Mastopexy: Periareolar, Vertical, and Wise Pattern
Ryan P. Ter Louw
Scott Spear†
†Deceased
DEFINITIONS
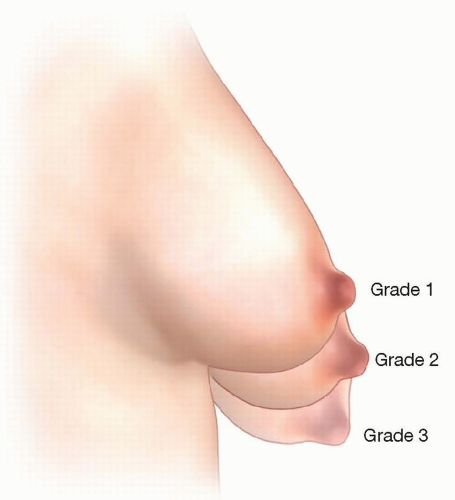
Ptosis of the breast is described by the Regnault classification (FIG 1).
Grade 1: minor ptosis; the nipple is at the level of the inframammary fold, above the lower contour of the gland.
Grade 2: moderate ptosis; the nipple is below the level of the inframammary fold, above the lower contour of the gland.
Grade 3: major ptosis; the nipple is below the level of the inframammary fold, at the lower contour of the gland.
Mastopexy—masto meaning breast, pexy meaning to lift or fixate.
Periareolar mastopexy results in a scar camouflaged in the junction of the pigmented areolar and unpigmented breast skin.
Concentric mastopexy, eccentric, “donut” mastopexy
Vertical or circumvertical mastopexy results in a scar camouflaged in the junction of the pigmented areolar and unpigmented breast skin with a vertical extension along the breast meridian down toward the inframammary fold.
There may be a transverse scar as well if there is too much skin to be tailored in the circumareolar and vertical components.
Wise pattern mastopexy is planned from the outset to result in a scar around the areola, a vertical extension along the breast meridian down to the inframammary fold, with a horizontal scar hidden in the inframammary fold.
ANATOMY
The arterial supply of the breast is predominantly based off internal mammary perforators and the lateral thoracic artery.
Sensation to the nipple is derived from the 4th posterior intercostal nerve.
Cooper ligaments suspend the breast, originating on the pectoralis fascia and inserting into the dermis of the breast.
The borders of the breast:
Superior—clavicle
Inferior—inframammary fold
Lateral—latissimus muscle
Medial—sternum
PATHOGENESIS
Decreased elasticity of breast tissue with aging
Hormone-induced inflation and deflation of breast tissue
Stretch of Cooper ligaments
Deflation of breast envelope following breast feeding
PATIENT HISTORY AND PHYSICAL FINDINGS
History
Current cup size, height, and weight
Childbearing, breast-feeding, and future family planning
Personal and familial cancer history
Prior breast surgery, biopsies, radiation
Date of last mammogram
Examination1
Regnault classification of ptosis
Soft tissue evaluation: skin laxity, density of glandular tissue
Soft tissue masses, axillary lymphadenopathy, nipple discharge
Critical measurements
Nipple to sternal notch
Nipple to inframammary fold
Breast width
Nipple to midline
Areolar diameter
Patient weight, height, and bra size
Symmetry of nipple position and breast size should be noted and mentioned to the patient in the initial consultation. If present before surgery, asymmetry will persist postoperatively to some degree.
Chest wall deformities as well as the presence or absence of pectoralis major and latissimus muscles should be noted.
IMAGING
A yearly screening mammogram is recommended beginning at age 40, or 10 years earlier than a primary relative’s diagnosis of breast cancer.
DIFFERENTIAL DIAGNOSIS
Tuberous breast deformity
Pseudoptosis
SURGICAL MANAGEMENT
Preoperative planning in the mastopexy patient is critical for obtaining an aesthetic result.
Mastopexies have been the source of a disproportionate amount of litigation, so the surgeon should not take these operations lightly. Understanding the indications and limitations for each type of mastopexy will aid in avoiding trouble.
Periareolar mastopexy is most useful in patients who need limited movement of the nipple-areolar complex.
It allows for movement of the nipple-areola complex approximately 2 cm. Attempting to move the nipple more than 2 cm will result in flattening of the breast mound.
Periareolar mastopexy is ideal for grade 0 or 1 ptosis, glandular ptosis, or in the setting of combined augmentation mastopexy (FIG 2A,B).
Vertical mastopexy is a versatile operation that allows the surgeon to resite the nipple, regardless of the degree of ptosis, while reshaping the breast mound and tailoring the skin envelope (FIG 2C-F).
Wise pattern mastopexy is typically reserved for patients with significant skin redundancy that do not want a decrease in breast volume (FIG 2G,H).
Patients with nipple to inframammary fold distance of 12 cm or greater may be good candidates for this procedure, with the trade-off of an additional horizontal scar under the breast.
In vertical mastopexies, the decision to incorporate a horizontal incision is a function of removing dog ears at the IMF. The true Wise pattern mastopexy requires marking and committing to the surgical incisions with the patient in the standing position.
The entire Wise pattern incision pattern can be de-epithelialized to maintain breast volume.
Positioning
The patient should be positioned supine on the operating room table with the hips at the flexion point of the bed to facilitate the sitting position intraoperatively.
The arms may be tucked at the patient’s side or out on arm boards but should be secured and padded adequately.
TECHNIQUES
▪ Periareolar Mastopexy
Planning and Markings
The concentric or donut mastopexy is indicated for patients with minimal or grade 1 breast ptosis.
The surgeon should not attempt to achieve an aggressive movement of the nipple-areolar complex with this technique as it may excessively flatten the contour of the breast, produce a dilated widened areola, or result in poor circumareolar scarring.
The concentric mastopexy should be applied only to patients with reasonably aesthetic nipple position within the minimally ptotic breast.
If the nipple is not within the breast meridian, eccentric or crescentic mastopexy should be considered.
The patient is marked in the anatomic standing position, with arms at the sides.
The midline, inframammary fold, and breast meridian are marked.
The overall breast symmetry and NAC are assessed.
The proposed nipple position is transposed from the IMF to the anterior breast skin.
The outer mastopexy circumference is typically marked freehand (TECH FIG 1A).
The outer markings skirt the edges of the areola medially and laterally.
The critical upper and lower limits of the typically oval outer periareolar pattern are determined superiorly by the desired new upper border location for the superior edge of the areola and inferiorly by the length of skin
desirable to leave between the lower edge of the areola and the IMF (typically 5-8 cm depending on the size of the breast)
The inner pattern is usually drawn as a round circle using a “cookie cutter” pattern of 38 to 42 mm.
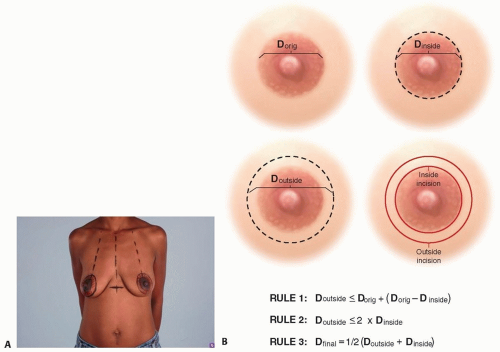
Basic guidelines for concentric mastopexy described by Spear et al.5 provide guidelines for nipple-areolar marking (TECH FIG 1B).
First and most importantly: Diameter outside − diameter original should be equal to or less than (diameter original − diameter inner), meaning it is preferable to remove more pigmented skin than unpigmented skin.
Second: Diameter outside should ideally be no more than two times the diameter inside.
Third: Diameter final = ½ (diameter outside + diameter inside).
Incisions and Closure
A 38- or 42-mm cookie cutter is used to mark the proposed nipple-areola diameter with the assistant applying mild tension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree