Fig. 14.1
Half-and-half nails. Seen here are the classic changes of half-and-half nails associated with renal failure. Visualization of the lunula is lost; the proximal nail appears white compared to the darker distal area. (Courtesy of Julia R. Nunley, M.D.)
Leukonychia, transverse: Leukonychia transverse is a frequently noted nail pathology that can be observed in patients with acute or chronic renal failure as well as renal transplant recipients. It is characterized by the presence of a white single 1–2 mm wide transverse nail plate band. Leukonychia has also been described in patients with acute arsenic toxicity (Mees lines), hepatic cirrhosis, and in association with immunosuppressive medications such as cyclosporine and prednisolone [19]. Other associated conditions include human immunodeficiency virus (HIV) infection, sickle cell anemia, pellagra, nail damage from handling paraquat, and during the course of various chemotherapeutic agents [17, 25–27]. Leukonychia is believed to result from abnormal keratinization of the nail plate [17] (Fig. 14.2).


Fig. 14.2
Transverse leukonychia. (Springer Berlin Heidelberg, Color Atlas of Nails, 2010, 45–61, Tosti A, et al.)
Nail-patella syndrome (NPS): NPS is a rare autosomal dominant disorder with a reported incidence of 1 in 50,000 live births [28, 29]. Sporadic occurrence accounts for approximately 20 % of the cases and because of the dominant type of inheritance, the children of affected individuals have a 50 % chance of developing the disease [28]. NPS is caused by loss-of-function mutations in the LMX1B gene linked to the distal end of the long arm of Chromosome 9 in the region 9q 34. Animal studies have shown that the LMX1B gene plays an important role in the dorsal-ventral pattering of limb development, morphogenesis and function of the glomerular basement membrane, as well as the development of the anterior segment of the eye [18]. Classical NPS involves nails, bone abnormalities of patellae, elbow, iliac, and less frequently renal and ocular involvement. Clinical manifestations can be observed during childhood or adolescence. Nail anomalies have been reported in up to 95 % of NPS patients [28]. Nail dysplasia and patellar aplasia or hypoplasia are the most commonly encountered nail abnormalities and are essential features for diagnosis. Nail dystrophy is more pronounced in the fingernails, and patellar abnormalities which may be asymmetrical can be present in up to 90 % of affected individuals [29]. Nail dysplasia is usually present at birth. A pathognomonic sign for NPS is the presence of triangular nail lunulae. The thumbs are more severely affected and the degree of involvement usually decreases progressively from the thumb to the 5th digit. Toenails are rarely affected. Skeletal abnormalities associated with NPS frequently involve the pelvis, elbow, and feet. A pathognomonic sign for NPS is the presence of iliac horns which are triangular bony protuberances of the posterior ilium and is found in 70–80 % of patients [28, 29]. They are located at the side of attachment of the gluteus medius muscle and project posterolaterally. Approximately 70 % of patients with NPS exhibit some degree of elbow involvement which can include limitation of extension, pronation and supination, cubitus valgus, and antecubital pterygia. Other skeletal abnormalities include rib hypoplasia, clubfoot deformities, shoulder girdle dysplasia, scoliosis, clavicular horns, and affected patients are also predisposed to increased incidence of fractures [29]. Ocular involvement includes open angle glaucoma and ocular hypertension. Renal involvement occurs in about 30–60 % of patients and presents with proteinuria and/or microscopic hematuria, edema, and hypertension. Renal involvement is the most serious aspect of NPS, as it can progress to nephrotic syndrome in up to 20 % of patients, and about 10 % of patients will progress to renal failure requiring subsequent renal replacement therapy, e.g., dialysis or renal transplantation [29]. Renal biopsies reveal nonspecific microscopic findings mostly related to the degree of renal failure, including focal and segmental sclerosis, proliferative glomerulonephritis with crescent formation with the only consistent histopathological feature being the focal thickening of glomerular basement membrane [28]. Under the electron microscope, the glomerular basement membrane appears irregularly thickened with electro-lucent areas giving the typical “moth-eaten” appearance [29]. Within the glomerular basement membrane and the mesangium, cross-banded fibrillar collagen-like material has been found in patients with glomerular involvement but not associated with nail or skeletal abnormalities. At the present time, conservative management of proteinuria and hypertension with angiotensin-converting inhibitors and angiotensin receptor blockers is indicated. Renal transplantation is considered a viable therapeutic modality in patients with end-stage renal failure as the disease may not recur in the transplanted kidney [29].
Digital clubbing and Pseudoclubbing: Clubbing is an overcurvature of the nails in the transverse and longitudinal axes with preservation of the angle between the nail palate and the proximal nail fold (Lovibond angle). Such an angle is usually less than 160°. In clubbing, this angle exceeds 180°, while in pseudoclubbing, it is less than 180° [30]. Clubbing was first described in the first century BC by Hippocrates and has been commonly described with pulmonary diseases, cyanotic heart disease, liver cirrhosis, but it can also be due to congenital causes and in some instances, it is idiopathic [31]. Both digital clubbing and pseudoclubbing have been described in patients with secondary hyperparathyroidism due to chronic renal failure [30–32]. Pseudoclubbing has been reported to occur in 0.6 % of dialysis patients [32] and can manifest as painful digits tender to palpation. In contrast to clubbing which tends to be symmetrical, pseudoclubbing usually presents as an asymmetric involvement of the fingers. Radiographically, there is resorption of the terminal tufts, i.e., acro-osteolysis. Other known associations include thyroid carcinoma, primary hypothyroidism, sarcoidosis, subungual hemangioma, scleroderma, and certain chromosome anomalies [33–39] (Fig. 14.3).
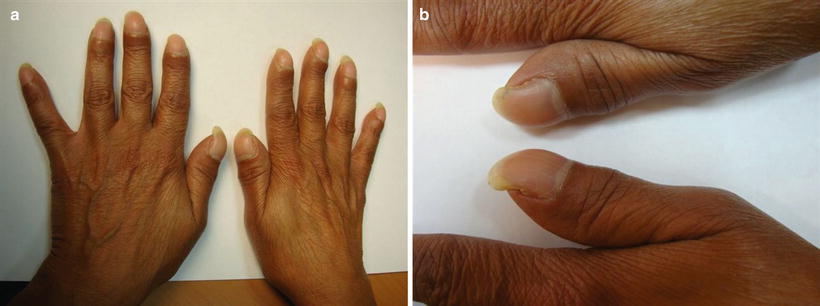
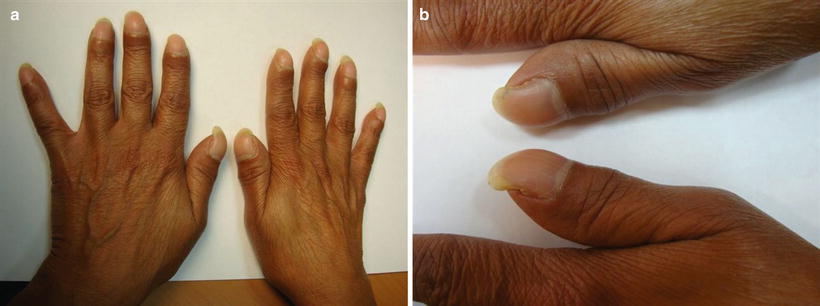
Fig. 14.3
Clubbing
Hemodialysis
Nail diseases in patients on maintenance hemodialysis are common and may affect from 52 to 71.4 % of patients [17, 40]. The most frequent onychopathy observed in hemodialysis patients include half-and-half nail, absence of lunula, splinter hemorrhage, and onycholysis [17–19].
Half-and-half nail: Half-and-half nail is the most common nail abnormality observed among hemodialysis patients with an estimated frequency that varies between 15 and 50.6 % among different series [41–45]. In half-and-half nails the proximal half of the nail is white, while the distal portion is reddish-brown. Generally, 20–40 % of the nail surface is affected [20]. There has been no demonstrable association between the dose and duration of hemodialysis and frequency of half and half nail [17, 19, 44, 46]. Some studies have shown that half-and-half nails can completely disappear after successful renal transplantation [17, 41]. The exact cause of this nail disorder remains unclear. For more detailed reference regarding half-and-half nail, see the section “Renal Failure” (Fig. 14.1).
Absent lunula: It is characterized by the absence of the visible portion of the nail matrix, and has been associated with metabolic disturbances as well as anemia related to underlying chronic renal failure [17, 47]. Absent lunula can also be found as a normal variant especially among people of Africo-Caribbean and Caucasian decent [6, 19, 40] but hemodialysis patients have a higher rate of occurrence compared to the general population. It has also been demonstrated to occur at any time during the course of chronic renal failure progression to end stage renal disease [17, 19] (Fig. 14.4).
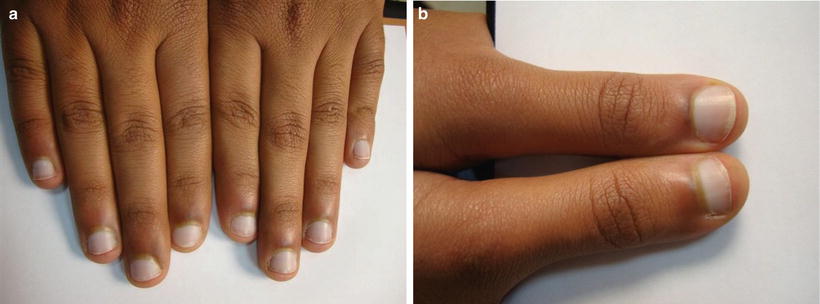
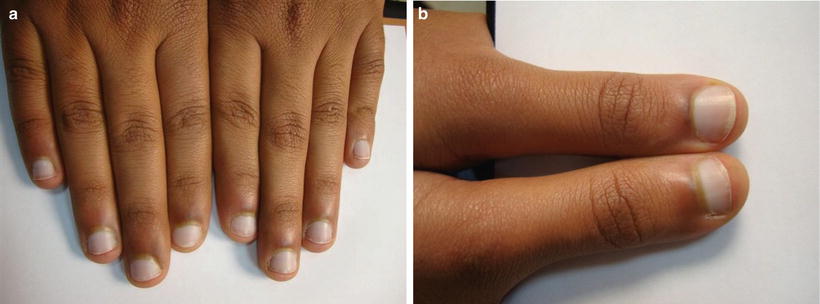
Fig. 14.4
Absence of lunula
Splinter hemorrhages: These appear as dark red, filiform, longitudinal lines in the distal region of the nail plate. Splinter hemorrhages can be seen in patients on hemodialysis or peritoneal dialysis and have been reported to occur with a prevalence of up to 20 % [17, 19]. Longer duration of dialytic therapy is not associated with the occurrence of splinter hemorrhages [11]. In hemodialysis patients, splinter hemorrhages are believed to result from microtrauma [17, 19]. The exact pathogenesis remains unclear but capillary fragility and thrombocyte dysfunction has been implicated in the development of splinter hemorrhages [17, 19]. They have also been reported in chronic glomerulonephritis, e.g., focal segmental glomerulosclerosis. Other associations include bacterial endocarditis, antiphospholipid antibody syndrome, trichinosis, onychomatricoma, and external trauma [46] (Fig. 14.5).
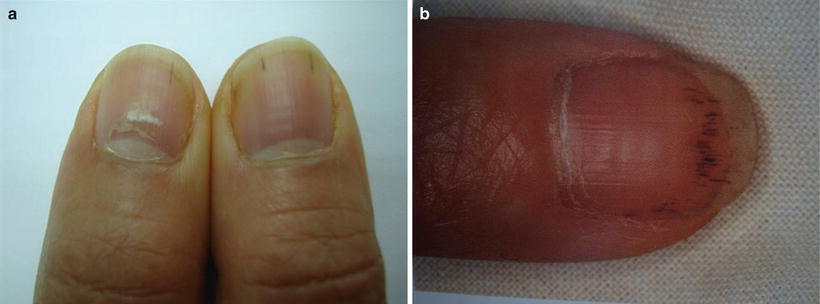
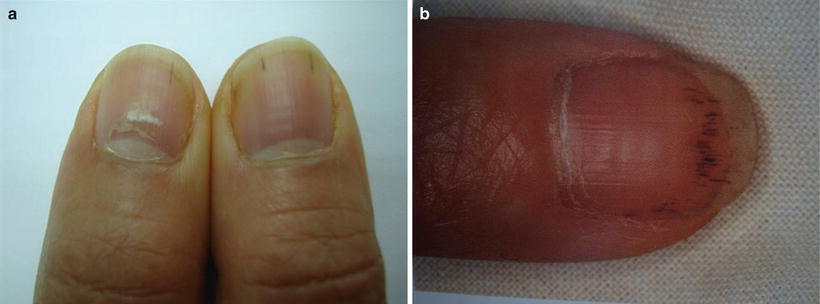
Fig. 14.5
Splinter hemorrhages
Onycholysis: Normally, the nail plate adheres strictly to the nail bed and this represents as an anatomical barrier. Its disruption results in nail plate detachment with onycholysis. Onycholysis is commonly seen in hemodialysis patients and can result from different local and systemic causes. Captopril has been described to induce reversible onycholysis [48, 49]. Medications causing photosensitivity can induce photo-onycholysis which has been described in hemodialysis patients receiving large doses of cephalordine or cloxacillin [50, 51] (Fig. 14.6).


Fig. 14.6
Onycholysis
Brittle nails: Brittle nails are alteration of the nails consistency and have been associated with up to 11.7 % of hemodialysis patients [19, 40]. Etiological factors associated with brittle nails include hypochromic anemia [40], malnutrition, peripheral vascular disease, and low circulating levels of iron and zinc [52] (Fig. 14.7).


Fig. 14.7
Brittle nail
Onychomycosis: Onychomycosis has a high prevalence among patients on maintenance hemodialysis. The frequency of onychomycosis in this population can range between 6.2 and 52 % [17, 44, 43, 53]. This may be due to impaired cellular immunity characterized by lymphopenia, decreased B-cell activity, and alteration of T-cell subsets [44]. The most common pathogen isolated in affected patients was Trichophyton rubrum followed by Trichophyton mentagrophytes, Scytalidium dimidiatum, and Candida species [44, 53]. Dermatophytes are more frequently isolated from the toenails whereas Candida species from the fingernails. Increase of the dialysis duration and presence of diabetes mellitus are known factors for occurrence of onychomycosis [53] (Fig. 14.8).
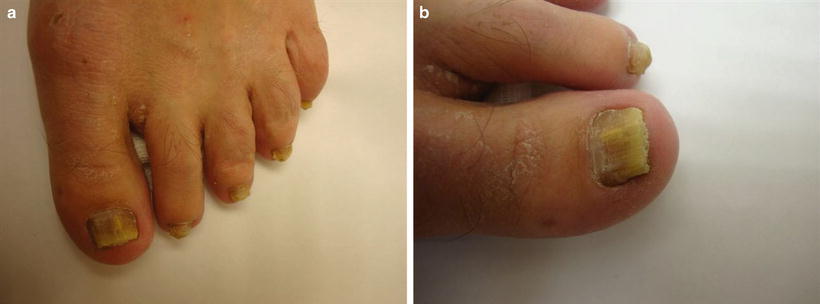
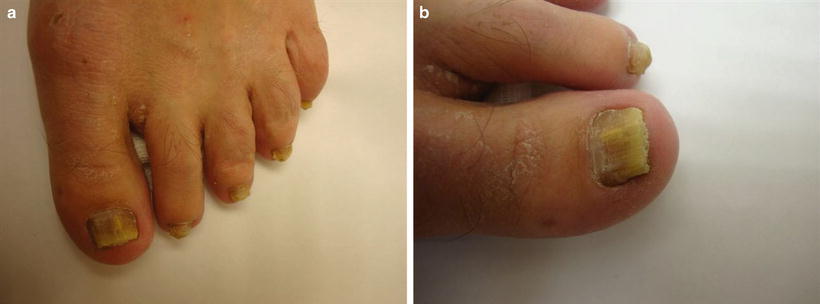
Fig. 14.8
Onychomycotic toenails
Renal Transplantation
A high incidence of nail changes among renal transplant recipients has been reported with an overall frequency of 56.6 % [17]. Nail pathology increases with age and with longer duration of immunosuppressive therapy [17]. The most commonly encountered nail changes are leukonychia, absence of lunula, onychomycosis, longitudinal ridging, and Muehrcke lines [6, 17]. Absence of lunula and longitudinal ridging are also frequent [6]. The occurrence of splinter hemorrhage and half-and-half nails is much less in renal transplant patients as compared to those on maintenance dialysis.
Leukonychia: Leukonychia has been shown to have increased prevalence rates in renal transplant recipients as compared to the general population [6] and is the most common nail pathology in this population [17]. It is characterized by the presence of a single 1–2 mm wide transverse white nail plate band. It has been documented to occur also in association with acute and chronic renal failure, hepatic cirrhosis, exposure to various medications, exposure to toxins, HIV infection, and during the course of various chemotherapy protocols [25–27, 54, 55]. Leukonychia is thought to result from abnormal keratinization of the nail plate [17]. For more detailed reference on leukonychia, see the section “Renal Failure” (Fig. 14.2).
Absence of lunula: There is increased frequency of absent lunula among renal transplant patients [6]. It is characterized by the absence of the visible portion of the nail matrix. Several other diseases have been associated with absence of lunula such as atherosclerosis, chronic obstructive pulmonary disease, and rheumatoid arthritis [6]. Absence of lunula was particularly observed with increased frequency in older renal transplant recipients. Interestingly, such increased prevalence was not related to duration of immunosuppression or any treatment protocols [17] (Fig. 14.4).
Superficial fungal infections: A significantly higher incidence of opportunistic infections such as superficial fungal infections, e.g.,Pityrosporum ovale and Candida albicans have also been noted with increased frequency in renal transplant recipients [6, 17]. The increased incidence of mycologically proven onychomycosis and superficial fungal infections in renal transplant recipients can be explanted on the basis of decreased cell-mediated immunity brought about by immunosuppressive therapy [6, 17]. Pityriasis versicolor is the most common isolated fungal infection followed by oral candidiasis, onychomycosis, and interdigital toe-web infection [55]. Trichophyton rubrum is the most common dermatophyte causing tinea unguium in this population [6, 56–58]. Some studies however, have shown Trichophyton mentagrophytes to be quite common [59, 60] (Fig. 14.8).
Muehrcke nail: Muehrcke lines are paired white transverse lines that have been seen in renal transplant recipients, end-stage renal failure, and Hodgkin disease [6]. It is believed to be caused by localized edema involving the nail bed thereby applying pressure to underlying vasculature, resulting in a decreased erythema of the nail bed [61].
Drug-induced onychopathy: Sirolimus is an immunosuppressive drug used commonly in renal transplantation as well as in rheumatoid arthritis. Dermatological side effects associated with sirolimus include edema, acne, aphthous ulceration, and vasculitis [62




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








