CHAPTER 18 Treatment of Lower Eyelid Retraction with Recession of Lower Lid Retractors and Placement of Hard-Palate or Allogeneic Dermal Matrix Spacer Grafts
Treatment of lower eyelid retraction is common in patients with thyroid ophthalmopathy. It may also occur as a complication of previous blepharoplasty procedures, both cosmetic and functional. Treatment consists of recessing the lower lid retractors and placing a spacer between them and the inferior tarsal border. Present options include hard-palate grafting for the spacer because (1) it provides a mucous membrane lining to the internal lower lid; (2) it is rigid and flat; and (3) it is autogenous. A useful alternative however is using an allogeneic spacer graft to avoid issues relating to harvesting and also to reduce operative time.
A lower internal blepharoplasty along with lower retraction surgery is commonly performed. This approach differs slightly from the transconjunctival approach to resection of lower eyelid herniated orbital fat (see Chapter 14), in that the retractor incision is made at the inferior tarsal border rather than 5–6 mm inferior to the inferior tarsal border.
Most patients who present with dissatisfaction after lower blepharoplasty complain or have symptoms related to lower eyelid malposition combined with a more ‘round’ appearance to the eye that is secondary to an increased vertical palpebral aperture and a shortened horizontal aperture. Often, mild to even moderate degrees of lower eyelid retraction need not be addressed depending upon the patient’s concerns, desires and expectations. Frequently, lower eyelid retraction is minimal and can be ignored. If, for instance, the patient with thyroid disease undergoes an orbital decompression for treatment of exophthalmos, the eye will commonly descend, thus making the lower eyelid retraction less apparent. If the retraction is moderate to severe and a decompression is not in the picture, the lower eyelid retraction should be treated. If a patient presents with lower eyelid retraction after blepharoplasty that is mild and without symptoms, they may have options for correction that are dependent upon what they are willing to endure regarding the surgical procedure, recovery, and final result.
Another method involves measuring the distance from a light reflex that is made to shine on the cornea to the lower lid as both patient and examiner look in the primary position of gaze, that is, the margin reflex distance-2 (MRD2) (see Chapter 3, Fig. 3-9).1 Normally, the lower eyelid rests at the inferior limbus. Measurements of retraction greater than 2 mm may be enough to warrant retraction surgery.
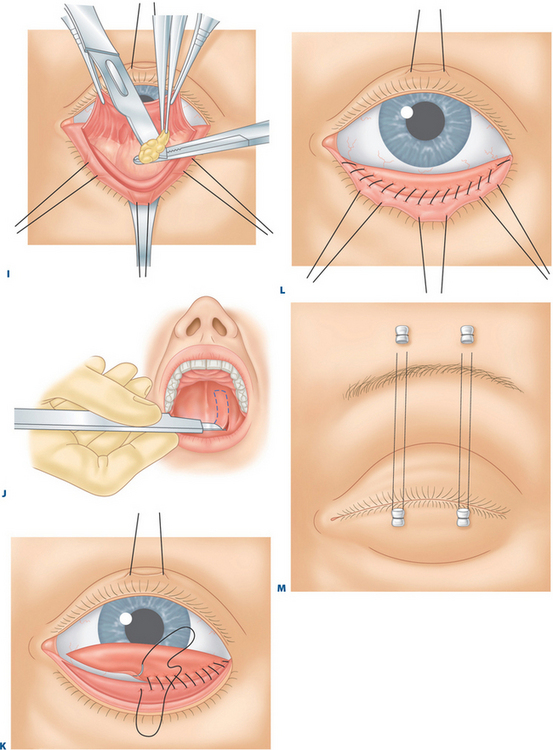
Preparation before surgery (with the implementation of a hard palate graft)
At some time before surgery, it is our preference when a hard palate graft is the chosen spacer graft, to work with a dentist who constructs a custom-fitted plastic plate that will fit onto the roof of the patient’s mouth.2,3 This plate is attached to several teeth with extensions that come off the plastic plate. After retrieval of the hard-palate grafts and the placement of an absorbable gelatin sponge (Gelfoam) to the donor site, the plastic plate is inserted onto the roof of the mouth. The plate provides comfort and maintains hemostasis.
Surgical technique
Hard palate harvesting and grafting
Local anesthesia with intravenous sedation is usually used. Topical tetracaine is applied over the eye. A corneo-scleral contact lens is placed over the eye and under the upper and lower eyelids to protect the eye and minimize the patient’s discomfort from the operating lights. The patient is prepared and draped in the usual fashion, similar to that used for upper or lower blepharoplasty (see Chapters 7, 14 and 16). The mouth is prepared with povidone-iodine (Betadine) sponges rubbed over the teeth, hard palate, and tongue surface.
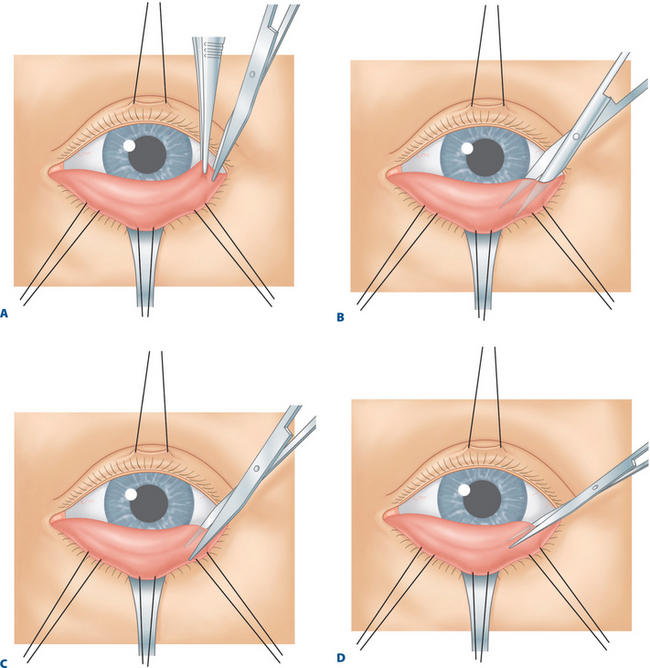
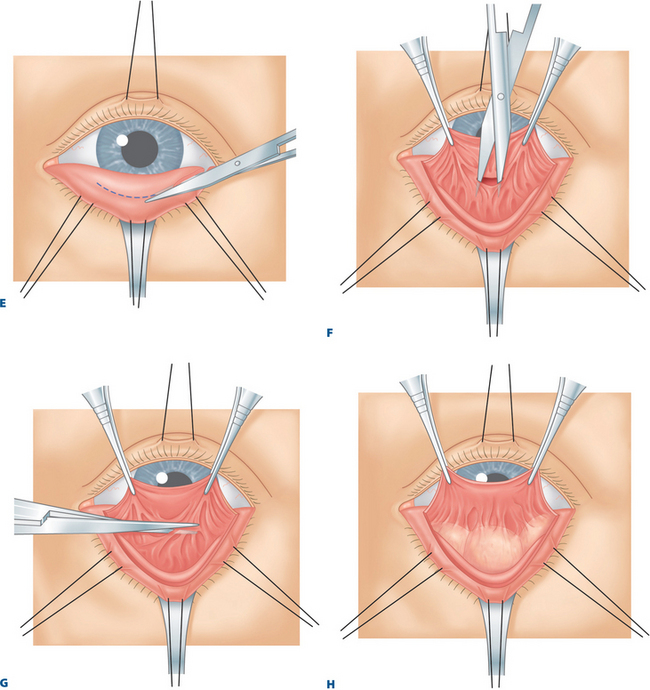
Recessing the lower eyelid retractors
A toothed forceps grasps the conjunctiva, Müller’s muscle, and the capsulopalpebral fascia at the temporal aspect of the eyelid, just beneath the inferior tarsal border (Fig. 18-1A). With a Westcott scissors, the surgeon penetrates this tissue and severs it from the inferior tarsal border. The Westcott scissors enters this opening and passes between capsulopalpebral fascia and orbicularis muscle across the eyelid (Fig. 18-1B). The surgeon facilitates this maneuver by separating the Westcott scissors blades during the passage and by pulling the scissors upward toward the conjunctival surface. At the same time, the surgeon’s assistant is releasing the Desmarres retractor slightly or pulling the skin surface outward. Because skin (and scar tissue in previously operated lower eyelids) is firmly attached to the orbicularis muscle and the conjunctiva is firmly attached to Müller’s muscle and capsulopalpebral fascia, the two lamellae separate in opposite directions during this maneuver.