Microvascular reconstruction of nasal defects is a complex procedure and must consider 3 nasal components: skin, osteocartilaginous framework, and intranasal lining. These layers can be reconstructed with various flaps and grafts. The commonly used flaps are the first dorsal metacarpal flap, dorsalis pedis flap, auricular helical rim flap, and radial forearm and prelaminated flaps. These flaps can be composed of skin and cartilage or skin and bone. The decision is based on the patient’s needs taking into consideration the extent of the defect and presence or absence of nasal septum and columella.
The nose is perhaps the most complex structure in the face, and its 3-dimensional structure and function makes it one of the most challenging areas for reconstruction. A common saying in surgery is that availability of multiple options usually means that none of them work well in every situation. This is true in nasal reconstruction. The surgeon must consider many variables when planning for reconstruction and decide on the approach based on the individual patient.
The enthusiasm for microvascular reconstruction must be neutralized by the fact that local flaps provide excellent color and texture match without the technical difficulties and morbidity of free tissue transfer. Matching those qualities from the available donor sites of free flap are less than optimal for nasal resurfacing, which is why the forehead flap is usually considered the primary option for reconstruction of the nasal skin. On the other hand, there are instances in which microvascular reconstruction becomes an attractive option or even necessary. The use of free flaps for nasal reconstruction is usually limited to total nasal defects, defined as bilateral through-and-through loss of nasal skin, cartilage, bone, and lining mucosa, defects with a lack of lining options, and defects that involve the upper lip or the cheek because of the limitation of recruitment of local tissues without distorting the facial units. Moreover, previous exposure to or the anticipation for postoperative radiotherapy can make the local tissues a more fragile form of reconstruction.
Reconstruction of total nasal defects must consider separately each of the 3 nasal components: skin, osteocartilaginous framework, and mucosal lining. The external envelope can be reconstructed with a variety of flaps and grafts, including free flaps. A few options include osteocutaneous or chondrocutaneous free flaps such as dorsalis pedis, radial forearm (prelaminated or not), and auricular helical rim that could potentially reconstruct the skin (or the nasal lining) and the framework simultaneously. However, the reconstruction of the nasal lining is the most difficult and possibly the most important. The likelihood of scarring and contracture need to be taken into consideration when choosing the lining reconstruction method because it can collapse the nose, obstruct the airway, and compromise the result of the entire effort. Options include mucosal grafts or flaps and skin grafts or flaps. Mucosal grafts usually provide good results, but in several situations their availability is limited, as in the case of loss of the nasal septum. Skin grafts are usually subject to contracture that leads to stenosis and nasal obstruction, dryness, and crusting. Free flaps have been used with success in nasal lining reconstruction, with radial forearm, lateral arm, dorsalis pedis, and first dorsal metacarpal being the most used flaps.
Different types of free flaps have been used for nasal reconstruction, each one with its own advantages and disadvantages. However, these flaps share a few common features. Generally, they are thin and are also covered by thin skin, which helps to create the contour around the nasal framework or provide adequate lining without obstructing the nasal airway. The flap should incorporate bone or cartilage for structural reconstruction or at least provide a well-vascularized bed for the bone and cartilage grafts, allowing them to survive and minimizing their resorption. The free flaps have a long pedicle because the vessels used for anastomosis are usually from the facial artery and vein, considering their location and caliber. In a few reports, surgeons have used vessels from previous free flaps for anastomosis or other vessels in the face, such as the angular artery.
Microvascular reconstruction of nasal defects is nearly always a staged procedure. The first step is to create a lining and support, the foundation for creating a patent nasal airway. The second stage usually involves refining the structural support and thinning of the flap. A third stage is usually done to refine the nasal contour.
Types of free flaps for nasal reconstruction
First Dorsal Metacarpal Flap
The first dorsal metacarpal free flap gets its name from the name of its arterial supply, the first dorsal metacarpal artery. This vessel comes from the radial artery, usually at the level of the snuffbox, and has a consistent anatomic course along the first interosseous muscle, supplying the skin over the first dorsal web space and the radial aspect of the dorsum of the index finger. The donor site skin paddle is small, which restricts its use ( Fig. 1 ). The donor site can usually be closed with a skin graft. Even though this prevents minimal functional impairment, it is highly visible.
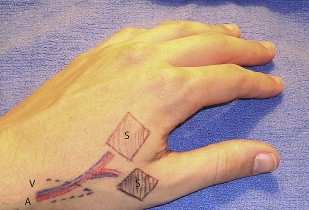
Despite its consistency, this flap has not been used frequently for facial reconstruction. It was reported to be used for eyelid and nose reconstruction. The major advantages of this flap are its thin skin and the possibility of a double skin island. One of its shortcomings, besides the skin paddle size, is the vessel caliber. Often, the size is about 1 mm, making the microvascular anastomosis technically challenging, and at times is less than 0.5 mm, making these flaps too small for microvascular transfer.
Dorsalis Pedis Flap
The dorsalis pedis flap was initially described by McGraw and Furlow. These flaps provide one of the thinnest skin sources, with minimal bulk and fat, and offer the possibility of incorporating the metatarsal bone, creating an osteocutaneous free flap. The flap is based on the dorsalis pedis artery, which can provide a long pedicle that helps when used in head and neck reconstructions. The amount of tissue is variable, depending on the cutaneous distribution of the artery. This flap was described as proximal or distal, depending on where the skin island is harvested in relation to the ankle ( Fig. 2 ).
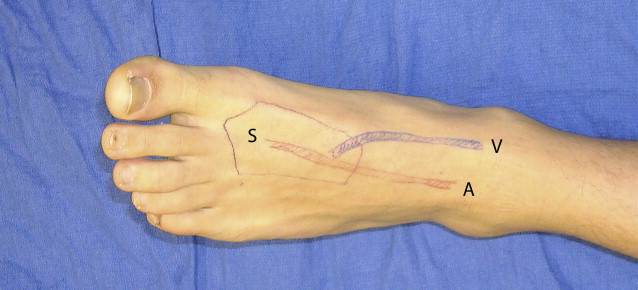
Even though most reports describe an overall successful result, the donor site still carries the chance of significant morbidity. One of the major drawbacks of this flap is the questionable presence of collateral circulation to the foot. This situation becomes even more important when considering the elderly population, who are prone to atherosclerotic disease.
Auricular Helical Flap
The ascending portion of the helix of the ear has a peculiar structure that resembles the nasal alae: thin skin anterior and posterior surrounding a layer of thin cartilage. The first description of a free flap from the auricle to the nose used an accessory auricle, a cartilage fragment covered by skin right anterior to the tragus. Shortly after, a formal description of a free flap from this region, pedicled on the superficial temporal vessels, was made to reconstruct the nose. The pinna has a rich vascular network with extensive collateral circulation supplied from the superficial temporal and the postauricular arteries, and some investigators argue that most portions of the ear could survive as a flap based on either vessel.
The center of the flap is the ascending helical rim, but it can be extended superiorly or inferiorly ( Fig. 3 ). Superiorly, advancing to the horizontal portion of the helix, the flap can be used to reconstruct the alae along with the columella. Inferiorly, to include the crus of the helix, the flap can be used to reconstruct the nostril sill. This flap has excellent color match and gives the reconstructed nose a similar contour. The dimensions of the flap can be customized depending on the extent of the defect; however, this flap carries the limitation of reconstruction of only a unilateral defect. This limitation is because of the resulting deformity of the donor ear. Often, the donor site can be closed primarily with rotation and advancement of the helical rim, which produces a smaller but acceptable ear. However, if the flap is very extensive, to reconstruct bilateral nasal alae defects, the donor ear may become unacceptably deformed. Microvascular reconstruction of the nasal alae means a substantial effort to reconstruct a small defect. Nonetheless, the reconstruction provides a well-vascularized tissue with a predictable result for the patient, unlike the composite grafts from the ear, and does not have variable survival or significant atrophy.

Radial Forearm Flap
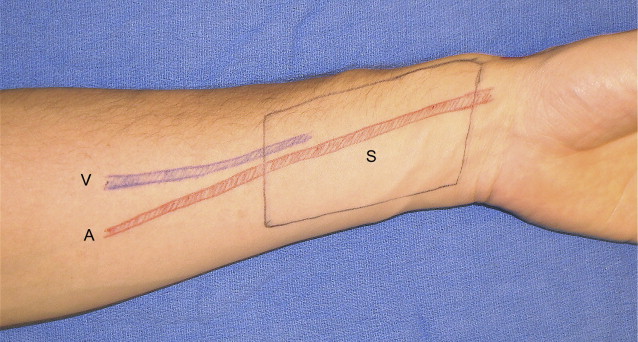
The radial forearm free flap was described in 1982 and since then became the workhorse in head and neck reconstruction. The flap is based on the radial artery. It is contraindicated in patients who do not have a palmar arch, which happens in about 15% of the population and is assessed by the Allen test, which evaluates palmar recirculation when the radial artery is occluded by manual pressure. In this scenario, the ulnar artery flap can allow for harvest of nearly the same skin. The radial forearm flap provides thin and hairless skin similar to the dorsalis pedis flap ( Fig. 4 ). However, the vessels in the forearm are not usually involved by atherosclerotic changes, and the donor site morbidity, functionally and cosmetically, in the upper extremity is much lower, with only the need of a skin graft to replace the forearm skin and a forearm splint to facilitate the skin graft success. The forearm flap is usually further thinned by a process called lipopluction, whereby the capsule of each lobule is punctured with a needle and the contents gently suctioned.