction block, and can be observed without meeting the absolute criteria for a true conduction
block. Velocity slowing is generally limited to compression and/or a segmental demyelinating process.
Electomyography (EMG)—Also referred to as “Needle EMG,” is performed by inserting a needle electrode into a muscle belly and observing for evidence of abnormalities in muscle membrane depolarization. Abnormalities can be observed at muscle rest (abnormal spontaneous activity, such as positive sharp waves, fibrillations, or fasciculations), or in voluntary motor unit morphology and recruitment patterns.
Motor unit—A motor unit is composed of all muscle fibers innervated by a single nerve fiber.
Temporal dispersion—The time over which a waveform occurs in response to a stimulus. It reflects the spread of signals reaching the electrode from slow and fast conducting fibers. Temporal dispersion is another parameter of segmental conduction evaluation, with an increase reflecting abnormality.
H wave—Analagous to a reflex arc, the H wave value is not utilized in upper extremity studies. A stimulus causes an orthodromic sensory response to be sent to the spinal cord, which responds with an orthodromic motor response back to the recording electrode.
F wave—This study is performed by stimulating a peripheral motor nerve and sending an antidromic motor response to the spinal cord followed by an orthodromic motor response to the recording electrode. It is useful to evaluate very proximal nerve involvement in peripheral neuropathies and in brachial plexopathies. (H and F waves are known as “late responses.”)
Neurapraxia—Describes an injury to a nerve in which the entire structure of the peripheral nerve is left intact, but conduction is temporarily impaired.
Axonotmesis—Describes an injury to a nerve involving axonal disruption within the supporting structures (which are left intact) of the nerve.
Neurotmesis—Describes an injury in which the entire nerve is disrupted.
Wallerian degeneration—Degeneration of the axon that has become detached from the neuron cell body, as in axonotmesis or neurotmesis injuries.
Positive sharp waves—Spontaneous electrical activity in a muscle that occurs relatively early in the period following denervation of the muscle studied with needle EMG.
Fibrillations—Spontaneous activity that occurs later in the period following denervation of the muscle studied with needle EMG.
Fasiculations—Spontaneous activity that indicates chronic denervation of a muscle studied with needle EMG. These can be seen clinically as well, whereas fibrillations can only be seen electrically.
Complex repetitive discharges—Spontaneous activity that indicates chronic denervation of a muscle studied with needle EMG.
Polyphasic motor units—Describes the morphology of voluntary motor units after an axonal loss has occurred followed by reinnervation of the motor unit studied via needle EMG.
Recruitment—The pattern of motor unit activation that occurs when a subject activates a muscle. Recruitment can be diminished in any case of nerve conduction impairment.
II. Anatomy
The peripheral nerves most often involved in problems presenting to the upper extremity subspecialist include
Suprascapular nerve (C5/6, upper trunk)
Long thoracic nerve (C5/6/7, upper and middle trunk)
Musculocutaneous (C5/6, lateral cord)
Radial (C5/6, posterior cord)
Axillary (C5/6, posterior cord)
Median (primarily C8/T1, also C7, lateral and medial cords)
Ulnar (C8/T1, medial cord)
III. Electrophysiology
The purpose of the nerve is to transmit motor impulses from the anterior horn cell to muscle, and from the peripheral sensory receptor to the spinal cord. The axonal membrane is electrically active, dependent on both its passive qualities and the active sodium-potassium pump, which maintains the resting membrane electrical gradient.
Axonal membranes contain voltage-dependant sodium channels. Current applied to the membrane depolarizes them and results in the opening of the sodium channels, causing an influx of sodium into the nerve. Anytime depolarization occurs beyond a threshold above the resting membrane potential an action potential is created, propagating depolarization along the axonal membrane and producing a neural impulse.
Conduction velocity depends on the diameter of the axon and its myelination. Depolarization propagates quickly between myelinated segments of the nerve, speeding conduction by occurring only at point intervals without myelin called the nodes of Ranvier (saltatory conduction). Depolarization also occurs at the neuromuscular junction.
Muscle membrane physiology is complex. Important to electrodiagnostic evaluation is the fact that muscle membrane stability is dependent on the integrity of the neuromuscular junctions of all the motor units in a muscle. Disruption of this connection between nerve and muscle results in predictable changes in muscle membrane stability and motor unit morphology. These changes are observable on needle EMG.
IV. Pathophysiology
From the discussion of electrophysiology, it is easy to comprehend the pathophysiology of neuropathy. Conduction can be impaired or blocked by direct pressure on the nerve, demyelination, or axonal loss. Axonal disruption results in the impairment of impulse propagation, disruption of the neuromuscular junction (resulting in muscle membrane destabilization and impaired motor units).
V. Common Entrapment Neuropathies and Basic Electrodiagnostic Strategy for Each
Suprascapular nerve
Compression most commonly occurs at the suprascapular notch (affecting the supraspinatus and infraspinatus) or at the spinoglenoid notch (affecting the infraspinatus only).
Stimulation is performed at Erb point or the supraclavicular fossa and onset latencies are recorded at the supraspinatus and infraspinatus. Needle EMG of these muscles is performed to determine the presence and severity of denervation.
An entrapment neuropathy at the suprascapular notch results in prolonged latencies to both muscles. An entrapment neuropathy at the spinoglenoid notch results in prolonged latencies to the infraspinatus only.
Axillary nerve
Not usually affected by intrinsic compression, axillary neuropathy is usually imposed by blunt trauma or by a stretch injury. A conduction study can be performed by stimulating the nerve superior to the clavicle and evaluating the onset latency of the CAMP. Needle EMG abnormalities limited to the deltoid and teres minor, but sparing other posterior cord-innervated muscles confirm this diagnosis. Weakness of the axillary-innervated muscles without evidence of denervation generally carries an excellent prognosis.
Musculocutaneous nerve
Entrapment by the coracobrachialis muscle may occur, and neuropathy can also follow heavy exercise. Musculocutaneous nerve palsy is also seen following anterior glenohumeral dislocation, although it is less frequent than axillary nerve palsy. Needle EMG demonstrates denervation in the biceps, brachialis, and coracobrachialis. An abnormal lateral antebrachial cutaneous sensory study can be helpful in corroborating the diagnosis especially when compared to the contralateral/unaffected limb.
Antebrachial cutaneous nerves
Lateral antebrachial cutaneous nerve—The peak latency can be prolonged, and the action potential amplitude can be diminished. It is recommended that the comparison study be made to the contralateral limb.
Medial antebrachial cutaneous nerve and posterior antebrachial cutaneous nerve neuropathies are not typically identified as mononeuropathies; but rather in association with other conditions such as brachial plexopathy.
Stimulation of the lateral antebrachial cutaneus nerve and medial antebrachial cutaneus nerves is performed at the lateral and medial antecubital arm. Surface electrodes are used to evaluate peak latencies, SNAP amplitudes, as well as action potential morphology.
Radial nerve
The nerve is susceptible to direct injury or extrinsic compression at the spiral groove, or where the radial nerve crosses from posterior to lateral at the lateral intermuscular septum.
Posterior interosseus nerve entrapment can occur anywhere along the “radial tunnel” including
Compression of the nerve at or distal to the supinator can result in compression neuropathy of the terminal branches, producing a variety of wrist/digit extensor deficit patterns. Needle EMGs of the affected muscles are useful in diagnosis.
Radial motor nerve conduction study is performed by stimulating the nerve proximal to the spiral groove, at the lateral arm distal to the spiral groove,
and in the forearm. A needle or surface electrode picks up the stimulation response, most often at the most distally innervated muscle, the extensor indicis proprius.
Sensory study of the radial nerve can be performed by placing a surface electrode over the first web space and stimulating the nerve in the lateral forearm.
Median nerve
There are two commonly encountered sites of median nerve compression: at the elbow between the two heads of the pronator teres or at the carpal tunnel.
Pronator syndrome occurs when the median nerve is entrapped while passing through the two heads of the pronator teres. It can be associated with muscle hypertrophy, trauma, fracture, or impingement by a median artery. A fibrous band can also occur connecting the pronator teres to the tendinous arch of the FDS. In addition to tenderness to palpation at the pronator teres, clinical features distinguishing it from carpal tunnel entrapment can include weakness of the flexor pollicis longus and hypoesthesia over the thenar eminence (the palmar cutaneous branch of the median nerve departs the main fiber of the median nerve and passes above the flexor retinaculum at the wrist located just ulnar to the tendon of FCR). The syndrome can be mistaken for similar symptoms produced by entrapment at the ligament of Struthers and the exceedingly infrequent humeral supracondylar process. Any weakness of the pronator teres indicates that the entrapment likely is above the muscle.
Conduction studies are useful to rule out carpal tunnel entrapment and other causes of symptoms, although mild conduction velocity slowing through the forearm is sometimes observed. In severe cases associated with axonal loss, needle EMG can be helpful to establish the pattern of denervation.
The median motor conduction study is performed by placing a surface electrode at the abductor pollicis brevis and stimulating the nerve at the wrist just proximal to the carpal tunnel (to record the onset latency) and at the medial antecubital fossa (to calculate conduction velocity between the two stimulation points).
The median sensory conduction study is performed by placing a surface electrode on the second or third digits and stimulating the nerve at the wrist, proximal to the carpal tunnel.
Anterior interosseous nerve syndrome occurs when this branch is entrapped after separation from the nerve proper, usually distal to the pronator teres. It may occur spontaneously or in association with a forearm or a supracondylar humeral fracture. There are no sensory deficits, but motor deficits may be present in the pronator quadratus, flexor pollicis longus, and flexor digitorum profundus (FDP) of the index and middle fingers. Nerve conduction studies will not reveal any abnormality, but needle EMG of the innervated muscles may reveal abnormalities confined to the nerve branch distribution. A conduction study to measure motor latency to the pronator quadratus using a needle pick-up can be performed, but should be compared to the asymptomatic limb. Conduction studies of the median nerve are otherwise performed to rule out other causes of median neuropathy.
Carpal tunnel syndrome is the most commonly diagnosed median compression neuropathy. The electrodiagnostic strategy includes confirming median neuropathy and site of entrapment at the wrist. Segmental studies across the wrist, as well as comparing the transcarpal with palm-to-digit segments for disproportionate proximal segment slowing confirm the location of compression. Needle EMG is not usually needed to identify carpal tunnel compression, but is useful to rule out cervical radiculopathy or proximal nerve involvement, especially in the case of axonal loss. Needle EMG can also help grade the severity of neuropathy, but is unlikely to redirect care.
Ulnar nerve
Like the median nerve, the ulnar nerve can be compressed around the elbow or
the wrist.
Ulnar compression neuropathy at the elbow occurs either posterior to the medial epicondyle (cubital tunnel), or at the aponeurosis joining the two heads of the flexor carpi ulnaris (FCU).
The ulnar nerve can also be entrapped at Guyon’s canal. Compression here is commonly caused by a ganglion, but can also be the product of ulnar artery thrombosis or aneurysm. A lack of dorsal ulnar sensory deficit helps differentiate entrapment here from at the elbow. If axonal loss is present, it will spare FDP III/IV and the FCU on needle EMG (a proximal lesion can selectively affect distal fibers, so the reverse is not true). Much less commonly, the nerve is entrapped distal to the cubital tunnel in the forearm, before it enters Guyon canal.
The goal of evaluating an ulnar neuropathy is localization and characterization. This includes a general assessment of latencies, amplitudes, and segmental conduction velocities. Important to evaluation of the ulnar nerve is conduction across the elbow. Routinely, a single segment is assessed from the distal axilla/medial arm across the medial epicondyle. Short segment and inching studies can also be done to attempt identification and localization of a subtle conduction abnormality. Similar to median nerve testing, transcarpal segment testing can help confirm that a prolonged distal latency is due to compression at the wrist.
Ulnar sensory studies are performed in a similar manner as for median sensory studies, placing the surface electrodes at the fifth digit. The motor study is performed by placing an electrode at the abductor digiti minimi (can also be placed at the first dorsal interosseus muscle) and stimulating the nerve at the wrist proximal to Guyon canal, distal to the cubital tunnel, and then proximal to the cubital tunnel. Similar to median nerve studies, ulnar studies evaluate onset latency CAMP amplitudes, and conduction through the forearm as well as across the cubital tunnel.
VI. Martin-Gruber Interconnections
An anatomical variant involving an interconnection from the median to ulnar nerves in the forearm can be identified. It is almost always motor, often arising from the anterior interosseus nerve. Fibers communicating from the median nerve to the ulnar nerve innervate either median nerve—innervated (thenars) or ulnar nerveinnervated muscles (first dorsal interosseus, adductor pollicis, and abductor digiti minimi). Routine conduction studies demonstrate an apparent conduction block on
proximal compared to distal ulnar stimulation, due to the higher number of motor fibers in the distal nerve that have joined from the median nerve. The number of fibers communicating varies, causing variable conduction study changes. The interconnection encountered most frequently can be confirmed by stimulating the median nerve at the elbow and recording the responses with electrodes placed over the innervated ulnar and median-innervated muscles. Stimulation of the median nerve at the wrist records a response only from the median-innervated muscle.
VII. Grading of Severity and Determining Chronicity of Compression Neuropathies
Grading severity of a peripheral compression neuropathy is variable and somewhat subjective. Test reports should include the criteria by which a neuropathy grade is assigned. There are gradients of severity within and between the following designations, generally reported as follows:
Mild: A compression that produces evidence of conduction slowing (latency prolongation) on sensory nerve testing, but demonstrates normal sensory amplitudes and normal motor responses
Moderate: Evidence of sensory axonal loss and/or motor conduction slowing (latency prolongation and/or segmental velocity slowing)
Severe: Evidence of motor nerve axonal loss (amplitude decrement not limited to a proximal segmental conduction block, and/or evidence of denervation on needle EMG)
Chronicity of an axonal neuropathy can be assessed based on the presence of conduction abnormalities and the observations made during needle EMG. In the acute phase, the appearance of spontaneous denervation potentials can range from a few days to 4 weeks or more, depending on the distance of the tested muscle from the lesion. For most upper extremity neuropathies, abnormal spontaneous activity can be observed by 21 days following injury date. Conduction abnormalities usually appear first, and can be observed within a few days to a few weeks, depending on severity and location of the injury. As recovery ensues, conduction studies may normalize depending on injury severity; and spontaneous activity may extinguish completely, while changes in voluntary motor unit morphology indicate reinnervation.
Demyelinating injuries are not easily assessed for chronicity. Pure demyelinating conditions often produce decrement in motor unit recruitment (correlating with weakness). Demyelination is not associated with the presence of abnormal spontaneous activity.
VIII. Normal Values
The normal values referenced for an electrodiagnostic study depend on local standards. Normal value ranges are generally referenced from normal population studies comprising 500 or more. Normal values can be established for a particular lab by similar testing. Because of differences in equipment used and nuance of techniques, the referenced standards of a given lab for normal and abnormal conduction results are going to be generally more reliable for interpreting results than those sourced elsewhere. Reference tables from the testing lab are almost always readily available. Finally, normal values for nerves tested are often included in the report.
IX. Limitations of Testing
Electrodiagnostic testing can be limited by several factors. First, the test requires active patient cooperation. Although it is generally uncomfortable for the patient to go through, it is almost always tolerable. Obesity, edema, peripheral vascular disease, wounds/skin breakdown, surgical scarring (especially if recent), burns, fixed deformities or contractures, casts, splints, external fixators, and the many permutations of these can all adversely affect the test by limiting the quality and amount of data collected.
X. Sample Table from an Electrodiagnostic Test
The presentation of data from electrodiagnostic reporting varies, but is similar in content. The following are representative, and the concepts are applicable from one report to another. The abnormal values are in bold type and explained. All other values are considered normal from the reporting lab. The following findings indicate a median compression neuropathy at the wrist and an ulnar demyelinating/compression neuropathy at the elbow.
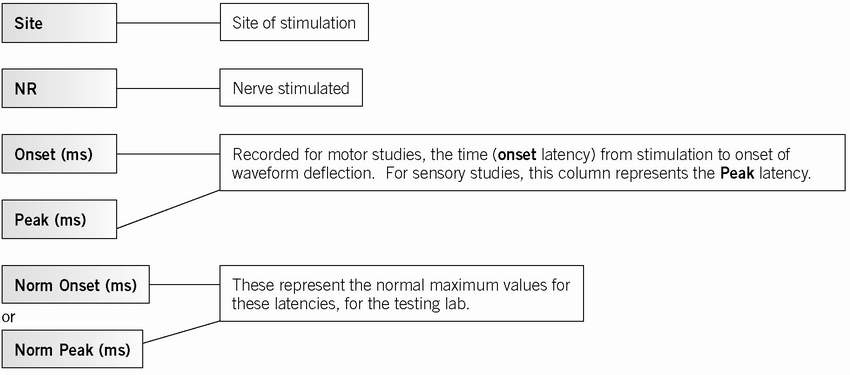
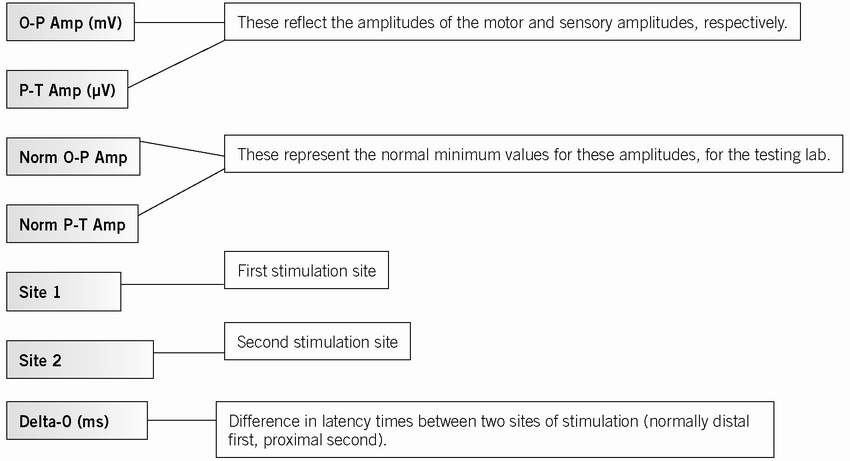
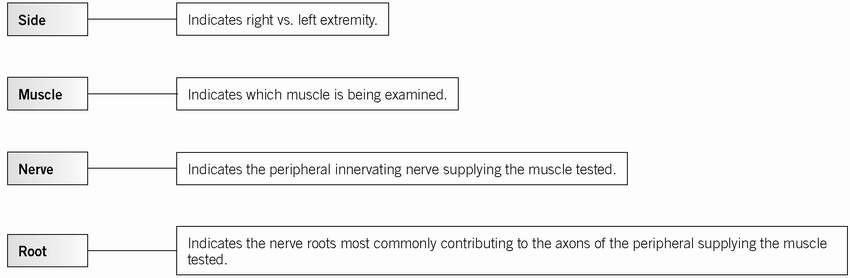
Explanation of Table Headers (tables are explained below): (
Table 17.1 and
17.2)
Examples of Nerve Conduction Study Tables, as Typically Seen in a Report (
Table 17.3)
Examples of Nerve Conduction Study Tables, as Typically Seen in a Report (continued) (
Tables 17.4 and
17.5)
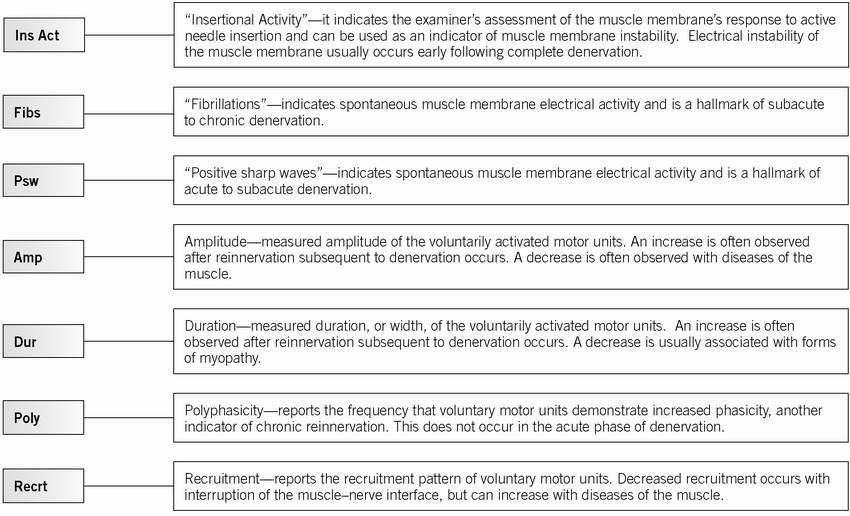
Sample Table Reporting Needle EMG Findings (
Table 17.6)
Compression Neuropathies
It is important to take note that the term “compression neuropathy” refers to a chronic condition that has developed and persisted over time, as opposed to an acute nerve compression associated with a traumatic event, such as compartment syndrome. The surgeon must have an understanding of the anatomy and pathophysiology of these conditions in order to make the correct diagnosis and proceed with the appropriate treatment. It is also imperative that the surgeon is aware of other distinct neurological problems that may exist in the upper extremity, which may blur the diagnostic picture.
Both sensory and motor symptoms are observed. Sensory symptoms can include tingling, numbness, “electric shocks,” burning, and pain. As nerve compression progresses from mild to severe, the symptoms will typically range from occasional paresthesias to constant numbness and anesthesia. Perception of vibration, movement, and pressure are the first to be lost, and perception of pain and temperature are the last to be lost. Motor symptoms can include weakness and progress to overt paralysis.
The most common compressive neuropathy in the upper extremity is median nerve compression at the wrist, or carpal tunnel syndrome, followed by ulnar nerve compression at the elbow, or cubital tunnel syndrome. Other peripheral nerve compressions in the upper extremity are much less common.