Nail Surgery: Introduction
Patient Selection
Risks and Precautions
Preoperative photographs as well as any taken during surgery may be useful medicolegally. Careful history taking may reveal systemic disease such as diabetes mellitus, blood dyscrasia, vascular disease, vascular collagen disease (scleroderma), allergy, chronic pulmonary disease, or immune impairment. Any of these may at times be contraindications to surgery or may call for alteration of the technique to be used. Surgery of the nail is not recommended in patients with high-risk conditions. A history of concurrent use of drugs may be relevant, because these drugs may affect anesthesia (e.g., monoamine oxidase inhibitors or phenothiazines), prolong bleeding (e.g., aspirin and anticoagulants), delay healing (e.g., glucocorticoids), or have toxic effects on the nail apparatus (e.g., retinoids). There may be a history of allergy to lidocaine or mepivacaine or to parabens contained in both as a preservative. A knowledge of previous antitetanus immunization is important, because administration of tetanus toxoid may be advisable in association with surgery involving the toenail or traumatic lesions that come into contact with soil.
A magnifying lens may be useful to observe the color, surface, and structure of the periungual tissue and to compare the unaffected contralateral digit. It may be necessary to probe in order to localize pain, to obtain a radiograph to rule out underlying bone involvement, or to ask for ultrasonography and magnetic resonance imaging when a tumor is suspected.
Anatomy
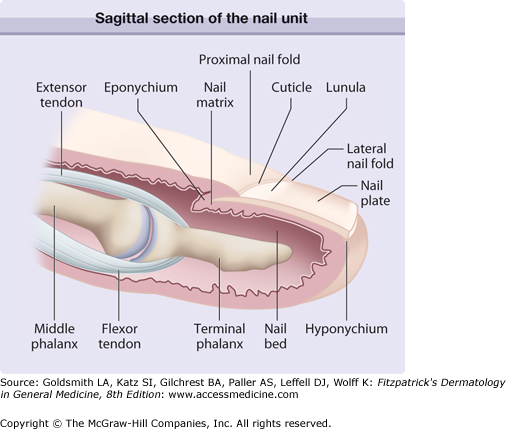
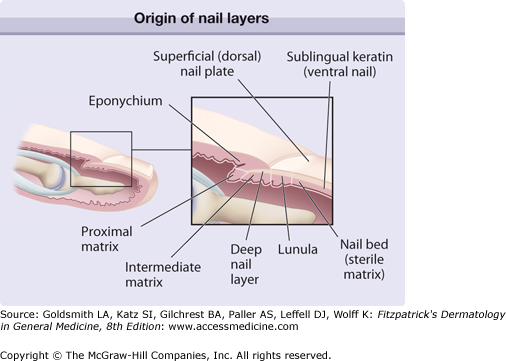
The nail plate is the permanent product of the nail matrix. Its normal appearance and growth depend on the integrity of the perionychium and the bony phalanx (Fig. 245-1). The nail is a semihard horny plate covering the dorsal aspect of the tip of the digit. The nail is inserted proximally in an invagination that is practically parallel to the upper surface of the skin and laterally in the lateral nail grooves. This pocket-like invagination has a roof, the proximal nail fold, and a floor, the matrix from which the nail is derived. The matrix extends approximately 6 mm under the proximal nail fold, and its distal portion is only visible as the white semicircular lunula. The general shape of the matrix is a crescent, concave in its posteroinferior portion. The lateral horns of this crescent are more developed in the great toe and are located at the coronal plane of the bone. The ventral aspect of the proximal nail fold encompasses both a lower portion, which continues the matrix, and an upper portion (roughly three-quarters of its length), called the eponychium (see eFig. 245-1.1). The germinal matrix forms the bulk of the nail plate. The proximal element forms the superficial third of the nail plate, whereas the distal element provides its inferior two-thirds. The ventral surface of the proximal nail fold adheres closely to the nail for a short distance and forms a gradually desquamating tissue, the cuticle, made of the stratum corneum of both the dorsal and the ventral sides of the proximal nail fold. The cuticle seals and protects the nail cul-de-sac.
The nail plate is bordered by the proximal nail fold, which is continuous with the similarly structured lateral nail fold on each side. The nail bed extends from the lunula to the hyponychium. It has parallel, longitudinal rete ridges.
In contrast to the matrix, the nail bed has a firm attachment to the nail plate. Colorless but translucent, this highly vascular connective tissue, containing glomus organs, transmits a pink color through the nail. Avulsion of the overlying nail plate denudes the nail bed.
Distally, adjacent to the nail bed, lies the hyponychium, an extension of the volar epidermis under the nail plate, which marks the point at which the nail separates from the underlying tissue. The distal nail groove, which is convex anteriorly, separates the hyponychium from the fingertip.
The circulation of the nail apparatus is supplied by two digital arteries that course along the digits and give off branches to the distal and proximal arches. The sensory nerves to the distal phalanx of the three middle fingers are derived from fine, oblique, dorsal branches of the volar collateral nerves. Longitudinal branches of the dorsal collateral nerves supply the terminal phalanx of the fifth digit and also the thumb.
Instruments and Draping
The instruments used in nail surgery are, in general, the same as those used in cutaneous surgery with the addition of the instruments listed in Box 245-1.
|
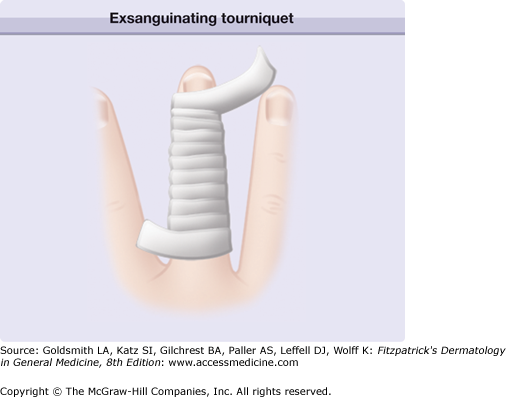
Draping is accomplished by means of a sterile glove on the involved hand. The tip of the glove is cut off on the finger that is to undergo surgery. The remaining open finger of the glove is then rolled back down the digit. This exsanguinates the digit and provides a tourniquet when it reaches the proximal part of the finger. For toenail surgery, the foot is draped in the usual aseptic manner with sterile towels secured by towel clamps.
Anesthesia
Local anesthesia should be administered while the patient is reclining or in a supine position. Lidocaine is widely used because the incidence of allergy to this agent is very low. Because the benefit of epinephrine is still debatable, it is preferable to use 2% lidocaine alone. A tourniquet can provide prolonged hemostasis when a bloodless operative field is required. It has been claimed that using tepid lidocaine minimizes the burning sensation associated with its administration. The use of one part 7.5% bicarbonate with nine parts lidocaine for the same purpose has also been advocated.
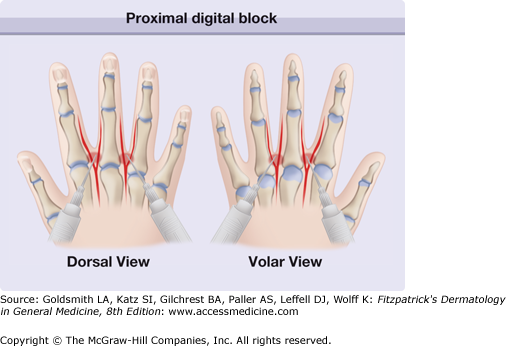
Anesthetics are administered via a 30-gauge needle on a Luer-Lok syringe using either a proximal digital block or a distal digital block (wing block) procedure. Other techniques, such as median distal anesthesia or transthecal block, have not replaced the classic routes of anesthesia. Although emergencies related to minor surgery occur rarely, the ready availability of resuscitative equipment and expertise is essential.
The proximal digital block procedure is less painful than the distal block procedure, but the anesthesia takes 5–10 minutes to become established. The hand is laid down flat, with the fingers spread, so that 1–2 mL of anesthetic can be administered by a dorsal injection, with a thin needle inserted and directed tangentially to the sides of the bony phalanx at the base of the involved finger and as far as the lateral side of the flexor tendon (Fig. 245-2). A tourniquet effect may inadvertently be produced by injecting more than 5 mL of anesthetic and should be avoided. The absence of blood reflux in the syringe should be verified before injection if a nondental syringe is used. When the operation is strictly localized to a lateral region, a block limited to the nerves ipsilateral to the lesion suffices, as in the case of a partial distolateral nail avulsion.
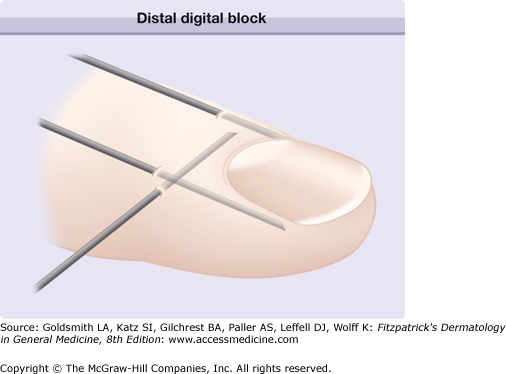
The distal digital block procedure is more painful than the proximal block procedure, but anesthesia occurs immediately. This method is absolutely contraindicated, however, when bacterial infection in the region is being addressed. The latter requires wrist block or general anesthesia.
For a distal digital block, the needle is inserted just behind the junction of the proximal nail fold and a lateral nail fold and a few tenths of a milliliter of anesthetic is injected, which whitens the region. The injection is continued by aiming the needle toward the pad. One then returns to the initial area to inject the proximal fold transversely. Finally, at the junction of the proximal fold with the lateral fold on the opposite side, one proceeds as described earlier (Fig. 245-3). The anesthesia is almost immediate, and when the procedure is done correctly, injections rarely have to be extended to the distal area of the finger.
Median distal administration is relatively simple and quick (Fig. 245-4). The needle is introduced at a 30-degree angle into the middle of the proximal nail fold and advanced distally into the underlying matrix. Anesthetic is injected slowly as the needle pierces first the nail plate, then the matrix, and finally the adjacent nail bed. The nail plate is soft and offers little resistance. Blanching confirms the delivery of anesthetic to the nail matrix and bed. Pain is brief and anesthesia nearly instantaneous. This method is suitable for most procedures performed on the proximal half of the nail unit. It is not suitable for matricectomy or complete nail avulsion.
The flexor tendon sheath may be used as an avenue for introducing anesthetic to the core of the digit. Through centrifugal anesthetic diffusion all four digital nerves are anesthetized rapidly. This technique involves palmar percutaneous injection of 2 mL of lidocaine into the potential space of the flexor tendon sheath at the level of the palmar flexion crease using a 3-mL syringe and a 25-gauge hypodermic needle.
There are several circumstances under which it is useful to have anesthesia of more than one digit at the same time. A wrist block may be appropriate in the surgical treatment of numerous warts and in the infiltration of more than one finger with triamcinolone in the treatment of nail unit psoriasis. This should be undertaken with the guidance of an experienced clinician.
Tourniquets
For brief intraoperative hemostasis (e.g., nail avulsion, punch biopsy of the nail bed), squeezing the sides of the digits is effective. If a prolonged bloodless field is required, a Penrose drain may be placed around the base of the digit and secured with a hemostat for use as a tourniquet. It is preferable not to leave it on for more than 15–20 minutes. The tourniquet application can be interrupted for a few minutes during longer procedures.
To complement anesthesia and facilitate establishment of a bloodless field, use of an exsanguinating tourniquet is recommended.1 A wide Penrose drain is wound tightly in loops that overlap in a distal to proximal fashion, with an exposed loose end left distally (eFig. 245-4.1). This “milks” the blood from the digit. The loose end is then grasped and the drain unwound, again from distal to proximal, until the nail unit is exposed with the final proximal loop.
Dressing and Postoperative Care
At the end of the operation, either the digit is cleansed with sterile 10% hydrogen peroxide solution and sprayed with a colorless disinfectant, or an antiseptic with hemolytic action is applied. The nail area is then covered with an antiseptic or antibiotic ointment on gauze or pads. Dressing must be done in a way that takes into account oozing, pain, and sensitivity. A bulky dressing provides a cushion against local trauma.
Dressings should be changed every other day or daily if there is infection. Several layers of sterile gauze should be kept in place by Micropore (2.5-cm) tape placed first on the dorsal aspect of the finger or toe, then on the ventral aspect, and last on the lateral edges in a U shape (a circular dressing should never be applied in the first week). Finally, use of an X-span tube dressing or Surgitube will give the patient more freedom to use the hand, but care must be taken that dressings do not constrict blood flow. During the first 48 hours the arm must be kept in a sling. Stitches are removed after 7–12 days.
Postoperative Complications
Bleeding is seen after the tourniquet is removed but can be stopped by compressing the lateral edges of the distal interphalangeal joint. In cases of persistent bleeding, 35% aluminium chloride solution or a cellulose application (Gelfoam) should be applied.
Pain threshold varies from patient to patient. Postoperative pain can be almost nonexistent if, in the absence of infection, the operation is followed by a periungual injection of 0.6 mL of 0.5% bupivacaine with 0.4 mL of 4 mg/mL dexamethasone. While the dressing is being put in place, the patient must be told what precautions to take. Providing a supply of moderately potent oral analgesics will help the patient feel in control of any pain, even if the patient chooses not to take the tablets. Sometimes postoperative pain may be severe, and it is alleviated by elevating the extremity as much as possible for 2 days. Pulsating pain beginning after 36–48 hours may indicate an infection, which should be treated according to the results of bacterial culture of the organism. Any bulky dressing that is blood stained after 24 hours should be changed.