CHAPTER 15 Lower Blepharoplasty: Blending the Lid/Cheek Junction with Orbicularis Muscle and Lateral Retinacular Suspension
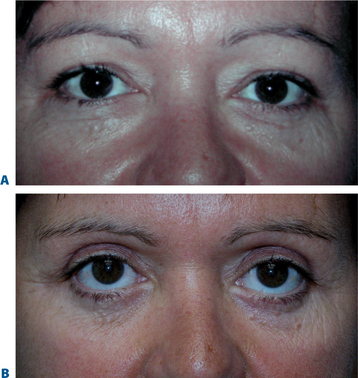
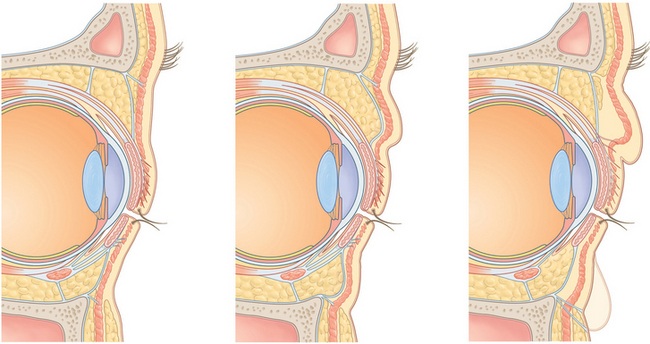
Similar to many facial aesthetic procedures, the current methods used in lower blepharoplasty have evolved for many reasons, including the lack of satisfaction with previous methods, complications arising from traditional surgical approaches, a better understanding of the anatomy of the aging periorbita and appreciation of the components of youth. Traditional lower blepharoplasty, for instance, performed 20 years ago typically incorporated a lower eyelid, infraciliary skin/muscle flap and excision of orbital fat through this incision by violating the orbital septum and performed without routine canthal reinforcement. The surgical efforts were basically a perceived solution to the antiquated notion of getting rid of ‘excess’ soft tissue (skin, muscle, and fat) in addition to straightforward access to lower eyelid fat without regard for the concurrent senescence of supporting structures. Depending on the patient’s presentation as well as the aggressiveness of the surgical procedures, a varying degree of lower eyelid malposition was met, and fortunately dissatisfaction of the overall appearance of the lower periorbita was uncommon. Patients could usually detect an overall improvement (‘bags were gone’) of their appearance and often accepted a varying degree of lid malposition, hollowness, and scarring as routine (Fig. 15-1). These results were often published with great pride, as the perception of the improvement in the few noted areas and the lack of options available fostered the acceptance of these results. Even the most noted surgeons were achieving these results and many were complacent that this was ‘the best that could be done.’
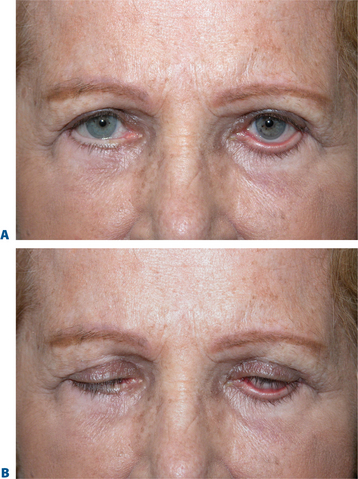
The emergence of a greater appreciation of the ‘oculoplastic surgeon’ to a large degree emanated from referrals by these noted surgeons whose patients experienced eyelid changes that were outside the acceptable range (lid retraction, ectropion, lagophthalmos, onset or exacerbation of long-term dry eye symptoms, etc.) (Fig. 15-2). Based primarily on the ophthalmologist’s exposure to periorbital anatomy and lower eyelid reconstruction, repair of lid malposition and the like were accomplished via procedures to horizontally tighten or shorten the lower eyelid to better position the eyelid/globe interface and effectively aid lower eyelid posture. The improvement of sometimes disastrous situations was appreciated despite the reality that the lid changes could rarely be fully restored (Fig. 15-3). Surgeons who treated these problems usually incorporated techniques such as the lateral tarsal strip1 or other methods that shortened the lower eyelid horizontally2 in an attempt to reduce vertical lower eyelid distraction by increasing horizontal lid tension. The improvement was notable and became the accepted standard of care. These procedures, in most cases however, might have been avoided if a lower eyelid/canthal reinforcement was performed at the time of the initial surgery. Why, however, were these latter procedures not routinely performed?
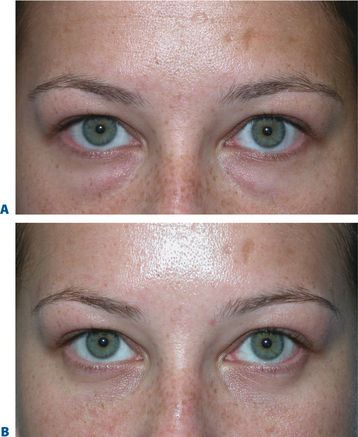
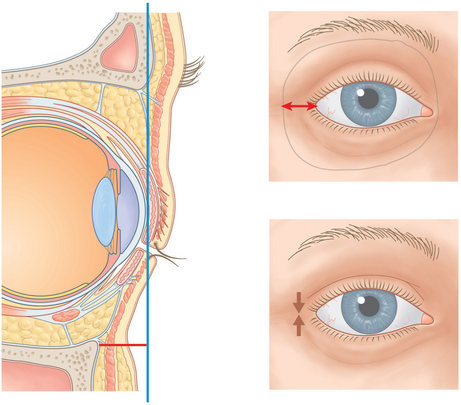
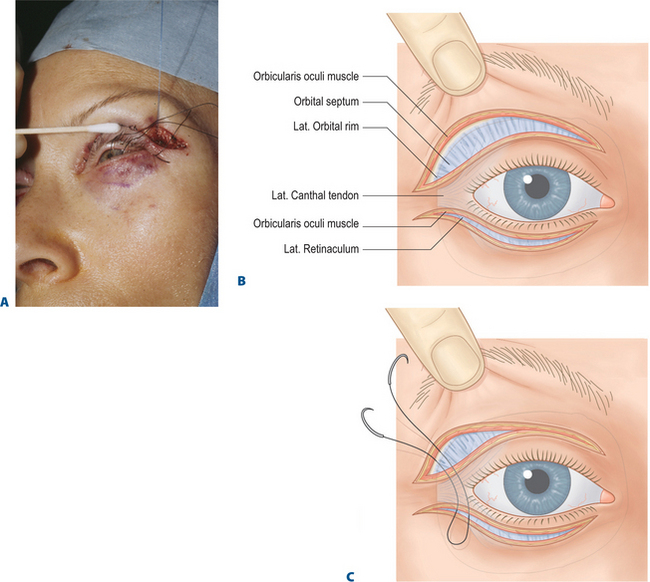
One possible explanation for the avoidance of routine canthal support is that the anatomy of the lateral canthus and traditional canthal reinforcement procedures are both complex to understand and the reconstruction of the lower eyelid and lateral canthus commonly heralded complications including asymmetry, canthal misalignment and eventual shortening of the horizontal palpebral aperture after fixation was lost. Instead of incorporating methods that were proactive in supporting the lower eyelid, many surgeons either avoided lower blepharoplasty, accepted varying mild to moderate degrees of eyelid malposition, or adopted other procedures that were suboptimal in restoring the youthful complement. The transconjunctival approach to removal of lower eyelid fat then became popular due to the negligible change in lid position,3 while at the same time improving lower eyelid ‘bags’ (Fig. 15-4). Except for the rare very young individual with good soft tissue tone and elasticity, the improvement of the lower eyelid ‘bulges,’ however, were often met with worsening of the appearance of the lower eyelid skin surface, either relating to a deflationary effect and diversion of attention from bags to lower eyelid skin/soft tissue quality. It is my opinion that for all the wrong reasons, laser skin resurfacing of this region then became more popular, combined with transconjunctival removal of fat, in order to improve the appearance of the skin.4 This anatomic and surgical oversimplification (volume depleting the lower eyelid by fat removal combined with exfoliating the skin) can produce significant improvement to the appearance of the lower periorbita.5 I too employed this procedure earlier in my practice and realized that with significant degrees of application of laser energy to improve lower eyelid skin appearance, eyelid retraction was at the very least temporary, and canthal support (via a simple suture canthopexy without surgical release) could maintain or improve the lower eyelid posture. While I was not convinced that horizontal shortening type procedures like the lateral tarsal strip were prudent in such situations, I explored the ability to effectively suspend the lateral canthus via suture, hopefully in a way that was better than prior attempts at suture canthopexy6 (Fig. 15-5).
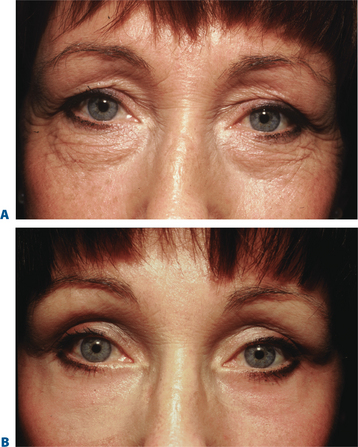
This was obviously not the first suture canthopexy procedure developed. One glimpse at the 1993 issue of Clinics in Plastic Surgery edited by Dr Robert Flowers7 reveals the current thinking on a spectrum of canthal support procedures. Most suture suspension procedures were considered unsatisfactory, with the exception of those that required minimal support (usually in the younger patient) as it was felt that loss of fixation (long-term) was inevitable. Techniques evolved and were modified8 that included the incorporation of drill holes through the lateral orbital rim for individuals where either periosteum in this region was deemed inadequate,7 or where it was presumed that failed canthopexy often related to a point of disinsertion. On the other hand, I felt that good periosteal purchases (fixation) were likely to be more long lasting than the entrance of the suture (below) through the lateral canthal ligament.6,9 The lateral retinacular suspension was essentially another variety of suture canthopexy, whereby the canthal system was reinforced by a suture suspension that was delivered through a lower eyelid incision with the opportunity of using variable vectors of support by exiting the suture through the upper eyelid at a multitude of levels (Fig. 15-6). It seemed clearer to me later that with ongoing orbicularis muscular function at the lateral canthus with subconscious and frequent animation, that the likely point of eventual disinsertion would be here at the lateral commissure rather than at the periosteum at the orbital rim. While I recognized the need for some sort of canthal support in patients undergoing CO2 laser skin resurfacing to the lower eyelid and canthus, I was then unsure of how long the supportive effects could be expected. I began incorporating a lateral retinacular suspension procedure routinely with my laser skin resurfacing procedures to the lower eyelid through a 2–3 mm incision at the lateral commissure (Fig. 15-7). I found that reinforcing the polypropylene suture with Vicryl sutures (see p. 171) at the commissure either reduced or slowed down the disinsertion at the lateral canthal tendon and often many months (even years) later found that the suture was still attached to the lateral orbital rim. As this maneuver aided my many patients who had undergone laser skin resurfacing, I then began to extend the lateral retinacular suspension procedure to skin flap lower eyelid surgery which has been the mainstay of my lower blepharoplasty to date.
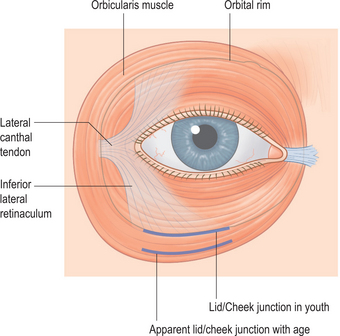
It has also been my opinion that despite the fact that skin quality appearance could be improved by laser skin resurfacing, the aging pathology of the lower periorbita as well illustrated by Drs Harris and Mendelson in their facial anatomy chapter in this book (see Chapter 5) and other writings10,11 indicates that it rests greatly on the orbicularis muscle and its retaining ligaments (Figs 15-8, 15-9). I believe this is due to a complicated combination of life-long animation, descent and hypotonia of the orbicularis, and atrophy of the adjacent periorbital soft tissue (skin, subcutaneous fat, ligamentous attachments) that allows the lower orbital fat to be anteriorly displaced combined with radial expansion of the soft tissues which better explains the lower periorbital ‘bulges’ (Fig. 15-10). As I believe that laser skin resurfacing was an abbreviated remedy, I also realized that skin–muscle flap surgery was often ineffective in significantly improving the lower eyelid skin. In lieu of this, I began re-exploring the use of skin flap dissection in an attempt to create an advancement flap of skin only (that contracts as do all advancement flaps) which would hopefully improve the lower eyelid skin rhytids and overall appearance. This plane of dissection also interrupts the attachments of orbicularis to the deep dermis which is a component of the cause of lower eyelid rhytids. Combined with adequate stabilization of the lower eyelid and lateral canthus via effective canthopexy and orbicularis muscle suspension, the skin tightening improved its appearance without inducing lid malposition. After many procedures utilizing this technique, it became clearer to me that this approach could improve lower eyelid skin appearance, at times to the same degree as laser skin resurfacing. The advantage of this approach also allowed me to expose the orbital component of the orbicularis oculi muscle throughout the lower eyelid and at the lateral canthus for further rejuvenative refinement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree