Nerve Repair and Reconstruction—Peroneal Nerve
Shawn Moshrefi
Catherine Curtin
DEFINITION
Peroneal Nerve Injury
Peroneal nerve injuries vary in severity, mechanism, and needed treatment.
The nerve injury type dictates the treatment and prognosis.
Types of nerve injury1
Neuropraxia: conduction delay with no axonal injury. These injuries will recover spontaneously without intervention.
Axonotmesis: axonal injury resulting in disruption of the axons; however, the supporting nerve scaffolding is intact. In these injuries, distal nerve segment will undergo Wallerian degeneration and proximal fibers will regenerate. Spontaneous recovery is possible.
Neurotmesis: complete disruption of the nerve. In these injuries, spontaneous regeneration will not occur.
Neuroma in continuity: disruption of the axons though the scaffolding seems to be intact. However, at the injury site, there is internal fibrosis, which prevents axons from regeneration. In these injuries, spontaneous regeneration will not occur.
Mixture of injury types: nerve patterns can be complex, and one nerve can have several different levels of injury.
ANATOMY
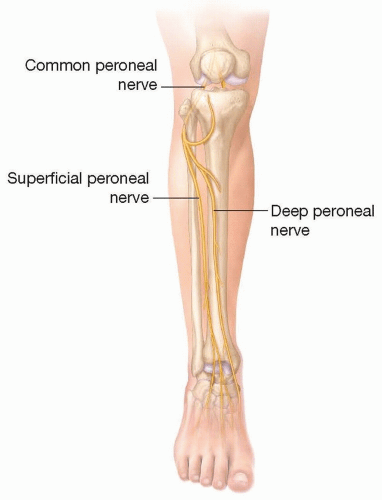
The common peroneal nerve fibers originate from L4 to S3 nerve roots (FIG 1).
The common peroneal nerve branches from the sciatic nerve in the popliteal fossa.
The motor component of the peroneal nerve innervates the anterior and lateral lower leg compartment muscles as well as some intrinsic muscles of the foot.
The sensory component of the peroneal nerve supplies the first dorsal web space of the foot and the top of the foot.
The peroneal gives off the lateral sural cutaneous branch, which joints the medial sural cutaneous branch (contributed from tibial nerve) to form the sural nerve.
The common peroneal nerve crosses from posterior to anterolateral around the neck of the fibula.
The peroneal nerve is susceptible to compression as it wraps around the fibula.
Once the nerve crosses anterior to the fibula, it branches into the superficial peroneal and deep peroneal nerves.
The superficial peroneal nerve passes straight down the lateral compartment.
The superficial peroneal nerve supplies motor to the lateral compartment (peroneus longus and peroneus brevis).
The superficial peroneal nerve supplies sensation to the top/lateral portion of the foot.
The nerve transitions from within the muscle to a more superficial subcutaneous position at the junction of the middle and distal thirds of the lower leg. This transition site can be a point of compression.
The deep peroneal nerve turns acutely around the fibular neck to enter the anterior compartment of the leg. The deep peroneal nerve then passes under the intermuscular septum between the anterior and lateral compartments to eventually course down between the tibialis anterior and extensor hallucis longus alongside the anterior tibial artery.
The deep peroneal motor nerve supplies the anterior compartment of the leg as well as some of the small foot extensor muscles: tibialis anterior, extensor digitorum longus, peroneus tertius, extensor hallucis longus, extensor digitorum brevis, and extensor hallucis brevis.
The deep peroneal nerve supplies sensation to the first web space of the foot.
PATHOGENESIS
Direct trauma can injure the nerve along its course.
Fibular fracture can lacerate the nerve or result in neuropraxia.
Knee dislocation can result in a stretch injury or even a rupture of the peroneal nerve.2
Iatrogenic injuries that occur include prolonged tourniquet time, laceration of nerve during hardware placement, and compression of nerve from operative positioning.
Swelling and compression can cause injury along the course of the peroneal nerve.
Ankle swelling can cause superficial peroneal nerve entrapment and resulting pain.
Compression from tight splints or casts can result in common peroneal nerve injury.
Soft tissue masses
Cysts, especially Bakers cysts, or other nerve compressing structures can result in peroneal nerve injury.
Neural tumors such as schwannomas can result in nerve deficits.
PATIENT HISTORY AND PHYSICAL FINDINGS
A complete and thorough history detailing patient’s history of present illness, current injuries, history of prior injuries, prior surgeries (including spinal, buttock, and lower extremity procedures), comorbidities, occupation, and other caseby-case considerations should be obtained.
Inspection
Is the leg/foot swollen?
Are there vascular changes?
Is there atrophy?
Is there a gait abnormality or foot drop?
Vascular exam should assess for palpable pulses distally, temperature, and capillary refill of the foot.
Sensory exam
Ten test: this quick test uses the contralateral area of normal sensation as a reference. The patient is lightly touched in the contralateral healthy distribution, and this normal sensation is a “ten.” Then, both the healthy and affected side are lightly touched at the same time, and the patient is asked to grade the affected side using the scale 0 to 10.3
Motor exam
Consists of testing the respective muscles that the peroneal nerve: extension of the foot and ankle.
Each muscle can be tested individually and compared to the contralateral side. Comparing to the healthy side allows for identification of subtle motor deficits seen in compression.
Motor examination remember mnemonic PED = Peroneal Everts and Dorsiflexes or more correctly noted, Extends.
Scratch collapse test4
This test can identify site of nerve entrapment.
Directly over the suspected nerve compression, the examiner gently scratches the skin. Then, the examiner immediately tests arm external rotation by applying force to the patient’s dorsal forearm. The patient attempts to resist.
A positive test on the scratch collapse test is when the patient briefly has decreased external rotation strength and “collapses” under the examiner’s pressure.
Tinel test
IMAGING
X-rays are useful for suspected bony injury.
Angiography may be required in complex trauma patients.
This is particularly important as the deep peroneal nerve runs intimately with anterior tibial artery.
MRI
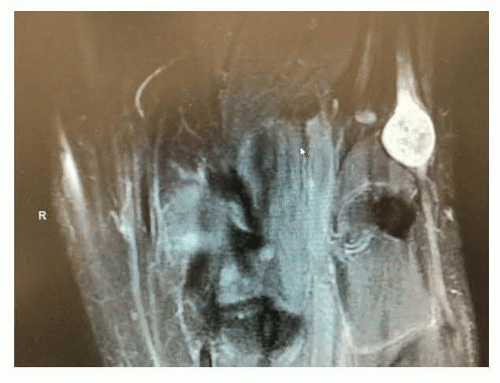
Standard MRI can assess for soft tissue masses such as Baker cysts, schwannomas, or tumors.
FIG 2 shows a large peroneal nerve schwannoma with its typical smooth bright appearance.
MRI neurogram can identify areas of nerve compression and enhancement (FIG 3).
Nerve conduction studies and electromyelography.
For acute injuries, perform the first nerve testing at least 1 month after injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree