Fig. 28.1
Corpse dissection of a transverse rectus abdominis myocutaneous (TRAM) flap: scissors are collocated behind the superior pedicle and the flap is rotated toward the chest. The inferior pedicle running posteriorly to the rectus abdominis muscle is clearly visible
Rectus abdominis muscles can be vascularized by three different patterns:
1.
Type I: single superior and inferior arterial supply (29 %).
2.
Type II: double-branched system from each source artery (57 %)
3.
Type III: triple-branched system from each vessel (14 %).
Symmetrical vascular pattern symmetry was described in only 2 % of patients.
Miller et al. [12] found that only 40–50 % of patients have macroscopic communication between the two systems, whereas 60 % of patients have choke vessels of microscopic caliber. The superior vessels pass into the muscle from the deep aspect of the costal margin and run inferiorly. The distal supply enters the posterolateral aspect of the muscle below the arcuate line and passes up to anastomose with the superior vessels in the periumbilical area. Major vascular supply is provided by the deep inferior vessel with venous drainage system supported by two large venae comitantes into the iliac vein. The inferior and the superior venous systems create an anastomotic web at the umbilical level. When a pedicled TRAM flap is raised, distal venous flow has to reverse and follow the drainage pattern of the superior veins, overcoming the venous valves within the choke system described by Moon and Taylor [11]. Arterial perforators arise in two rows aside the linea alba. The lateral row lies 2–3 cm within the lateral border of the rectus sheath, whereas the medial row lies 1–2 cm from the linea alba. These vessels differ significantly in both size and number; their caliber may vary up to several millimeters in diameter.
The anterior rectus sheath is tightly adherent to the muscle at the tendinous inscriptions. It is formed by two layers provided by external and internal oblique muscles in the lower rectus abdominis muscle and by a single layer in the upper rectus abdominis muscle. During flap elevation, it is possible to harvest a gentle strip of fascia within the muscle in order to keep it more resistant to tractions or to spare as much fascia as possible in order to provide a stabler closure of the door site [13]. A muscle-sparing technique can be used to leave a strips of muscle laterally and medially to assist in maintaining abdominal-wall strength, but it has been demonstrated that any muscular segment left loses neurovascular inputs [14, 15]. For these reasons nowadays the muscle-sparing pedicle TRAM flap can be considered obsolete. Two major vascular classifications exist for TRAM flap blood supply. The most classical description was introduced by Hartrampf (Fig. 28.2), who divided the supply into four zones:
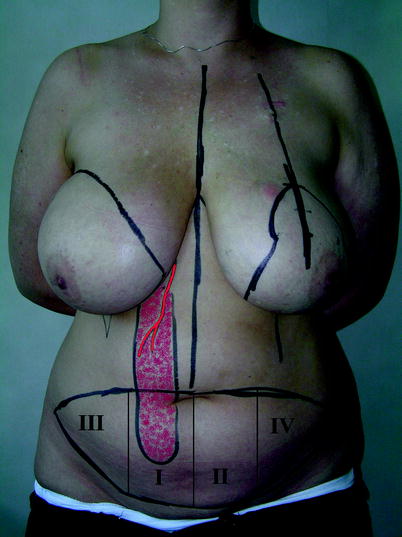
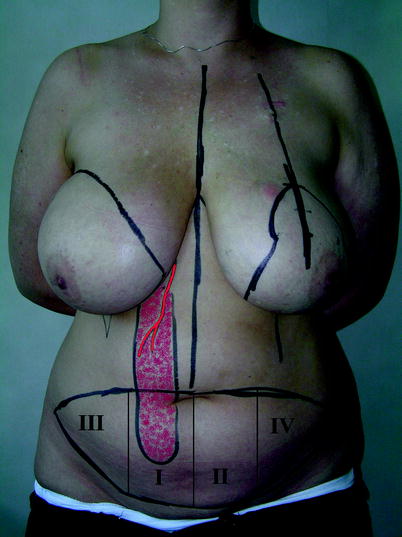
Fig. 28.2
TRAM flap vascular zone classification of Hartrampf
1.
Zone I: overlying the muscle pedicle
2.
Zone II: lying across the midline, immediately adjacent to zone I
3.
Zone III: lying lateral to zone I on the ipsilateral side
4.
Zone IV: lying lateral to zone II on the contralateral side from the pedicle.
Zone I has been found to be the most reliable portion of the flap. The medial portion of zone III is the next most reliable portion of the flap, but its blood supply decreases close to the ipsilateral tip. The medial portion of zone II is also usually reliable, but the lateral part is less predictable. Finally, zone IV should always be considered as not vascularized and should be discarded routinely. Holm et al. [16] demonstrated that although zone I remains the most reliably perfused portion of the flap, any flow across the midline is more precarious than ipsilateral flow. So the classification of Holm et al. proposes that Hartrampf’s zone III should be renamed zone II, and Hartrampf’s zone II should be renamed zone III (Fig. 28.3).
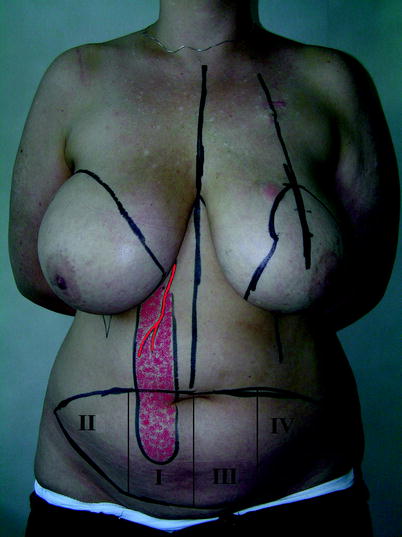
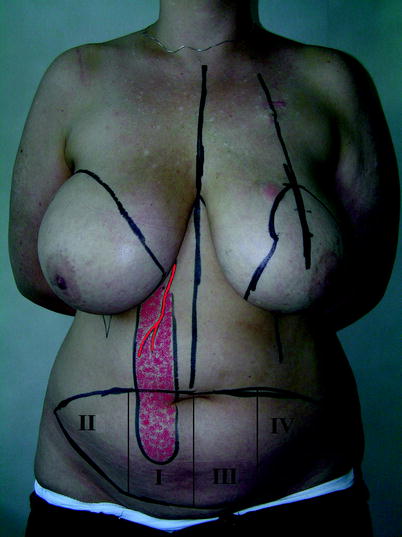
Fig. 28.3
TRAM flap vascular zone classification of Holm et al
Moon and Taylor [11] recommend surgical delay of the TRAM flap until 1 week before definitive elevation. The procedure focuses on ligation of the superficial and deep inferior epigastric systems in an outpatient setting. It increases arterial supply, but TRAM flap partial necrosis is often related to venous congestion rather than arterial inadequacy. A bigger flap can be raised with a bipedicled approach or as a free flap.
28.4 Surgical Technique
Appropriate patient selection is the key to achieving predictable results. Candidates for TRAM flap breast reconstruction must have sufficient lower abdominal tissue to achieve a successful reconstruction. Clinically, this can be evaluated by estimating the amount of superficial fat in the lower abdomen by squeezing the tissue between one’s index finger and thumb (i.e., the “pinch test”). Patients with prior abdominal surgery should be carefully selected before undergoing TRAM flap reconstruction. A Pfannenstiel or McBurney incision is considered safe. The surgical technique for flap harvesting can be similar in immediate or delayed reconstruction. Preoperative markings consist in midline drawing (very effective in donor site closure to achieve a good symmetry and result) and cutaneous palette drawing. This is achieved by marking a suprapubic transverse straight or arcuate line from one inguinal fold to the other. Laterally, it continues upward in the inguinal fold or parallel to it up to the superior transverse mark. This line is drawn 1 or 2 cm above the navel and laterally it create an angle with the anterior superior iliac spine. Markings are variable in function of the amount of skin and fat available in the lower abdomen. Also inframammary folds are marked. Preoperative Doppler imaging is useful in order to find perforators but it is not mandatory. Recipient site markings are different in the case of immediate or delayed reconstruction. In immediate breast reconstruction, the breast undergoing mastectomy is marked with oncological patterns such as for Patey mastectomy, skin-sparing mastectomy, or nipple-sparing mastectomy.
In the case of delayed breast reconstruction, it is suggested to mark inframammary fold in the contralateral breast and to recreate the opposite one with the same footprint but 2 cm above: it will be lowered during the donor site closure by donor site suture tension. Skin between this marking and mastectomy scar should be removed in order to recreate a natural new inframammary fold but surrounding skin should be excised if there is radiodystropy. A tight mastectomy scar can also be cut in a Z-style incision to release skin tension is needed.
Perioperative assessment consists of heparin prophylaxis associated with pneumatic leg pumps. Blood transfusions can be required but should be prevented. The patient is positioned on a folding surgical bed.
Surgery starts by undermining the epigastric flap in a suprafascial plane. Skin is incised to the sheath with an upward 45° inclination in order to include as many perforators as possible and also in order to face the donor site skin flap with similar thickness (Fig. 28.4).


Fig. 28.4
Elevating the epigastric skin flap. A 45° initial incision can produce several improvements, such as better skin vascularization and better donor site closure with a nice aesthetic result
Rectus abdominis muscles are both individuated up to the rib arc and xiphoid. Rectus abdominis muscles and external oblique muscles are dissected on a suprafascial plane keeping a very thin layer of fat on the fascia in order to respect suprafascial vascularization as much as possible (Fig. 28.5).


Fig. 28.5
Epigastric skin flap is elevated: the rectus abdominis muscles are both individuated up to the rib arc
Then, a tunnel is undermined to the breast. The tunnel should be large enough to let the surgeon’s fist pass (Fig. 28.6). Before the flap dissection is continued, it is helpful to tilt the patient in order to check donor site closure (Fig. 28.7). In case of excessive skin tension, it is possible to modify the preoperative lower markings.



Fig. 28.6
A tunnel is undermined to transpose the flap to the chest. It should be large enough but it is suggested that dissection should not exceed the midline in order to respect the inframammary fold

Fig. 28.7
Checking donor site closure. The patient can be moved to a slightly sitting position but skin tension should be avoided
Flap dissection continues with suprafascial dissection of the TRAM flap skin island from lateral to medial, identifying perforators (Fig. 28.8). The choice of an ipsilateral or a contralateral pedicle is based on the availability of good perforators. If possible, it is suggested to harvest an ipsilateral pedicle because it has been described as having better perfusion [17] and also a better arch of rotation. Also an ipsilateral pedicle avoids having a muscle bulge in the xiphoid after flap rotation.


Fig. 28.8
Lateral view of the skin island after dissection. Perforators are usually identified in a row
Once it has been decided which side is to be dissected, the rectus sheath is incised all along its length medially to the lateral border and a few millimeters laterally to the perforators. The fascia is also incised 1 cm laterally to the medial border of the muscle down to the skin palette (Fig. 28.9).


Fig. 28.9
Fascial dissection exposes rectus abdominis muscle
Muscle is dissected from the fascia and intercostal segmental vessels and nerves are ligated (Fig. 28.10). Main vessels run just beneath muscle so it is suggested that the posterior fascia should be dissected by fat surrounding main vessels.










