I. HISTORICAL ORIGINS
A. References of total nasal reconstruction date as far back as 3000 BC India.
B. Local cheek flaps published in “Sushruta Samhita” by Sushruta (India, 700 BC).
C. Adjacent tissue rearrangements recorded by Celsus (Greece, ~40 AD) and Paulus Aegineta (Byzantine Greece, ~660 to 680 AD).
D. Italian method used the arm flap, originated by Branca in ~15th century Italy, published by Tagliacozzi in 1597.
E. Indian method using the forehead flap, originated in ~1440 in India and Nepal by Kanghiara or Mahrattas families, published by “Madras Gazette” in 1700s Bombay, reproduced in English in “Gentleman’s Magazine” in 1794 England.
II. IMPORTANT FACTORS TO NOTE WHEN DEFINING THE DEFECT
A. Etiology of the defect
1. Skin cancer: Must have clear oncologic margins before reconstruction
a. Immediate reconstruction preferred after Mohs excision, and sometimes after frozen sections depending on tumor type and aggressiveness, due to the possibility of false-negatives (know your pathologist and Mohs surgeon and the reliability of their reports).
b. Delayed reconstruction (e.g., non-Mohs or melanoma resection)
2. Trauma, ischemic necrosis (e.g., secondary to rhinoplasty), and infection: Reconstruction proceeds when the viability of the remaining tissue is certain
III. LOCATION OF THE DEFECT
A. Proximal, middle, or distal third of nose
B. Nasal subunits that are involved
IV. SIZE OF THE DEFECT
A. Less or greater than 1.5 to 2.0 cm (for choosing local flap vs. forehead flap).
B. *If more than 50% of a subunit is involved, then include the remainder of the subunit as part of the estimated defect size (subunit principle).
V. TISSUE PLANES INVOLVED BY THE DEFECT
A. External nasal cover: Skin, subcutaneous fat, and submuscular aponeurotic system (SMAS)
B. Structural support: Perichondrium/cartilage and periosteum/bone
C. Internal nasal lining
ANATOMY
I. NASAL REGIONS (BY THIRDS)
A. Proximal third
1. Nasal bones and bony septum
2. Thin skin over the radix
3. Nasal bones thicker more proximally
______________
*Denotes common in-service examination topics
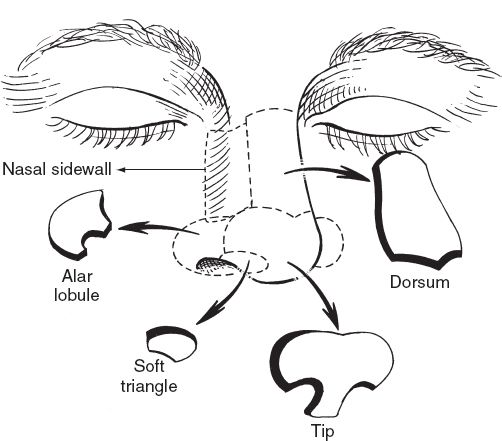
Figure 20-1. Nasal aesthetic subunits.
B. Middle third
1. Upper lateral cartilages and cartilaginous septum
2. Thin skin over the dorsum
C. Distal third
1. Lower lateral cartilages, nasal tip, alae, and caudal cartilaginous septum
2. Thick, less mobile, sebaceous skin over the nasal tip and alae
II. NASAL SUBUNITS (NINE TOTAL)
A. *Dorsum, two sidewalls, tip, two alae, columella, and two soft triangles (Fig. 20-1).
III. LAYERS (SUPERFICIAL TO DEEP)
A. Skin
B. Subcutaneous fat
C. SMAS (± musculature)
D. Deep fatty layer (very thin)
E. Perichondrium/periosteum
F. Cartilage/bone
G. Mucosa/mucoperichondrium
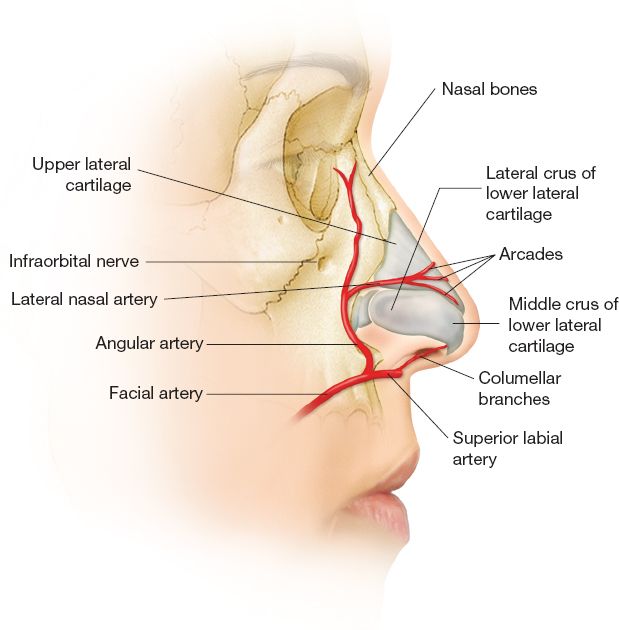
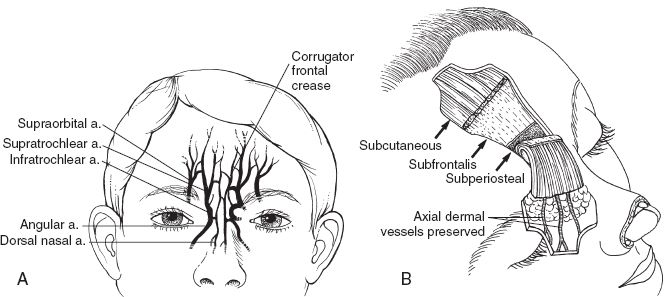
IV. RELEVANT VASCULAR SUPPLY—Major nerves and blood vessels of the external nasal covering run deep to the SMAS, with a few exceptions (Fig. 20-2).
A. External carotid artery branches
1. Angular arteries
a. Branch of facial artery
b. Superficial to or within the SMAS
c. Supplies lateral surface of caudal nose
d. Gives off lateral nasal arteries
2. Superior labial arteries
a. Within the orbicularis oris muscle, or between the mucosa and muscle
b. Supplies nasal sill, septum, and base of columella
Figure 20-2. Arterial supply of external nasal cover.
3. Infraorbital arteries
a. Branch of internal maxillary artery
b. Supplies dorsum and lateral nasal side walls
B. Internal carotid artery branches
1. Dorsal nasal branch
a. Branch of ophthalmic artery
b. Supplies dorsum and lateral skin
2. External nasal branch
3. Supratrochlear arteries
a. Branch of ophthalmic artery
b. 1.7 to 2.2 cm from midline
c. Runs between corrugators and frontalis layers at orbital rim, becoming superficial to frontalis at mid-forehead level.
4. Supraorbital arteries
a. Branch of ophthalmic artery.
b. ~2.9 cm from midline
c. Runs through a notch or foramen with a superficial branch coursing superficial to SMAS and a deep branch coursing deep to or within the SMAS.
C. Venous anatomy: Venous drainage parallels arterial supply. Note—The angular vein becomes the anterior facial vein and communicates with the ophthalmic veins and cavernous sinus.
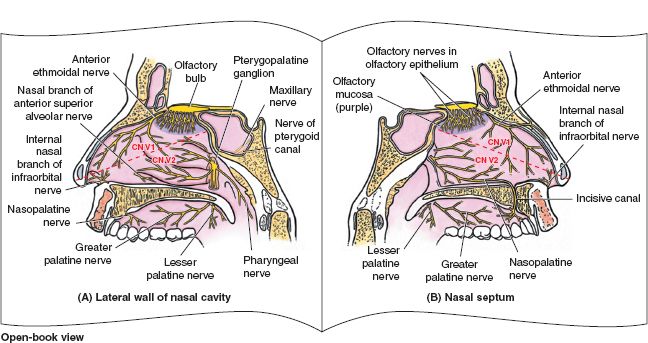
Figure 20-3. Innervation of nasal cavity. A: Sensory innervation of the lateral wall of the nasal cavity. B: Sensory innervation of the medial wall and the nasal septum. (From Agur AMR, Dalley AF, eds. Grant’s Atlas of Anatomy. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2004.)
D. Septal vasculature: Branches of the anterior ethmoidal artery, posterior ethmoidal artery, sphenopalatine artery, and superior labial artery.
E. *Lateral nasal wall vasculature: Branches from anterior ethmoidal artery, posterior ethmoidal artery, and sphenopalatine artery.
V. INNERVATION (FIG. 20-3)
A. Sensory
1. External cover: Branches from the ophthalmic (V1) and maxillary (V2) divisions of the trigeminal nerve
a. *Supratrochlear, infratrochlear, and external nasal branches of the anterior ethmoidal nerve (derive from V1).
b. Infraorbital nerve (derives from V2)
2. Septum: Branches of the anterior ethmoidal (V1) and nasopalatine nerves (V2).
3. Lateral nasal wall: Branches of the anterior ethmoidal (V1) and branches of the pterygopalatine nerve (V2).
B. Motor innervation to muscles of the SMAS layer is supplied by branches of the facial nerve (VII).
SURGERY
I. GENERAL OBJECTIVES (depending upon the defect, one or more of these objectives will need to be achieved)
A. Establish or repair bony/cartilaginous foundation
B. Restore internal nasal lining
C. Restore external cover
D. Maintain patent airway
E. Optimize aesthetic result
II. OPTIONS FOR BONE/CARTILAGE FOUNDATION
A. Midline (septal) foundation
1. L-shaped septal strut (fabricated from septal cartilage, bony septum, rib, outer table cranium, or iliac bone)
2. *Cantilevered graft (fabricated from septal cartilage, bony septum, rib, outer table cranium, or iliac bone) and secured to the remaining nasal bones or frontal bone
3. *Septal pivot flap based superiorly per Millard or inferiorly per Burget and Menick.
4. Alloplastic materials such as vitallium, titanium, or porous polyethylene; we do not encourage the use of these due to the high rate of exposure and infection.
B. Lateral structures (nasal bones, upper lateral cartilages, and lower lateral cartilages)
1. Use septal, conchal, or rib cartilage
2. Reconstruct native cartilage anatomy when possible
3. Bolster reconstructed areas that are prone to collapse (sidewalls, alae, and columella) with cartilage grafts
4. Maintain airway patency (spreader grafts)
5. Lateral crural strut graft
a. Measures 3 to 4 mm wide by 20 to 25 mm long
b. Lateral end spans from piriform rim to lateral crura
c. Positioned caudal to alar groove.
d. Useful for lateral crural malposition and alar retraction
C. Alar support
1. Alar batten graft
a. Used for alar collapse and external nasal valve obstruction.
b. Placed cephalad to alar rim.
2. Alar contour graft
a. Inserted through infracartilaginous incision into alar-vestibular pocket inferior to rim of crus.
b. Used to recreate external nasal valve.
III. OPTIONS FOR RESTORING NASAL LINING (For larger defects, one may combine multiple available options. Lining must be restored because wound contraction caused by secondary healing always results in significant distortion of the nose or synechiae.)
A. Residual nasal vestibular lining
1. Often more nasal lining is available than is apparent, especially with a contracted, secondarily healed defect involving the alar rim.
2. Advancement of 2 to 3 mm of internal lining may be achieved; must use cartilage graft to provide rigid support to prevent subsequent retraction.
3. Often carried out in a bipedicled fashion; donor site may need coverage with full-thickness skin graft.
B. Turnover flap
1. Most appropriate for situations when the external nasal cover is to be reconstructed with a forehead flap.
2. The external nasal cover is turned in (rather than discarded) to be used as lining.
3. The scarred nature of the external nasal cover in these situations make the “turnover flap” relatively avascular with unreliable survivability.
4. Must be kept <1 cm in length.
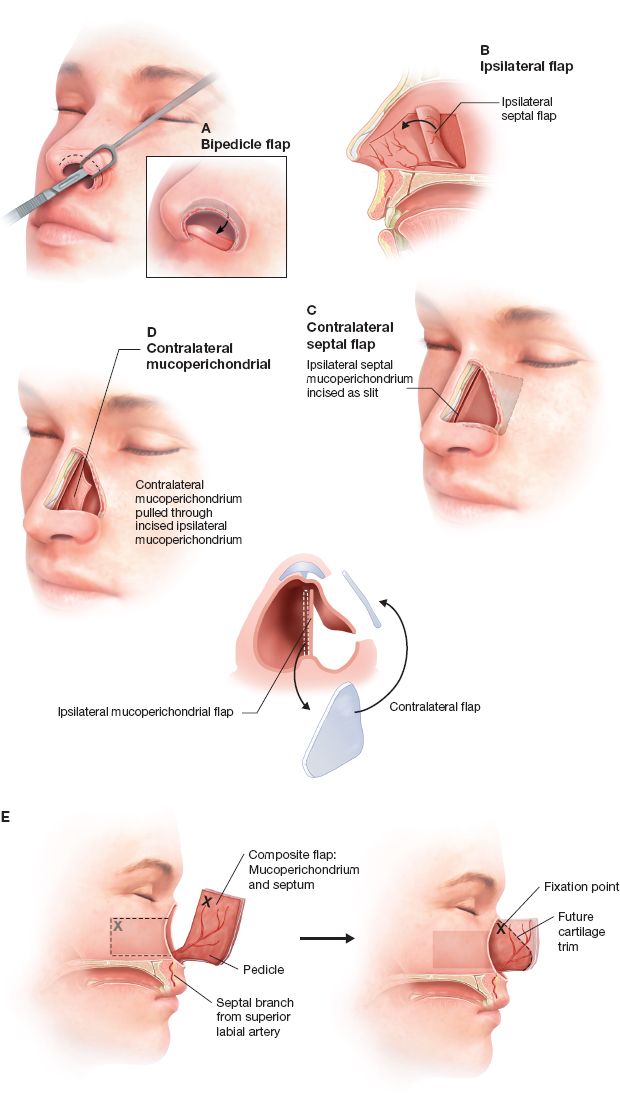
C. Intranasal flaps for lining (generally contraindicated for smokers) (Fig. 20-4)
1. Ipsilateral septal composite flap
a. Based upon axial septal blood supply (septal branch off the superior labial artery) and includes septal mucoperichondrium.
b. Appropriate for cases with unilateral defect involving the internal lining of the middle and upper vaults.
2. Contralateral septal composite flap (septal door flap) can also be used, where nasal septum and contralateral mucoperichondrium is hinged on the dorsum and transferred into the defect such that the septal mucosa now lines the airway. Based on anterior ethmoid artery.
D. Other flaps for lining
1. Inferior turbinate flap
a. May be used for small full-thickness alar defects.
b. Pedicle based upon the anterior attachment of the turbinate.
2. FAMM (facial artery musculo-mucosal) flap.
a. Good for lining the middle vault.
b. Consists of intraoral mucosa, submucosa, strip of buccinator muscle, deeper plane of orbicularis oris muscle, and facial artery with its venae comitantes.
c. Based superiorly upon the alar base and centered over the facial artery.
d. 8 to 9 × 1.5 to 2 cm of tissue available; may be passed via a tunnel directly into the nose (without any external scars).
Figure 20-4. Intranasal lining flaps. A: Bipedicle flap. B: Ipsilateral mucoperichondrial flap. C: Contralateral mucoperichondrial flap. D: Contralateral septal flap. E: Composite flap.
a. Rarely is used for nasal lining, usually in situations when all other options have been exhausted.
b. May perform delay to maximize chance of flap survival.
c. Disadvantages include thicker, stiffer tissue, and it cannot be thinned at initial transfer.
E. Forehead flap techniques for internal lining
1. Full-thickness skin graft
a. Used to line a full-thickness forehead flap (skin, subcutaneous fat, and frontalis muscle).
b. Cartilage grafts are NOT immediately placed under skin-grafted areas.
c. Reconstruction typically performed in three stages, and cartilage grafts are inserted under skin-grafted areas during subsequent stages of reconstruction.
2. Folded forehead flap
a. For full-thickness unilateral and bilateral defects.
b. Can replace internal lining defects up to 3.5 cm.
c. Uses the most distal edge of the flap (often within the scalp) harvested superficial to frontalis muscle and folded over on itself.
d. Best used in a three-stage reconstruction with cartilage grafts placed during the second stage.
3. Prelaminated forehead flap
a. Viable option for small- to medium-sized rim defect in elderly or debilitated patients for whom the priority is to minimize the physiologic burden of each surgery (with less emphasis upon aesthetic outcome).
b. Each procedure may be done under light sedation or local anesthesia alone.
c. Preliminary operation involves application of a full-thickness skin graft to the distal deep surface of the flap under the frontalis muscle along the proposed nostril margin of the planned forehead flap. Cartilage graft also placed between the frontalis muscle and overlying external skin (providing rim support along nostril margin).
d. Usually requires at least three surgical stages.
4. Second forehead flap
a. May be used for large internal lining defects.
b. A second forehead flap may be used for lining of the forehead flap used for external cover.
c. Midline support may be established at initial surgery.
d. Lateral support (alar cartilage grafts) should be placed at subsequent thinning.
F. Free flap
1. Multiple available donor options
a. Radial forearm free flap
b. Temporoparietal fascia flap + skin graft
2. Usually needed with
a. Large and deep defects to central face (e.g., shotgun injury)
b. Major contamination, radiation injury, or immunosuppression
3. Requires a multiple staged reconstruction
a. Initial stages involve temporary external nasal cover (e.g., radial forearm free flap folded upon itself) and temporary structural support (metal or cadaveric cartilage).
b. Final bony/cartilage support and external nasal cover (e.g., forehead flap) are placed at later stages.
IV. OPTIONS FOR RESTORING EXTERNAL NASAL COVER (MOST COMMON FOR SMALL DEFECTS)
A. Technical pearls
1. Convert circular defects into square defects with sharp corners (circular defects encounter concentric contraction when healing).
2. Incisions should follow natural relaxed skin tension lines when possible; place upon junction of lateral nose and cheek when possible; orient vertically or transversely upon glabella and nose.
3. No incisions on concavities
B. Smaller defects (less than 1.5 to 2 cm in greatest dimension)
1. Upper third/radix
a. Secondary healing
b. Primary closure (wounds smaller than 5 to 10 mm)
c. Integra ± full-thickness skin graft (preauricular or postauricular)
d. Local flaps
i. Single lobe transposition flaps (Banner, Romberg)
ii. Dorsal nasal flap and its variants (can actually reconstruct up to ∙2.5 cm defects)
a) Based laterally on angular arteries
b) Entire nasal dorsum rotated and advanced caudally
iii. Glabellar flap
2. Middle third/dorsum and sidewalls
a. Secondary healing
b. Primary closure (wounds smaller than 5 to 10 mm)
c. Integra dermal regeneration matrix ± full-thickness skin graft (preauricular or postauricular)
d. Consider cheek flap for recruitment of tissue onto sidewalls
e. Local flaps
i. Single lobe transposition flaps (Banner, Romberg)
ii. Dorsal nasal flap
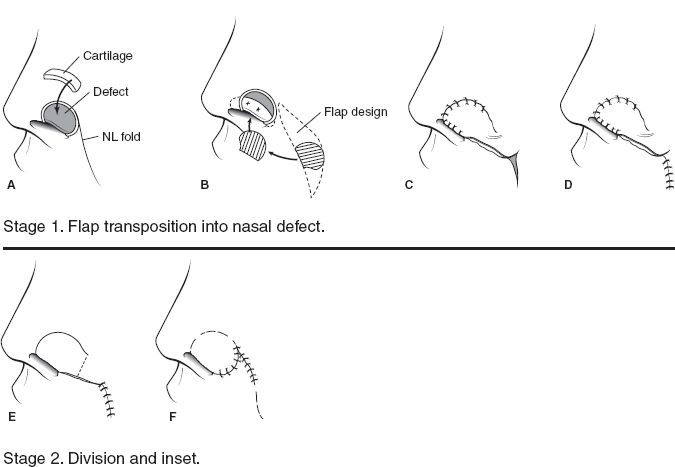
iii. Nasolabial flap (Fig. 20-5): for sidewall/alar defects up to 2 cm
iv. V–Y advancement: Good for small defects along the alar groove
v. Rhombic flap
3. Nasal tip
a. Integra dermal regeneration matrix + secondary healing versus full-thickness skin graft from forehead.
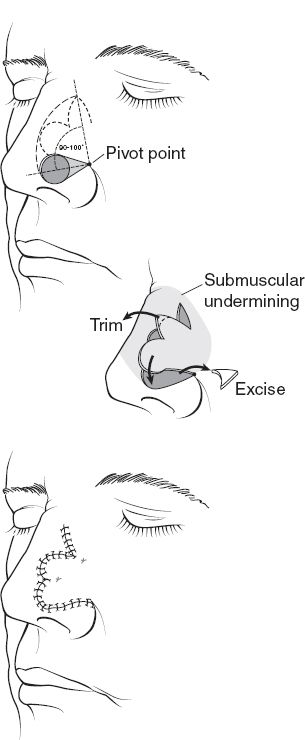
b. Local flap—bilobed flap (Fig. 20-6)—does not reach the infratip lobule; should not be used to reconstruct defects within 0.5 cm of nostril rim
i. For defects measuring 1.5 cm or less
ii. If the defect is within 1 cm of the nostril margin, some degree of rim distortion is expected.
iii. Maximum 50 degrees of rotation per lobe or 100 degrees total.
iv. Undermine widely above perichondrium/periosteum.
v. First lobe diameter should equal the defect diameter.
4. Alae
a. Local flap—nasolabial flap (Fig. 20-5)
i. For defects up to 2 cm
ii. Perform under general anesthesia (avoid distortion/blanching of local anesthetic)
iii. Immediate insertion of cartilage graft
iv. If entire alar subunit is to be reconstructed, it should be done in two stages.
b. Composite grafts (auricular donor site for chondrocutaneous tissue)
i. For full-thickness defects (external cover, fibrofatty tissue, and internal lining) involving the alar margin or soft triangle.
ii. All portions of the placed graft must be within 1 cm from a wound edge (i.e., maximum theoretical limit of defect is 2-cm diameter); ideal defect size is 1 cm or less. Donor graft is harvested slightly larger than defect to accommodate expected contraction with healing.
iii. Reported survival rates ranging from 50% to 90%; ~30% failure or significant necrosis is to be expected.
iv. Helical crus for alar rim defect; other donor sites on the ear may be used.
Figure 20-5. Two-stage nasolabial flap.
v. Improved graft take and aesthetic result when defect is allowed to heal secondarily and reconstructed in delayed fashion.
vi *Graft is white initially; turns blue at 24 to 72 hours; then gradually becomes pink over subsequent days.
C. Larger or adversely located defects (defects >1.5 to 2 cm or defects located upon the infratip lobule and within 0.5 cm of nostril rim)
1. Forehead flap (Fig. 20-7)
a. Two-stage
i. Flap is partially thinned distally at the initial transfer (supratrochlear arteries become subcutaneous at level of mid-forehead).
ii. Makes the flap more susceptible to necrosis.
b. Markings
i. Supratrochlear artery is found 1.7 to 2.2 cm lateral to midline and usually corresponds to vertical tangent of medial border of eyebrow.
ii. Doppler out course in preoperative area.
iii. Create flap base about 1.5 cm (0.7 cm to each side of artery).
iv. Mark out rhytids so that they line up at the end of the case.
v. Curve the pedicle of the flap into non-hair-bearing areas.
vi. Template is created from the defect and placed at anterior hairline with flap centered over the supratrochlear artery.
c. Surgery
i. Inject lidocaine with epinephrine into entire forehead and nose. Block nerve up into hairline where you are going to take out standing cutaneous deformity (SCD).
ii. When injecting, do not infiltrate too much to avoid distortion.
iii. Place patient in 20 to 30 degrees of reverse Trendelenberg to decrease venous pooling.
iv. Prep the patient’s full face and scalp including the submental area.
v. Create template of the defect with Telfa or chromic paper.
Figure 20-6. Bilobed flap. Markings for blob flap (above). Undermining, elevation and trimming of flap during transposition (middle). Bilobe flap following inset (below).
Figure 20-7. Forehead flap. A: Arteries (a.) of the forehead. This richly anastomotic network provides the basis for the paramedian forehead flap (B).
vi. Place cut template from hairline upside down onto the nose so that it will rotate clockwise from right side or rotate counterclockwise from left side.
vii. Use a suture to measure distal end of template to level of medial brow and then see if it reaches from medial brow to distal recipient site.
viii. Pedicle is incised through skin, subcutaneous tissue, muscle, and f ascia, except not completely through the galea at the distal part of the flap.
ix. Flap is elevated from superior to inferior.
x. Rapid dissection until reaching the corrugator at which point muscle is dissected away from underlying periosteum bluntly (use spreading scissors).
xi. Once you are near the pedicle, enter the subfascial plane just superficial to periosteum of frontal bone.
xii. At the supraorbital ridge, score the periosteum and go under periosteum with periosteal elevator.
xiii. You may see the pedicle on deep surface of the frontalis muscle as it exits over or through the corrugator.
xiv. Undermine the entire forehead in both directions in subfascial plane.
xv. Make parallel vertical galeotomies 2 to 3 cm apart to help close the donor site, but avoid supraorbital nerve just medial to temporal line.
xvi. If needed, use foley catheter balloon for intraoperative tissue expansion to facilitate closure of the donor site.
xvii. Use 2-0 Vicryl suture to reapproximate fascia moving from inferior to superior.
xviii. If cannot close the top, can leave open and place bacitracin.
xix. Cut out SCD from top of donor site into hair and use staple for the scalp.
xx. Tailor thickness of flap by thinning distal portion removing muscle and most of subcutaneous fat using a no. 15 blade.
xxi. Bevel out 45 degrees around the edges of the forehead flap.
xxii. The most distal aspect of flap should be skin only and progressively becomes thicker from most distal to most proximal portions
xxiii. Inset flap with 4-0 monocryl in deep dermis followed by a running 6-0 nylon suture.
xxiv. Can wrap the raw part of flap with Integra
xxv. *Divide pedicle between 10 days and 3 weeks and inset flap.
xxvi. At second stage, can just thin distal flap and place back down or cut and inset pedicle and thin flap.
D. Columellar reconstruction—many options, none are ideal
1. Full-thickness skin graft from forehead (in situations without cartilaginous deficit)
2. Banked forked flaps and variants (soft tissue in the region of the columellar footplate/nasal floor/upper lip is rotated or advanced onto the columella)
3. Nasolabial flaps
4. Tunneled labial mucosal flap
5. Composite chondrocutaneous grafts. Helical rim used for the columella
6. Forehead flap
V. COMPLICATIONS
A. Possible complications
1. Infection: Cellulitis ± purulent drainage; always consider the possibility of infection involving the underlying structural grafts
a. Aggressive antibiotic treatment
b. Any abscess must be washed out
c. Persistent drainage suggests infection of structural grafts; investigate for internal lining defect
2. Necrosis of flap can be avoided by protecting the vascular supply to avoid ischemia.
a. Debride as needed
b. If flap cannot be salvaged with acceptable aesthetic result, plan on performing another flap.
B. Factors leading to complication
1. Inappropriate pedicle width (pedicle base should be 1.2 to 1.5 cm). Wider bases will encounter undue tension on rotation.
2. Flap design is too short or with pivot point too high (causing excess tension)
3. Excessive thinning at first stage leading to vascular compromise.
4. Excessive re-elevation of flap at stage II (do not elevate beyond 1 to 1.5 cm of the tip and nostril margin).
5. Smoking—three-stage approach is safer in smokers; avoid “intranasal flap” options for internal lining.
6. Radiation—can lead to severe atrophy, induration, or ulceration.
RHINOPHYMA
I. FEATURES AND ETIOLOGY
A. Most advanced stage of rosacea (1—frequent facial flushing; 2—thickened skin/telangiectasias/erythrosis; 3—acne rosacea; 4-rhinophyma).
B. Predominantly male disease; prevalent among English/Irish ancestry, peak presentation at later than age 50, probably no association with alcohol.
C. Disease begins with vascular instability of the skin; fluid is lost into interstitium; inflammation and fibrosis follows. Dermal and sebaceous gland hypertrophy develop. Sebaceous ducts become plugged resulting in dilation and cyst formation.
D. Therapies
1. Nonsurgical (will slow progression, but does not cure): both topical and oral antibiotics/retinoids
2. Surgical (goal is complete resolution, allow surgical site to heal secondarily)
a. Dermaplaning
b. Dermabrasion
c. Cryosurgery
d. CO2 and argon laser
E. Cutaneous malignancies (e.g., basal cell carcinoma, squamous cell carcinoma) can lie within the rhinophymatous tissue
F. *Oral retinoids (isotretinoin/Accutane) should be discontinued 1 year prior to surgery as they impair re-epithelialization
PEARLS
1. If the blood supply to the columella is disrupted, the nasal tip relies on the lateral nasal arteries for blood supply
2. The forehead flap should become thicker when dissecting distal to proximal (subcutaneous to submuscular to subperiosteal)
3. The donor site of the forehead flap heals remarkably well by secondary intention.
4. The maximum rotation of a bilobed flap is 100 degrees
5. Defects of the nasal ala are best treated with a flap to prevent retraction and notching of the rim
QUESTIONS YOU WILL BE ASKED
1. What three things are required in all cases of nasal reconstruction?
Lining, support, and coverage.
2. What is the subunit principle of nasal reconstruction?
If 50% or more of a subunit is missing, then excise the remaining portion to achieve an optimal aesthetic outcome.
3. How far on either side of the midline is the supratrochlear artery located?
1.7 to 2.2 cm.
4. When should isotretinoin be discontinued in relation to nasal resurfacing procedures?
One year prior to surgery.
THINGS TO DRAW
Draw the nasal aesthetic subunits (Fig. 20.1).
Recommended Readings
Burget GC, Menick FJ. Nasal support and lining: the marriage of beauty and blood supply. Plast Reconstr Surg. 1989;84(2):189–202. PMID: 2748735.
Elliott RA Jr. Rotation flaps of the nose. Plast Reconstr Surg. 1969;44(2):147–149. PMID: 4895071.
Guo L, Pribaz JR, Pribaz JJ. Nasal reconstruction with local flaps: a simple algorithm for management of small defects. Plast Reconstr Surg. 2008;122(5):130e–139e. PMID: 18971686.
Menick FJ. The evolution of lining in nasal reconstruction. Clin Plast Surg. 2009;36(3):421–441. PMID 19505612
Millard DR Jr. Reconstructive rhinoplasty for the lower half of a nose. Plast Reconstr Surg. 1974;53(2):133–139. PMID: 4590746.
Rohrich RJ, Griffin JR, Adams WP Jr. Rhinophyma: review and update. Plast Reconstr Surg. 2002;110(3):860–869; quiz 870. PMID: 12172152.
Zitelli JA. The bilobed flap for nasal reconstruction. Arch Dermatol. 1989;125(7):957–959. PMID: 2742390.
< div class='tao-gold-member'>