23 Microdermabrasion
Microdermabrasion (MDA) is a superficial skin resurfacing procedure that utilizes gentle mechanical abrasion to remove the outermost layers of the epidermis.1 Removal of outer skin layers, also called exfoliation, has been used for skin rejuvenation since 1500 BC, when the ancient Egyptians used sandpaper and sour milk baths containing lactic acid. Microdermabrasion uses refined abrasive elements, such as diamond-tipped pads or a constant flow of crystals swept across the skin, to remove the stratum corneum.2 Due to popular marketing, patients are aware of MDA and it is often considered as an initial treatment for aesthetic rejuvenation. It is one of the most commonly performed aesthetic procedures in the United States today, with more than half a million MDA treatments performed annually, according to data from the American Society for Aesthetic Plastic Surgery,3 and it is one of the most common aesthetic procedures incorporated into office practice.4,5
Skin rejuvenation with microdermabrasion is based on the principles of wound healing. By wounding and removing superficial skin layers in a controlled manner, cell renewal is stimulated with regeneration of a healthier epidermis and dermis.1 After a series of MDA treatments, histologic changes in the skin are evident. These changes include a compacted stratum corneum and smoother epidermis, increased dermal thickness with fibroblast production of new collagen and elastin,6 and increased skin hydration with improved epidermal barrier function.7,8 Clinical improvements can be seen in hyperpigmentation9 and rough skin texture.10 Some studies also show improvements in fine lines, pore size, superficial acne scars, and acne vulgaris.7,9,11 MDA can be readily combined with other minimally invasive aesthetic procedures, such as chemical peels and nonablative laser treatments, many of which can be performed in the same visit, to enhance skin rejuvenation results.12
Patient Selection
While almost any patient will benefit from exfoliation with MDA, patients with mild to moderate photoaging changes of solar lentigines, rough texture, and fine lines (e.g., Glogau types I and II) typically derive the most noticeable benefits (see Chapter 19, Aesthetics Principles and Consultation, for a description of Glogau types). Results with MDA are slow and progressive, requiring a series of treatments for visible improvements. Assessment of patients’ expectations at the time of consultation and commitment to a series of treatments is essential to the success of these treatments.
Patients of all Fitzpatrick skin types may be treated with MDA (see Chapter 19 for a description of Fitzpatrick skin types). It is advisable to treat darker skin types (IV through VI) conservatively because they have increased risks of pigmentary changes such as postinflammatory hyperpigmentation. Elderly patients with thin and friable skin and patients with erythematous conditions such as rosacea, telangiectasias, and poikiloderma of Civatte are also treated conservatively, because they have greater risks of abrasion and worsening of erythema respectively.
Cosmetic Indications1
Microdermabrasion Devices Currently Available
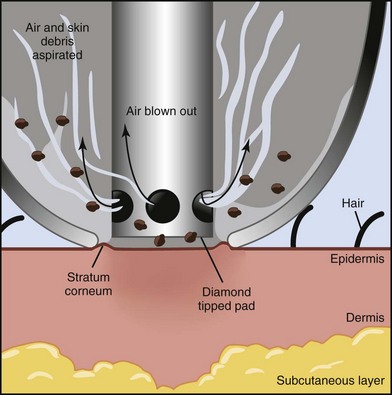
Most MDA devices utilize a closed-loop vacuum system, which draws the skin up to an abrasive element on the handpiece tip. The handpiece is passed across the skin and cellular debris is removed and suctioned up into a collection container and disposed of after treatment. The process of MDA exfoliation using a diamond-tipped device is shown in Figure 23-1. Abrasive elements used by MDA devices vary and the most commonly used elements are:
Crystal-free MDA devices have become popular because they lack these ocular and inhalation risks. Common crystal-free abrasive elements include diamond-tipped pads and bristles. Figure 23-2 shows a MDA handpiece with diamond-tipped treatment heads of various coarseness. Most of these devices have reusable treatment heads that can be sterilized following treatment. Some crystal-free devices combine simultaneous application of topical solutions during exfoliation, called infusion. The intent is to deliver topical products more effectively to the skin by taking advantage of the transient disruption of the epidermal barrier. Selection of topical solutions is based on the presenting condition. For example, hydroquinone or cosmeceuticals such as kojic acid and decapeptide-12 may be used for patients with hyperpigmentation; erythromycin and salicylic acid for acne and rosacea; and hyaluronic acid and glycerin for dehydrated skin.
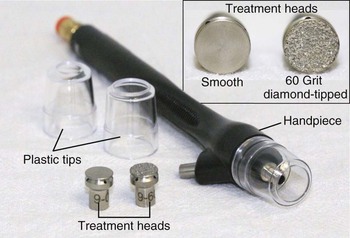
FIGURE 23-2 Microdermabrasion handpiece and diamond-tipped treatment heads.
(SilkPeel Envy, copyright Rebecca Small, MD.)
MDA devices are classified by the FDA as type I devices, which do not require the manufacturer to establish performance standards or perform clinical trials to demonstrate efficacy. With more than 30 MDA devices available, this presents a challenge to providers when selecting a device. Most MDA machines are either manufactured for estheticians (“esthetician grade”) or for clinical providers (“medical grade”), with the latter capable of deeper exfoliation with higher vacuum pressures and more abrasive treatment heads. Commonly used MDA devices are listed in the Resources section at the end of the chapter.
Contraindications1
Advantages of Microdermabrasion
Anatomy
Histologic evaluation of skin immediately after treatment with MDA demonstrates smoothing of the stratum corneum.13 Each pass of an aluminum oxide crystal MDA handpiece removes approximately 10 to 15 µm of skin, two passes fully remove the stratum corneum, and four passes penetrate to the stratum granulosum layer of the epidermis.14 The epidermal barrier function is transiently disrupted for 2 to 3 days after treatment with increased transepidermal water loss. These effects, however, are reversed 1 week after treatment, and a more compacted stratum corneum is regenerated with improved barrier function and increased skin hydration compared to pretreatment skin.15,16
In addition to short-term improvements in epidermal barrier function, longer term improvements have also been demonstrated in the epidermis and dermis following repeated MDA treatments. Epidermal thickness increases by up to 40% due to increased cellularity,7 and dermal collagen and elastin deposition increase, which can be seen clinically as a reduction of coarse pores and fine lines.6