CHAPTER 11 Müller’s Muscle–Conjunctival Resection–Ptosis Procedure Combined with Upper Blepharoplasty
Patients often present for cosmetic rejuvenation of the upper periorbita and the examination reveals both dermatochalasis and upper eyelid ptosis. In these situations it is both possible and preferable, to combine an upper blepharoplasty with ptosis surgery. Although this technique is commonly performed through an external approach with levator aponeurosis advancement or resection, many cosmetic surgeons do not appreciate the possibility of combining an internal Müller’s muscle–conjunctival resection with an external upper blepharoplasty, especially when the skin and orbicularis oculi muscle are excised and an eyelid crease is reconstructed.
The Müller’s muscle–conjunctival resection–ptosis procedure, described in 1975 by Putterman and Urist, is a technique in which Müller’s muscle in the upper eyelid is partially resected and advanced.1 The exact mechanism by which the correction of ptosis is achieved is probably due to a number of effects that include resection and advancement of Müller’s muscle as well as the secondary effects of advancing the levator aponeurosis to the superior tarsal border. The classic approach to the treatment of a variety of lid ptosis presentations has been mostly through variations of an external (skin-muscle incision) approach through the upper eyelid crease whereby the anatomic ‘defect’ is visualized and presumably repaired (see Chapter 10). This approach, however, more often requires the cooperation of the patient during the surgical procedure and heralds a host of potential variabilities that include, but are not limited to, sedative effects, local anesthetic effects, edema, and performance anxiety on both the patient’s and surgeon’s part. To the contrary, the Müller’s muscle conjunctival resection can be performed with continuous IV sedation or even general anesthesia as it does not require intraoperative patient cooperation. The procedure is used to treat a variety of upper eyelid ptosis and can be combined with an upper blepharoplasty with or without crease reconstruction via a skin flap or a skin-muscle flap approach. The procedure has the many advantages over other ‘posterior approach’ lid ptosis procedures and the external approaches that includes the preservation of upper eyelid tarsus (which creates less risk of suture-induced keratopathy and theoretically preserves structural and functional aspects of the upper eyelid), repositions the elevated (involutional) eyelid crease to a lower positioned and more youthful level, and can more predictably improve upper eyelid position (MRD) and contour. In addition, the usual skin-muscle and fat excision that is performed for a host of reasons, including adequate exposure to the levator aponeurosis (that can be volume depleting to the upper eyelid), can be avoided if desired. There also is rarely a need for additional surgery to treat residual ptosis or overcorrections. This procedure that was originally felt to be effective mostly in individuals with only mild to moderate upper eyelid ptosis and/or had a positive response to neosynephrine eye drops, can in fact be applied in most all types of ptosis presentations.
Diagnosis and preoperative evaluation
MRD1 test
The MRD1 measurement is used to assess the upper eyelid levels (see Chapter 3, Fig. 3-8). It should be performed both before and during the phenylephrine test.
Phenylephrine test
Side effects, such as myocardial infarction and hypertension, have been reported after instillation of phenylephrine drops,2 but are exceedingly rare. Therefore, it is important to determine that the patient does not have a significant cardiac risk before the phenylephrine test is performed. In our collective experience this has, however, rarely posed a problem but if there is ever a significant concern then the patient’s primary care physician or cardiologist should be consulted.
Glatt and Putterman3 have compared test results using 2.5 percent and 10 percent phenylephrine. It appears that both solutions are effective in determining candidates for the Müller’s muscle–conjunctival resection procedure, but that the 2.5 percent solution may theoretically result in fewer vasoactive side effects. Our experience has been primarily with the 10 percent solution. Patients should be warned regarding the likely pupillary dilation after this test which may yield transient photophobia and visual blurring. If there is a history of glaucoma, it may be prudent to contact their ophthalmologist regarding any concerns of pupillary dilation. Finally, regarding other symptomatology after these tests, it is not uncommon for patients to experience transient ocular irritation that might relate to dryness or exposure symptoms and indicate to the surgeon the possibility of dry eye symptoms after surgery.
Surgical technique
Anesthesia
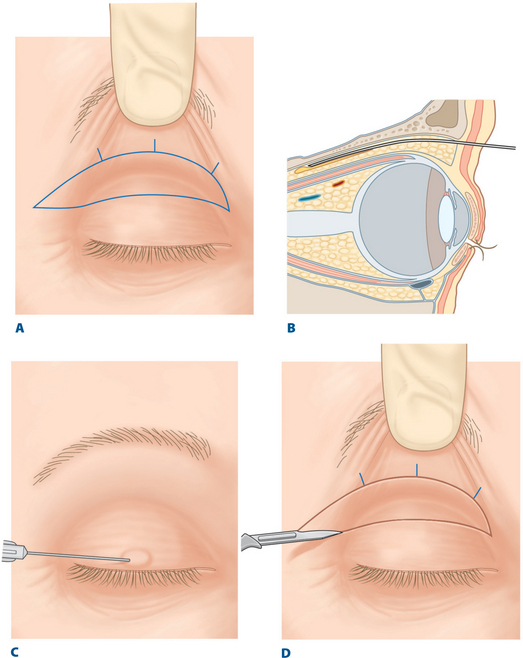
Local anesthesia is preferred in adults. The upper eyelid skin to be removed is marked according to the technique for upper blepharoplasty with crease reconstruction (see Chapter 7) or without crease reconstruction (see Chapter 8) (Fig. 11-1A). A frontal nerve block is used with local anesthesia to avoid swelling and bruising of the upper eyelid by local infiltration, which would make the operation more difficult and inexact.4