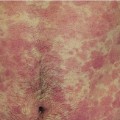
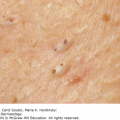
26 An accurate diagnosis, based on a proper history and examination (see Chapter 3), must come before a rational line of treatment can be chosen, and even when a firm diagnosis has been reached, each patient must be treated as an individual. For some, no treatment may even be the best treatment, especially when the disorder is cosmetic or if the treatment would be worse than the condition itself. A patient with minimal vitiligo, for example, may be helped more by careful explanation, reassurance and camouflage than by an extended course of enthusiastic treatment producing only marginal improvement. If a diagnosis cannot be reached, the doctor has to decide whether a specialist opinion is needed, or whether it is best to observe the rash, perhaps treating it for a while with a bland application. In either case, the indiscriminate use of topical corticosteroids or other medications, in the absence of a working diagnosis, often confuses the picture and may render the future diagnosis more difficult. However, provided the steps described in Chapter 3 are followed, a firm diagnosis can usually be made, and a sensible course of treatment can be planned but even then the results are often better when patients understand their disease and the reasons behind their treatment. The cause and nature of their disease should be explained to patients carefully, in language they are familiar with, and they must be told what can realistically be expected of their treatment. False optimism or undue pessimism, by patients or doctors, leads only to an unsound relationship. Too often patients become discontented, not because they do not know the correct diagnosis but because they have not been told enough about its cause or prognosis. Even worse, they may have little idea of how to use their treatment and what to expect of it; poor compliance often follows poor instruction. If the treatment is complex, instruction sheets are helpful; they reinforce the spoken word and answer unasked questions. A useful source of regularly updated information sheets on different dermatological conditions and their treatment is provided by the British Association of Dermatologists (http://www.bad.org.uk/site/792/default.aspx). The principal steps in diagnosis and management: Some of the treatments used in dermatology are listed in Table 26.1. Table 26.1 Therapeutic options in dermatology. The great advantage of topical therapy is that the drugs are delivered straight to where they are needed, at an optimum concentration for the target organ. Systemic side effects from absorption are less than those expected from the same drug given systemically. With topical treatment, vital organs such as the marrow, liver and kidneys are exposed to lower drug concentrations than is the skin. However, topical treatment is often messy, time-consuming and incomplete, whereas systemic treatment is clean and quick and its effect is uniform over the entire skin surface. Cost must also be considered. Some drugs can only be used topically (e.g. permethrin for scabies and mupirocin for bacterial infections), while others only work systemically (e.g. azathioprine for pemphigus and methotrexate for psoriasis). When a choice exists, and both possibilities are equally effective, then local treatment is usually to be preferred. Most cases of mild pityriasis versicolor, for example, respond to topical antifungals alone so systemic itraconazole is not the treatment of first choice. A drug (the active ingredient) used on the skin must be dissolved or suspended in a vehicle (base). The choice of the drug and of the vehicle are both important and depend on the diagnosis and the state of the skin. For a drug to be effective topically, it must pass the barrier to diffusion presented by the horny layer (see Chapter 2). This requires the drug to be transferred from its vehicle to the horny layer, from which it will diffuse through the epidermis into the papillary dermis. Passage through the horny layer is the rate-limiting step. The transfer of a drug from its vehicle to the horny layer depends on its relative solubility in each (measured as the partition coefficient). Movement across the horny layer depends both upon the concentration gradient and on restricting forces (its diffusion constant). In general, non-polar substances penetrate more rapidly than polar ones. Low molecular weight drugs penetrate the epidermis better than high molecular weight ones. A rise in skin temperature and in hydration, both achieved by covering a treated area with polyethylene occlusion, encourages penetration. Some areas of skin present less of a barrier than do others. Two extreme examples are palmar skin, with its impermeable thick horny layer, and scrotal skin, which is thin and highly permeable. The skin of the face is more permeable than the skin of the body. Body fold skin is more permeable than nearby unoccluded skin. In humans, absorption through the hair follicles and sweat ducts is of little significance and the amount of hair on the treated site is no guide to its permeability. In many skin diseases, the horny layer becomes abnormal and loses some of its barrier function. For example, the abnormal nucleated (parakeratotic) horny layers of psoriasis and chronic eczema, although thicker than normal, have lost much of their protective qualities. Water loss is increased and therapeutic agents penetrate more readily. Similarly, breakdown of the horny layer by chemicals (e.g. soaps and detergents) and by physical injury will allow drugs to penetrate more easily. Conversely, as the skin heals,the barrier function of the horny layer returns and drug absorption diminishes. In summary, the penetration of a drug through the skin depends on the following factors: These include corticosteroids, tar, dithranol, antibiotics, antifungal and antiviral agents, benzoyl peroxide, retinoic acid and many others (Formulary 1). The choice depends on the action required, and prescribers should know how each works. Topical corticosteroids are the mainstay of much local dermatological therapy and their pharmacology is summarized in Table 26.2 (Figures 26.1 and 26.2). Table 26.2 The pharmacology of topical corticosteroid applications.
Medical Treatment
Therapeutic options
Drugs
Topical
Systemic
Physical
Surgical
excision
curettage
Intralesional injection
Electrodessication
Cryotherapy
Radiotherapy
Phototherapy
Laser therapy
Topical and systemic therapy
Topical treatment
Percutaneous absorption
Active ingredients
Active
Include hydrocortisone and synthetic halogenated derivatives
constituents
Halogenation increases activity
Bases
Available as solutions, lotions, creams, ointments, sprays, mousses foams, masks and tapes
Penetration
Readily penetrate via the horny layer and appendages
Form a reservoir in the horny layer
Polyethylene occlusion and high concentrations increase penetration
Metabolism
Some minor metabolism in epidermis and dermis (e.g. hydrocortisone converts to cortisone and other metabolites) ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access