EVALUATION OF A NECK MASS
I. HISTORY
A. Age of patient
1. Young patients are more frequently associated with congenital and infectious processes
2. Older patients more frequently have neoplastic and malignant processes
B. Duration and pattern
1. Date first noted
2. Growth pattern: Intermittent presence and fluctuations in size suggest a non-neoplastic process; slow growth followed by rapid growth suggests a neoplastic process
C. Significant symptoms that may accompany a neck mass include
1. Otalgia, dysphonia, odynophagia, dysphagia, and generalized pain
2. Constitutional symptoms: Fever, chills, night sweats or weight loss
3. Hyper- or hypothyroid symptoms: Changes in energy level, mood, or temperature sensitivity.
D. Potential associations or causal agents
1. Exposure history: TB, animals (cats), radiation, or nickel
2. Recent infections: URI, sinusitis, dental problems, or recent dental procedures
E. Family history
1. Inherited syndromes
a. Multiple Endocrine Neoplasia type I *(MEN-I): Thyroid medullary carcinoma, parathyroid hyperplasia, and pituitary tumors
b. Li–Fraumeni syndrome: Sarcoma and other malignancies
c. Basal cell nevus (Gorlin’s) syndrome: Multiple basal cell carcinomas and odontogenic keratocysts
d. Neurofibromatosis
2. Nonsyndromic family history of benign or malignant disease
F. Social history
1. Tobacco: Head and neck squamous cell carcinoma is six times more likely in smokers
2. EtOH: Potentiator especially in patients with a positive tobacco history
II. PHYSICAL EXAMINATION (requires a complete examination of head and neck; see also Chapter 14: “Squamous Cell Carcinoma of the Head and Neck”)
A. Skin: Examine the scalp, ears, face, and neck for lesions or masses.
B. Eye: Proptosis, visual acuity disturbances, or extraocular movement changes may be a sign of an orbital mass.
C. Ear: Masses or effusions may indicate Eustachian tube obstruction
D. Nose: Inspect for nasal mucosa lesions and sinus discharge
E. Oral cavity/oropharynx
1. Inspect tonsillar pillars and posterior pharyngeal wall and perform mirror laryngoscopy or flexible laryngoscopy
______________
*Denotes common in-service examination topics
2. Palpate and inspect palate, tongue (dorsal, ventral, and base), floor of mouth, gingiva, buccal mucosa, and lips
3. Evaluate salivary flow (Stenson and Wharton ducts)
F. Neck
1. Inspection
a. Evaluation for symmetry and visible masses or lesions
b. Activation of musculature and symmetry on repose and while swallowing
c. Jugular venous distension may be seen with upper neck masses
2. Palpation
a. Anterior and posterior triangles (anterior and posterior to the sternocleidomastoid muscle), including lymph node areas 1–5
b. All lymph node chains are examined for
i. Mobile versus fixed nodes
ii. Soft or doughy versus hard nodes
iii. Tenderness on palpation
3. Salivary gland palpation (see below)
4. Thyroid palpation
a. Performed from both anterior and posterior positioning
b. In repose and on swallowing
c. Evaluate size, symmetry, and consistency
G. Neurological evaluation of cranial nerve function
1. May assist in detection of an unknown primary
2. Nerve involvement may be an indicator of an aggressive neoplastic process
III. DIFFERENTIAL DIAGNOSIS OF NECK MASSES
A. *“80% Rule”
1. *80% of nonthyroid neck masses in adults are neoplastic, 80% of these are malignant, 80% of these are metastases, and 80% of these are from primaries above the clavicles
2. *80% of neck masses in children are inflammatory or benign
B. *The type of neck mass is predicted by location
1. Midline: Teratoma, dermoid, or thyroglossal duct cyst
2. Anterior triangle: Branchial cleft anomaly or lymph node (site for nodal drainage of intra- and extraoral sites)
3. Posterior triangle: Lymph node (site for nodal drainage of intra- and extraoral sites)
4. Regional sites suggestive of local disease process
a. Thyroid
b. Salivary gland (parotid, submandibular, and sublingual)
C. Adenitis
1. Nodes greater than 1.5 cm in diameter are considered abnormal
2. Bacterial etiologies include Streptococcus, Staphylococcus, Mycobacterium, Catscratch fever (Bartonella), Tularemia, and Actinomyces
3. Viral causes include Epstein–Barr virus (EBV), cytomegalovirus (CMV), herpes simplex virus (HSV), HIV, rhinovirus, and adenovirus
4. Fungal infections are likely caused by Coccidiodomycosis
5. Toxoplasmosis can cause generalized or focal lymphadenitis.
6. Empiric therapy with antibiotics for 10 days to 2 weeks is indicated if the mass is inflammatory
a. Treat the most common causes in the differential diagnosis based on history, physical examination, and appropriate diagnostic studies
b. Close follow-up of empiric treatment is required
c. Persistence of adenitis greater than 2 weeks requires additional work-up and treatment
D. Congenital neck masses
1. Branchial cleft anomalies
a. Arise from primitive branchial arches, clefts, and pouches
b. May include cysts, fistulas, or sinuses
c. *Cleft I: external auditory canal
d. Cleft II
i. Most common
ii. *Run under middle/lower sternoclydomastoid and over CN IX
iii. Runs under ECA and over internal carotid toward tonsillar fossa
iv. Third and fourth branchial cleft anomalies
e. Cleft III: Similar to cleft II but runs under ICA
f. Treated by excision of the cyst or sinus; may be complex in some cases of second branchial arch cysts, and may course around the carotid artery
2. Thyroglossal duct cyst
a. Remnant of thyroglossal duct epithelium
b. *Occur anywhere from the foramen cecum of the tongue to the suprasternal notch
c. Often found in midline
d. Most commonly diagnosed in the first two decades of life
e. Treated by complete excision of the cyst tract, decreased recurrence rate if hyoid bone included in excision (Sistrunk procedure)
3. Dermoid cyst
a. Teratoma-like cysts contain two rather than three (teratoma) germ layers
b. *Often presents as a midline doughy mass; most common in young adults
c. Usually amenable to local excision
d. Pre-op CT recommended to rule out
i. Extension of dermoid through posterior table which would require neurosurgical intervention
ii. *Glioma or encephalocele
E. Thyroid masses
1. Solitary nodule: Cyst, benign, or malignant neoplasm
2. Multinodular goiter: Toxic or non-toxic
3. Inflammatory/autoimmune: Reidel, Hashimoto, and De Quervain thyroiditis
4. Malignancy: Papillary carcinoma, follicular carcinoma, Hürthle cell tumors, medullary carcinoma, and anaplastic carcinoma. The majority of thyroid cancers are low grade (papillary and follicular) and amenable to surgical excision. Anaplastic tumors are associated with high mortality and are usually not treated surgically.
F. Neoplastic neck masses
1. Benign
a. Mesenchymal: Fibroma, lipoma, leiomyoma, rhabdomyoma, and neural tumors are usually amenable to resection
b. Salivary gland masses: See below
c. Vascular masses: Vascular malformation (not a neoplasm; actually a congenital anomaly), hemangioma, lymphangioma (See Chapter 15: “Vascular Anomalies, Lymphedema, and Tattoos”)
2. Malignant
a. Sarcoma: Fibrosarcoma, liposarcoma, neurofibrosarcoma, and angiosarcoma. Usually amenable to surgical management with or without radio-therapy (see Chapter 13: “Malignant Skin and Soft Tissue Lesions”)
b. Salivary tumors: See below
c. Lymphoma
3. Metastases
a. Primary regional site for head and neck malignancy spread is to cervical lymph nodes
b. Esophageal and lung tumors
IV. DIAGANOSTIC STUDIES
A. Ultrasound with Doppler: Useful for determination of cystic versus complex versus solid; shows association with adjacent structures (thyroid, lymph nodes); and guidance for fine-needle aspiration (FNA). Ultrasound is excellent for diagnostic imaging of thyroid disorders.
B. MRI: Best for the evaluation of primary lesions of palate, parotid, and retro- and parapharyngeal spaces
C. CT with contrast: Evaluation of nodes >1 to 1.5 cm, especially with necrotic center of greater than 3 mm; evaluation of extracapsular extension of nodal disease
D. FNA is especially useful for thyroid masses and solid masses of the neck. Accuracy is highly dependent on operator and cytopathologist experience.
E. Nuclear medicine studies: Thyroid uptake scans can be useful to determine whether a mass is actively sequestering iodine (and therefore likely benign). Salivary gland scans (see below).
F. Indications for open biopsy of a neck mass
1. Persistent for greater than 3 weeks
2. Likely metastatic without evidence of primary tumor
3. Negative endoscopy with multiple random biopsies
4. Negative FNA
5. Probable lymphoma
SALIVARY GLAND NEOPLASMS
I. SALIVARY GLAND ANATOMY
A. Glands develop during the 6th to 8th week of gestation as oral ectoderm and nasopharyngeal endoderm
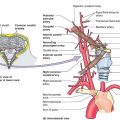
B. Parotid gland
1. *The parotid is located in the preauricular upper neck (tail) with deep and superficial lobes. The facial nerve separates the lobes.
2. The surrounding fascia of the gland is an extension of the superficial layer of the deep cervical fascia
3. The gland consists predominantly of serous acini
4. *Stenson’s duct arises from the anterior border of the parotid and enters the oral cavity at the level of the maxillary second molar
C. Submandibular (submaxillary) gland
1. Located in the submandibular triangle
2. Surrounded by the splitting of the superficial layer of deep cervical fascia
3. *Mucus and serous acini are, along with the parotid, responsible for the majority of saliva production.
4. Wharton duct arises from the medial gland and enters the oral cavity in the anterior floor of mouth
5. Closely associated with the lingual nerve which sends autonomic fibers to the gland
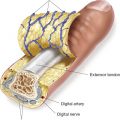
D. Sublingual gland
1. Located in anterior floor of mouth just below the mucosa
2. No fascial covering
3. Mucus acini
4. Drained by multiple ducts of Rivinus along its superior aspect entering the oral cavity. Occasionally, a coalescence of these ducts form the Bartholin duct which empties into Wharton’s duct.
E. Minor salivary glands
1. 600 to 1,000 glands are located just below the submucosal layer of the oral cavity
2. No fascial covering
3. Mainly mucous-secreting glands
4. Simple ductal system which empties directly into the oral cavity
II. DIAGNOSIS OF SALIVARY GLAND PATHOLOGY
A. History
1. Findings favoring a diagnosis of neoplasm
a. Presence over an extended period of weeks to months
b. Pain is usually a sign of advanced disease
c. Slow but persistent growth or slow growth with sudden rapid phase indicates possible malignant transformation or secondary infection with malignancy
2. Findings favoring an infectious processes. Rapid onset with signs of inflammation (warmth, erythema, and edema), repeated episodes of inflammation, alcohol abuse, autoimmune diseases (i.e., Sjogren syndrome), HIV, xerostomia, and dehydration
B. Physical examination findings
1. Findings favoring neoplasm
a. Discretely palpable firm mass especially when fixed to adjacent tissue
b. Facial nerve involvement/paralysis is a sign of malignancy
2. Findings favoring an infectious processes: Tenderness on palpation, evidence of duct obstruction, presence of a stone, purulent discharge.
III. DIAGNOSTIC STUDIES
A. FNA
1. Accuracy is dependent on operator and cytopathologist experience
2. Accuracy in distinguishing benign versus malignant approaches 90% specificity
3. Indicated only if results may change decision to operate or extent of operation
B. MRI
1. Helpful for larger tumors (>3 cm) especially where there is a question of deep lobe parotid involvement
2. Visualizes delineation of poorly defined versus sharp margins (useful for distinguishing benign vs. malignant processes)
3. In general, benign lesions demonstrate low T1-weighted signal intensity but high T2 signal due to seromucinous content. Malignant lesions show low T1 and T2 signal intensities.
4. Perineural invasion, nodal metastases, and dural involvement may be demonstrated
C. CT
1. CT for neoplastic salivary disease can be helpful in submandibular gland neoplasms; it may demonstrate bony invasion.
2. Helpful for stone identification in duct obstruction
D. Nuclear medicine studies
1. Of historical interest; of minimal use currently for salivary gland disease
2. Warthin’s tumor and oncocytoma usually have positive uptake of technetium-99
IV. *BENIGN SALIVARY NEOPLASMS
A. Pleomorphic adenoma (benign mixed tumor)
1. The most common salivary gland tumor (the most common malignantsalivary tumor is mucoepidermoid carcinoma)
2. Represents 65% of parotid and submandibular and 40% of minor gland tumors. Usually occurs in patients with 30 to 50 years of age, presenting as a painless, slowly growing mass
3. *Treated with excision: Usually a superficial parotidectomy, submandibular gland removal, or local excision of minor gland tumors. A cure rate of 95% can be expected when excised with clear surgical margins (enucleation of benign mixed tumor results in recurrence).
B. Canalicular and basal cell adenoma (previously monomorphic adenoma)
1. Rule of 75%: Canalicular adenomas present in the upper lip in 75% of cases. Basal cell adenomas present in the parotid gland in 75% of cases.
2. Female predilection 2:1
3. May resemble a mucocele, which is rare in the upper lip
4. Surgical excision is usually curative. Recurrence is rare and may actually represent multifocal disease.
C. Warthin’s tumor (papillary cystadenoma lymphomatosum)
1. *Most common site is the parotid gland
2. *Rule of 10’s (a gross simplification)
a. 10% of all parotid neoplasms are Warthin tumors
c. 10 times risk in smokers
d. Male to female ratio is 10:1.
e. 10% are malignant
3. Usually Warthin’s tumors are treated with local excision with minimal margins, or with superficial parotidectomy
D. Oncocytoma
1. Rare neoplasm (less than 1% of all salivary tumors), predominantly found in older adults
2. Usually presents in the major salivary glands with 80% arising in the parotid
3. Surgical excision is usually curative, with minimal surrounding tissue taken to establish clear margins
V. MALIGNANT SALIVARY NEOPLASMS
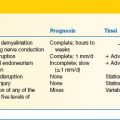
A. Mucoepidermoid carcinoma
1. *Most common salivary malignancy (however, the most common salivary neoplasm is pleomorphic adenoma)
2. Mucoepidermoid tumors represent 10% of parotid and submandibular neoplasms and 20% of minor gland neoplasms
3. *Most (70%) are found in the parotid gland, but they may also arise in the submandibular and minor salivary glands and intraosseous locations
4. Classified as low, intermediate, and high grade based on histopathology
5. Treatment is based on grade
a. Low: Surgical excision with negative margins; 90% cure rate
b. High: Treat like squamous cell carcinoma; 30% cure rate with neck dissection and postoperative radiation therapy
B. Adenoid cystic carcinoma
1. Represents approximately 10% of all salivary malignancies, and 40% of minor gland malignancy
2. Rare in the parotid; most common malignancy in the submandibular gland
3. Consists of cribriform, tubular, and solid histopathologic types
4. *Perineural spread is common which may include skip lesions (breaks in continuum) which are best seen preoperatively with MRI
5. Treat with surgical excision and radiotherapy; 5-year survival is 70%, but 15-year survival is approximately 10%
C. Polymorphous low-grade adenocarcinoma
1. Almost exclusively found in minor salivary glands
2. Presents in hard/soft palate in 60% of patients; also presents commonly in upper lip and buccal mucosa
3. 70% female; commonly presents in 6th to 8th decade of life
4. Perineural invasion is common
5. Wide surgical excision is indicated, including bones when involved
D. Acinic cell carcinoma
1. Rare (1%), low-grade malignancy; metastasis is unlikely
2. 95% arise within the parotid gland
3. Broad age range of presentation, from 3rd to 8th decade of life
4. Excision with superficial versus total parotidectomy, submandibular gland removal, or wide local excision of minor glands is usually curative
5. Radiation therapy may increase local control
E. Malignant mixed tumors (carcinoma ex pleomorphic adenoma)
1. Results from malignant degeneration of pleomorphic adenoma (10% degenerate)
2. Often presents with rapid growth in previous slow-growing lesion
3. Pain and facial nerve involvement often present
4. Treated with excision, neck dissection, and radiation therapy. Five-year survival is 50%
VI. MALIGNANT NEOPLASM MANAGEMENT
A. Surgical treatment of local disease is usually accomplished with primary tumor control, that is
1. Total parotidectomy
2. Partial parotidectomy
3. Submandibular gland removal
4. Sublingual/minor gland removal
B. Indications for neck dissection
1. Dependent on low- versus high-grade primary tumor pathology
2. Dependent on clinical presentation
3. Primary lesion size >4 cm increases likelihood of nodal disease and need for neck dissection
C. Postoperative radiation therapy
1. Increases locoregional control in larger malignancies or close margins
2. 60 to 65 Gy usually administered postoperatively
3. Should be used in high-grade malignancies, resudual or recurrent disease, T3 or T4 parotid malignancies and invasion of adjacent structures
D. Postoperative complications of salivary tumor excision
1. Sialocele
a. Presents as postoperative swelling with fluid collection
b. *Aspiration with placement of pressure dressing is usually successful for treatment
c. Botulinum toxin injection may be useful for resistant sialoceles
2. Facial nerve damage (see Chapter 24: “Facial Paralysis”)
a. *Damaged nerves should be immediately repaired if transection is noted intraoperatively, or grafted if a branch is intentionally resected for malignant disease
b. *Loss of the marginal mandibular or temporal branches results in the most significant longstanding deformity due to lack of arborization; the zygomatic and buccal branches have extensive arborization and the distal branches will often recover function
c. The frontal/temporal branch is most important for eye closure and needs consideration for reconstruction if there is evidence of inadequate arborization from the buccal/zygomatic branch
3. *Frey’s syndrome (auriculotemporal syndrome)
a. *Caused by reinnervation of sympathetic sudomotor (sweat) fibers by severed parasympathetic (salivomotor) fibers normally directed to parotid gland
b. Results in preauricular gustatory sweating (sweating in response to salivary stimulation)
c. Demonstrated by Minor starch–iodine test (topical starch/iodine powder mixture turns blue with sweating)
d. Relatively common (up to 30%) in patients after parotidectomy when iodine tested but many fewer patients complain of symptoms (<5%)
e. Initial treatment is topical antiperspirant prior to meals
f. Long-term treatment may require botulinum toxin (BoTox) injections for control
g. Thought to be caused by auriculotemporal nerve
PEARLS
1. 80% of nonthyroid neck masses in adults are neoplastic, and of those, 80% are malignant. However, 80% of neck masses in children are benign.
2. Indications for open biopsy of a neck mass
a. Persistent for greater than 3 weeks
b. Likely metastatic without evidence of primary tumor
c. Negative endoscopy with multiple random biopsies
e. Probable lymphoma
3. Slow-growing salivary gland lesions that suddenly begins rapid enlargement are often carcinoma
4. Mucoceles are common in the lower lip but rare in the upper lip.
5. Rule of 10’s for Warthin tumors
a. 10% of all parotid neoplasms are Warthin tumors
b. 10% are bilateral
c. 10 times risk in smokers
d. Male to female ratio is 10:1
QUESTIONS YOU WILL BE ASKED
1. What is the course of frontal branch of facial nerve?
The frontal branch can be roughly located along a line extending from the attachment of the lobule (approximately 5 mm below the tragus), anterior and superior to a point 1.5 cm above the lateral aspect of the ipsilateral eyebrow. The frontal branch crosses the zygoma approximately 1.5 cm anterior to the tragus. It runs superiorly to about 2 cm lateral to the lateral canthus. It runs within the temporoparietal fascia (also known as the superficial temporal fascia).
2. What is the course of marginal mandibular nerve?
The marginal mandibular branch crosses the mandible within 1 cm of the facial notch.
3. What is the relation of marginal mandibular nerve to facial vessels?
The marginal mandibular nerve crosses superficial to the facial vein and artery.
4. Name five ways to find the main trunk of the facial nerve.
1) The tympanomastoid suture is the most reliable landmark (this is 6 to 8 mm lateral to the stylomastoid foramen).
2) It lies approximately 10 mm inferior and 10 mm deep to the tragal pointer.
3) Identify distal branches and follow proximally.
4) It lies approximately at the level of the digastric muscle (in the superficial to deep dimension).
5) Drill out the mastoid to identify the descending (intratemporal) segment.
Recommended Readings
Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2009;19(11):1167–214. PMID: 19860577.
Lima RA, Tavares MR, Dias FL, et al. Clinical prognostic factors in malignant parotid gland tumors. Otolaryngol Head Neck Surg. 2005;133:702–708.
O’Brien CJ. Current management of benign parotid tumors—the role of limited superficial parotidectomy. Head Neck. 2003;25:946–952.
Scianna JM, Petruzzelli GJ. Contemoporary management of tumors of the salivary glands. Curr Opin Rep. 2007;9:134–138. PMID: 17288880.
Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 1986;8:177–184.
Torsiglieri AJ Jr, Tom LW, Ross AJ 3rd, et al. Pediatric neck masses: guidelines for evaluation. Int J Pediatr Otorhinolaryngol. 1988;16:199.
Tracy TF Jr, Muratore CS. Management of common head and neck masses. Semin Pediatr Surg. 2007;16(1):3–13. PMID: 17210478.
Witt RL. Major salivary gland cancer. Surg Oncol Clin North Am. 2004;13:113–127.
< div class='tao-gold-member'>