Management of Wrist Fractures
Sandeep Jacob Sebastin
Kevin C. Chung
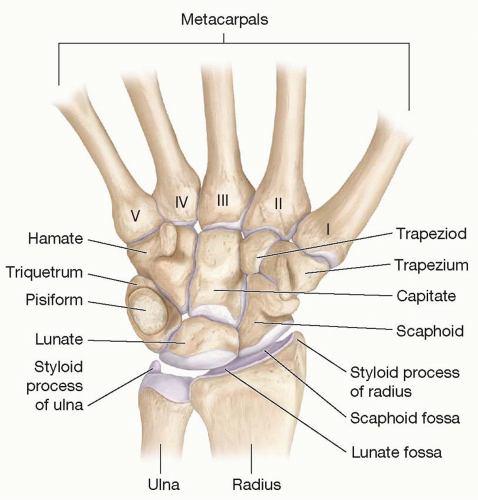
The wrist is one of the most complex joints in the body and links the forearm to the hand. Anatomically the wrist consists of eight carpal bones, but functionally it extends from the distal forearm to the base of the metacarpals and includes the distal ends of the radius and the ulna, eight carpal bones, and the bases of the metacarpals (Figure 76.1). The distal radius and ulna refer to the distal 2 to 3 cm metaphyseal (cancellous) portion of these two bones.1 The carpal bones are arranged in two rows. The proximal row includes the scaphoid, lunate, and the triquetrum and the distal row includes the trapezium, trapezoid, capitate, and the hamate. The pisiform is a sesamoid bone in the tendon of the flexor carpi ulnaris (FCU) and lies palmar to the triquetrum.2 This complex architecture of the wrist is maintained by the inherent geometry of the bones that are held together by numerous extrinsic and intrinsic ligaments (Chapter 81). This joint configuration maintains stability and allows for transfer of loads from the hand, while providing tremendous mobility. This chapter discusses the management of fractures of the wrist with emphasis on the distal radius and the scaphoid with brief mention of avascular necrosis of the lunate (Kienbock disease).
DISTAL RADIUS FRACTURES
A fracture of the distal radius and/or ulna is the most common fracture seen by physicians accounting for 15% to 20% of all fractures. There is a bimodal age distribution, with peaks of incidence occurring in the youth and in the elderly.3,4 In the younger population, these fractures are most often the result of high-energy trauma such as motor vehicle accidents or falls from a height. In the elderly population, however, these fractures frequently result from falls from a standing height and other low-energy trauma.5 Although the overall gender rates are similar, the fractures in men tend to occur in the younger group, whereas there is a preponderance of females in the elderly group due to osteoporosis. In the United States, approximately 280,000 fractures occur in working-age persons and the economic impact of these injuries is considerable, as patients take an average of 12-16 weeks to return to work. Approximately 10% of 65-year-old white women will experience a distal radius fracture in their lifetime and the annual incidence of distal radius fractures in the US population over the age of 65 has been reported to be 57-100 per 100,000. These numbers will rise in the future because the “Baby Boomers” are aging and individuals are living longer and lead healthier and more active lives compared to previous generations.6
Anatomy
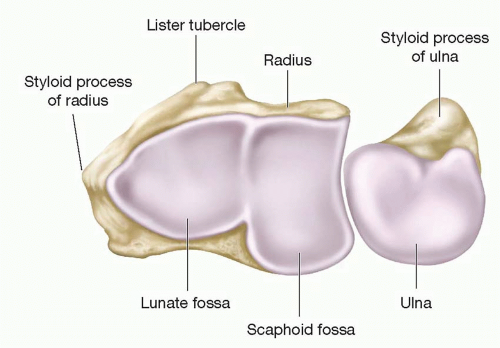
The ulna articulates proximally with the humerus and represents the stable unit of the forearm. The radius (with the associated carpus and hand) rotates around the ulna at the proximal and distal radioulnar articulations.3 The volar surface of the distal radius is relatively flat, whereas the dorsal surface is convex and closely related to the overlying extensor tendons. The volar cortex of the distal radius is also considerably thicker than the dorsal cortex. The distal ends of the radius and ulna articulate with the proximal carpal row. The distal end of the radius has three articular fossae (Figure 76.2). The most radial is the triangular scaphoid fossa with the radial styloid at its apex. An anteroposterior ridge (interfacet ridge) separates the scaphoid fossa from the lunate fossa. The sigmoid fossa is located along the distal ulnar surface of the radius and articulates with the ulnar head.7 It has a poorly defined proximal margin, but well-defined distal, volar, and dorsal margins.8 The carpus is separated from the distal end of the ulna by the triangular fibrocartilage complex (TFCC). The TFCC originates on the ulnar border of the lunate fossa and inserts onto the base of the ulnar styloid.9
Biomechanics
Approximately 80% of the axial load across the wrist is transmitted through the distal end of the radius and 20% across the TFCC and the distal end of the ulna.3 Most fractures of the radius occur at the metaphysis because it is mostly spongy cancellous bone. Fractures may be either extra-articular or intra-articular involving the radiocarpal and/or distal radioulnar joint/s (DRUJ). Extra-articular fractures often follow a fall on an outstretched, extended hand. Because the dorsal cortex is thinner compared to the volar cortex, it is frequently comminuted and results in the classic dinner fork deformity (dorsal displacement with dorsal tilt [loss of normal volar tilt], radial tilt [loss of radial inclination], and shortening [loss of height]).10 Intra-articular fractures usually result from higher energy trauma and the fracture pattern depends on the magnitude and direction of force and the quality of bone and soft tissues. The lunate can exert pressure on its fossa causing a die-punch fracture. A multifragmentary intra-articular fracture pattern with four large fracture fragments is often seen. These fragments are the radial styloid, the radial shaft, and volar and dorsal lunate fossa fragments.1 Occasionally the articular surface is sheared off to produce a fracture subluxation of the wrist. Other deforming forces around the distal radius include the insertion of the brachioradialis on the radial styloid, associated injuries to the ulnar styloid or the TFCC that can lead to DRUJ instability, and intercarpal injuries that can lead to carpal instability.11
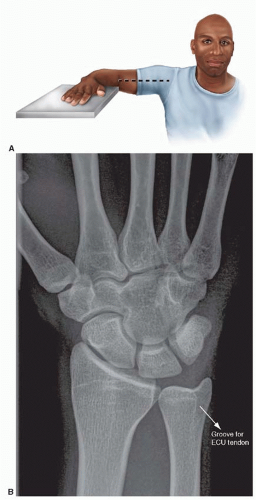 FIGURE 76.3. Standard PA radiograph of wrist. A. Positioning for a wrist PA radiograph. B. A correctly positioned PA view showing the ECU groove radial to the ulnar styloid. |
History and Physical Examination
The key elements in the history are the mechanism of injury to determine the energy involved and the direction of force transmission. This information is useful in assessing severity of injury and likelihood of associated ligament and nerve injuries.7 The patient should be questioned about pain in the hand, elbow, and shoulder and sensation in the median nerve distribution. The patient should also be questioned about handedness, occupation, medical history, social history, and recreational activities to determine the functional demands on the injured wrist.2,3
The involved wrist as well as the elbow and the contralateral upper limb are examined. Focal tenderness in the anatomic snuffbox suggests a scaphoid fracture. Tenderness 1 cm distal to the Lister tubercle suggests a scapholunate ligament injury. Median nerve function is evaluated by assessing sensibility at the fingertips. We use the ‘ten test’ to perform a quick assessment.12 A decrease in sensibility compared with the normal side may indicate the need for median nerve decompression.
Radiographic Evaluation
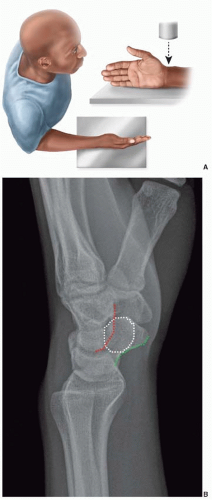
The posteroanterior (PA) and lateral radiographs are routine. The PA view is obtained with the shoulder in 90° abduction, the elbow in 90° flexion, and the wrist and forearm in neutral rotation (Figure 76.3A).13 In a true standard PA view, the groove for the tendon of the extensor carpi ulnaris should be at the level or radial to the base of the ulnar styloid (Figure 76.3B).9 The lateral view is obtained with the shoulder in 90° adduction, elbow in 90° flexion, and the hand positioned in the same plane as the humerus (Figure 76.4A). In a true lateral view, the palmar cortex of the pisiform should overlie the central third of the interval between the palmar cortices of the distal scaphoid and the head of the capitate (Figure 76.4B).
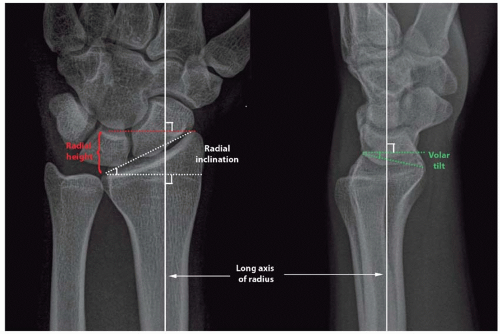 FIGURE 76.5. Measurement of radiographic parameters of the distal end of the radius [Radial height (red dotted lines), radial inclination (white dotted lines), and volar tilt (green dotted lines)]. |
Three radiographic measurements on standard PA and lateral views correlate with patient outcome: radial height, radial inclination, and volar tilt (Figure 76.5).9,11,13 The radial height is measured on a PA radiograph as the distance between a line perpendicular to the long axis of the radius passing through the distal tip of the sigmoid notch at the distal ulnar articular surface of the radius and a second perpendicular line at the tip of the radial styloid. Normal radial height averages 10 to 14 mm. The articular surface of the radius has a radial to ulnar slope (radial inclination) and a dorsal to volar slope (volar tilt).
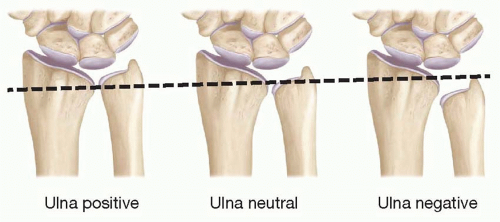
The radial inclination is also measured on a PA radiograph and represents the angle between one line connecting the tip of the radial styloid and the ulnar aspect of the distal radius and the second line perpendicular to the longitudinal axis of the radius. The normal radial inclination ranges between 20° and 25°. The volar tilt is measured on a lateral radiograph and represents the angle between the line along the distal articular surface of the radius and a line perpendicular to the longitudinal axis of the radius. The normal volar tilt averages 11° and has a range of 5° to 15°. An additional radiographic parameter that is useful is ulnar variance. Ulnar variance refers to the distance between the articular surface of the ulnar head and the ulnar border of the lunate fossa. It is described as neutral when both are at the same level: ulnar plus, when the ulna is longer; and ulnar minus, when the ulna is shorter (Figure 76.6). Normal ulnar variance can range from 0 ± 2 mm.
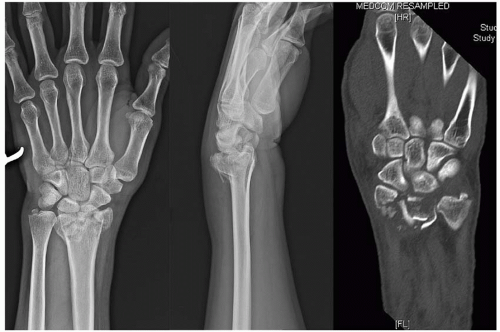
Plain radiography may be insufficient in the assessment of the comminuted, grossly displaced, and complex intra-articular fractures. Computed tomography (CT) is performed in such cases (Figure 76.7). CT should also be considered when a detailed evaluation of an articular step or gap is required. Magnetic resonance imaging (MRI) is useful when concomitant ligamentous injuries are suspected or fractures are suspected but not visualized on routine radiographs (Chapter 81). A dynamic fluoroscopic examination is also useful for detecting carpal instability.
Classification
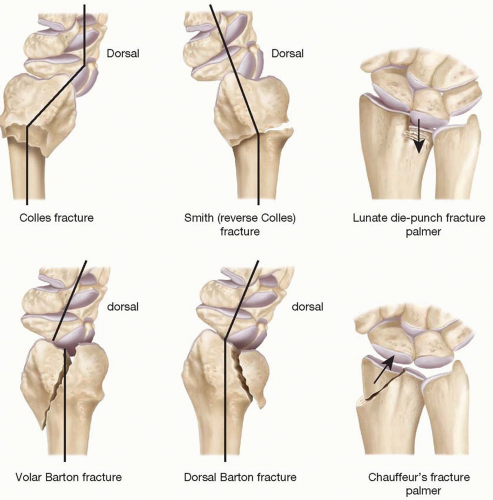
Many eponyms and classification systems have been used to describe distal radius fractures. A list of common eponyms has been provided because they are frequently used in clinical practice (Figure 76.8). The commonly used classification systems include the Frykman,14 Melone,15 Fernandez,16 Mayo Clinic,17 and the AO18 (Association for the Study of Internal Fixation) classifications. The Frykman, Melone, Mayo clinic, and the AO classifications focus on the fracture pattern, whereas the Fernandez classification is based on the mechanism of injury. We use the AO classification in our practice. It divides the fractures into three broad groups (A. Extra-articular; B. Partial involvement of articular surface; and C. Involvement of entire articular surface). These are then subdivided into 9 subtypes or 27 distinct fracture patterns (Figure 76.9).
Treatment
The aim of treatment of distal radius fractures is to restore normal anatomy (radial height, volar tilt, and articular congruity) because this is believed to correlate with functional outcome.1,13,19 Based on the radiographic findings, fractures may be classified as stable or unstable. Stable fractures do not displace at presentation or following manipulative reduction.20 They present with minimal displacement, have dorsal angulation less than 5°, and radial shortening less than 2 mm.21 Stable fractures can be managed with cast immobilization. In contrast, unstable fractures cannot be reduced or the reduction cannot be maintained. The factors that have been associated with instability following closed reduction are listed in Table 76.1.22,23 Age of the patient, dorsal comminution, and increased ulnar variance (>3 mm) are the most important predictors of collapse with cast treatment.24 Unstable distal radius fractures require surgical intervention to maintain reduction. Multiple surgical options are available that include percutaneous pin fixation, external fixation, open reduction and plate fixation, intramedullary fixation, and arthroscopically assisted fixation.
While there is no consensus, the current trend is toward internal fixation of unstable fractures.3 Insufficient data exist to support any particular treatment method. Although age is not a contraindication to surgical treatment, one must take into account the functional demands of the patient. Available evidence shows no difference between casting and surgical fixation of unstable distal radius fractures in the elderly, defined by age (>55 years), low functional demand, and poor bone quality with low-energy injuries.6
Closed Reduction and Plaster Immobilization.
This is the initial treatment for most distal radius fractures. It relies on ligamentotaxis to pull the fracture out to length, uses the intact soft tissues to reduce the displaced fragments, and requires a three-point pressure splint to maintain the reduction. Closed reduction needs relaxation of the local musculature with adequate analgesia. It can be performed under general anesthesia, axillary, or intravenous regional anesthesia, but usually it is performed under a hematoma block by infiltrating 5 to 7 mL of local anesthetic into the fracture site.
There are a number of ligaments that extend from the distal radius to the carpal bones. By putting longitudinal traction on the hand, these ligaments are stretched and pull the impacted distal radius fragments with them. In the common Colles fracture, the volar periosteum is torn, however the dorsal soft tissue (periosteum and the extensor tendon sheath) is intact. This dorsal soft tissue hinge is the key to the reduction. The traditional reduction maneuver consists of three steps: (1) Longitudinal traction for a few minutes to assist in muscle relaxation; (2) Application of a force in the direction of the deformity to disimpact the fracture fragments; and (3) Application of force opposite to the direction of deformity to reduce the fracture (Figure 76.10).25
We tend not to use the traditional maneuver to reduce Colles fractures as it requires extreme hyperextension and flexion. Instead we apply strong longitudinal traction by pulling on the thumb, index, and the long finger, while an assistant provides counter-traction at the distal arm just proximal to the elbow. Sustained traction is maintained for 5 to 7 minutes. Thereafter pressure is applied in a palmar direction on the dorsum of the distal radius (the distal fracture fragment) along with slight pronation and ulnar deviation to reduce the fracture (Figure 76.11).26,27
Once reduction is complete, it must be maintained by keeping the dorsal soft tissue hinge under tension. This is done by using a three-point pressure splint. Two points of pressure are on the dorsum of the forearm proximal and distal to the fracture site and one point is on the volar side corresponding to the fracture (Figure 76.12). Three-point pressure cannot be given by a simple dorsal splint or a volar splint. It needs a dorsoradial splint or a sugar-tong splint.28 We prefer the use of a sugar tong splint because forearm rotation can be controlled and it immobilizes the DRUJ.27 It is important to avoid extremes of wrist flexion and ulnar deviation (Cotton-Loder position) that can result in iatrogenic median nerve compression, extensor tendon tightness, and weaken flexion from decreased excursion of flexors. The splint should also not extend beyond the proximal palmar crease to allow full flexion of the metacarpophalangeal joint.
A cast is generally not applied after the initial reduction in the emergency room because subsequent swelling may lead to skin breakdown or compartment syndrome. Radiographs are repeated to evaluate restoration of the radiographic
parameters, to evaluate articular congruity, and assess severity of comminution. Patients are seen within 1 week after reduction for repeat radiography. If the reduction is maintained, the splint is exchanged for a cast. Patients are typically seen again 1 week after cast placement to ensure that fracture reduction is not lost. Surgical intervention may be needed if there is loss of reduction.9
parameters, to evaluate articular congruity, and assess severity of comminution. Patients are seen within 1 week after reduction for repeat radiography. If the reduction is maintained, the splint is exchanged for a cast. Patients are typically seen again 1 week after cast placement to ensure that fracture reduction is not lost. Surgical intervention may be needed if there is loss of reduction.9
TABLE 76.1 FACTORS ASSOCIATED WITH INSTABILITY FOLLOWING CLOSED REDUCTION OF DISTAL RADIUS FRACTURES | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree