The nasal valve is an important consideration in patients presenting with nasal obstruction. Controversy exists regarding the anatomy, terminology, evaluation, and management of the nasal valve. Innumerable techniques with variable effects have been described in the literature. The evidence qualifying these techniques has been plentiful, though often lacking in quality. This article reviews the controversial aspects of nasal valve management applying the best available evidence to help clarify potential areas of confusion. Future research using standardized definitions, consistent methodologies, and validated outcome measures are necessary to improve the quality of evidence and impact surgical decision-making.
Key points
- •
The nasal valve is frequently a contributor or sole cause of nasal obstruction and must be clinically evaluated in any patient presenting with nasal obstruction.
- •
Understanding of nasal valve anatomy with critical assessment of the site of obstruction is essential to effective nasal valve management.
- •
Validated outcome measures, such as the Nasal Obstruction Symptom Evaluation score, are helpful for preoperative evaluation of the severity of obstruction and postoperative assessment of success.
- •
Technique selection should be individualized to the locale and type of valve dysfunction. Spreader grafts are seldom adequate as a lone intervention for nasal valve dysfunction.
- •
High-quality research, ideally directly comparing techniques, is needed to both simplify and improve nasal valve management.
Introduction
The ability to breathe through the nasal passages is a noticeable feature of healthiness and well-being. The nasal airway plays a central role in air heating and humidification, olfaction, and, most importantly, airflow. Obstruction of the nasal airway is a common complaint in the otolaryngologic practice and has a dramatic impact on patient quality of life. Although several medical and surgical treatments exist to address this common patient complaint, developing the best therapeutic strategy targeting the sources of the problem can be challenging. Often, there are multiple contributing factors complicating treatment.
The causes of nasal airway obstruction are legion, though they can typically be broken down to mucosal or structural causes. Structural causes of obstruction may be posttraumatic, idiopathic, or iatrogenic at the hands of the nasal surgeon. Underpinning all of this is an anatomic malformation or dysfunction. In fact, up to 75% to 85% of people have some type of anatomic deformity of the nose. Only a subset of these individuals experience a severe enough impact on quality of life to prompt a clinical evaluation.
Most otolaryngologists are adept at diagnosing anatomical deformities of the septum and turbinates. However, nasal obstruction from nasal valve dysfunction (NVD) may be overlooked as a contributor or sole cause of nasal obstruction. NVD has been implicated in having a role in up to 13% of adults complaining of chronic nasal obstruction. Moreover, the nasal valve has been implicated as the cause of persistent nasal obstruction after septoplasty in up to 95% of cases.
NVD is a distinct cause of symptomatic nasal obstruction, yet there are several ambiguities surrounding the diagnosis and management of this process. The literature has often been confusing and occasionally contradictory in almost every aspect of management of the nasal valve. Discrepancies exist over the nomenclature and terminology, anatomy of the nasal valve, the desired effects of a particular technique, and appropriate outcome measures, just to name a few. In most outcomes studies, adjunctive procedures are often performed in addition to directed nasal valve correction, which potentially confounds the results. There is significant heterogeneity in study designs and lack of randomized controlled trials. Most studies are uncontrolled case series, which only recently have used validated outcome measures. This problem in the literature serves as an unfortunate imposition to quality clinical decision-making.
Although confusion may exist in the literature, there is in fact a good body of evidence supporting treatment of the nasal valve. Most of the evidence has been overwhelmingly positive. This article reviews the management of the nasal valve, highlighting the controversial aspects of this topic and addressing the current best practices available. The goal is not only to help the reader understand the challenges in the literature but also to provide a framework for thoughtful and effective management of this problem ( Box 1 ).
Anatomy
Terminology
Diagnosis
Objective outcome measures
Technique selection
Introduction
The ability to breathe through the nasal passages is a noticeable feature of healthiness and well-being. The nasal airway plays a central role in air heating and humidification, olfaction, and, most importantly, airflow. Obstruction of the nasal airway is a common complaint in the otolaryngologic practice and has a dramatic impact on patient quality of life. Although several medical and surgical treatments exist to address this common patient complaint, developing the best therapeutic strategy targeting the sources of the problem can be challenging. Often, there are multiple contributing factors complicating treatment.
The causes of nasal airway obstruction are legion, though they can typically be broken down to mucosal or structural causes. Structural causes of obstruction may be posttraumatic, idiopathic, or iatrogenic at the hands of the nasal surgeon. Underpinning all of this is an anatomic malformation or dysfunction. In fact, up to 75% to 85% of people have some type of anatomic deformity of the nose. Only a subset of these individuals experience a severe enough impact on quality of life to prompt a clinical evaluation.
Most otolaryngologists are adept at diagnosing anatomical deformities of the septum and turbinates. However, nasal obstruction from nasal valve dysfunction (NVD) may be overlooked as a contributor or sole cause of nasal obstruction. NVD has been implicated in having a role in up to 13% of adults complaining of chronic nasal obstruction. Moreover, the nasal valve has been implicated as the cause of persistent nasal obstruction after septoplasty in up to 95% of cases.
NVD is a distinct cause of symptomatic nasal obstruction, yet there are several ambiguities surrounding the diagnosis and management of this process. The literature has often been confusing and occasionally contradictory in almost every aspect of management of the nasal valve. Discrepancies exist over the nomenclature and terminology, anatomy of the nasal valve, the desired effects of a particular technique, and appropriate outcome measures, just to name a few. In most outcomes studies, adjunctive procedures are often performed in addition to directed nasal valve correction, which potentially confounds the results. There is significant heterogeneity in study designs and lack of randomized controlled trials. Most studies are uncontrolled case series, which only recently have used validated outcome measures. This problem in the literature serves as an unfortunate imposition to quality clinical decision-making.
Although confusion may exist in the literature, there is in fact a good body of evidence supporting treatment of the nasal valve. Most of the evidence has been overwhelmingly positive. This article reviews the management of the nasal valve, highlighting the controversial aspects of this topic and addressing the current best practices available. The goal is not only to help the reader understand the challenges in the literature but also to provide a framework for thoughtful and effective management of this problem ( Box 1 ).
Anatomy
Terminology
Diagnosis
Objective outcome measures
Technique selection
Anatomy
The nasal valve is an anatomically complex concept and is nonspecific in its original description. First suggested by Mink, the nasal valve was described as the region of maximal nasal resistance. It was later described by Bridger as the flow-limiting segment of the nasal airway located at the triangular aperture between the upper lateral cartilage (ULC) and septum. From the author’s perspective, the nasal valve is much more generic. In reality, the nasal valve encompasses the column of air housed by the mucosa, cartilage, and soft tissue of the nose external to the piriform aperture. This area is typically modified in some fashion during nasal valve surgery ( Fig. 1 ).
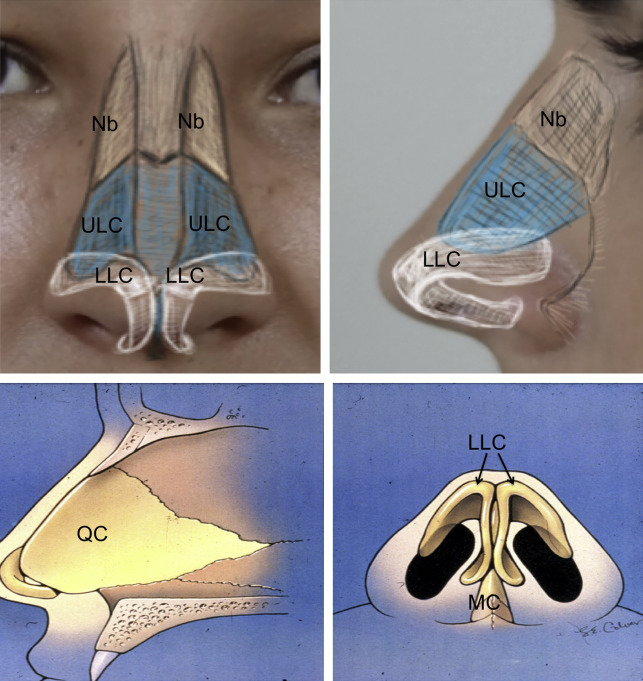
The two major components that comprise the nasal valve, the internal and external valves, are classically described in more anatomically specific terms. In most texts, the internal valve is the triangular cross-sectional area between the caudal border of the ULCs, the septum, the head of the inferior turbinate, and nasal floor. The normal angle at the junction of the caudal ULC and septum is 10° to 15° in the caucasian nose and usually more obtuse in asians and african americans. Of the entire nasal valve area, the internal valve is generally considered to be the narrowest portion and is the site of maximal airway resistance.
The external valve has classically referred to the area in the nasal vestibule, under the alar lobule, formed by the caudal septum, medial crura of the alar cartilages, alar rim, and nasal sill. It is important to note that, though the location and anatomy of the internal valve has been largely consistent in the literature, this has not been universally true regarding the external valve.
As an alternative to the classic definition of the external valve, Khosh and colleagues referred to the external valve as bound superolaterally by the caudal edge of the upper lateral cartilages, laterally by the piriform aperture and fibrofatty tissues of the ala, and the nasal floor. Spielmann and colleagues described the external nasal valve as being formed by the septum, the medial and lateral crura of the lower lateral cartilage (LLC), and the premaxilla. Ballert and Park used a separate term to describe the area between the internal and external valves. The intervalve area was defined as the caudal-lateral aspect of the lateral crus, including the fibrofatty tissue, which extends to the piriform aperture and immediately deep to the supra-alar crease.
Yet another way to consider the anatomy of the nasal valve is to divide it into 2 zones, as described by Most. In order to better characterize the points of lateral wall collapse, he described 2 zones where lateral wall collapse occurs. Zone 1 corresponds to the scroll region and inferior portion of the upper lateral cartilage, whereas zone 2 corresponds to the skin and soft tissues of the nasal ala, similar to the traditionally described external valve ( Fig. 2 ).
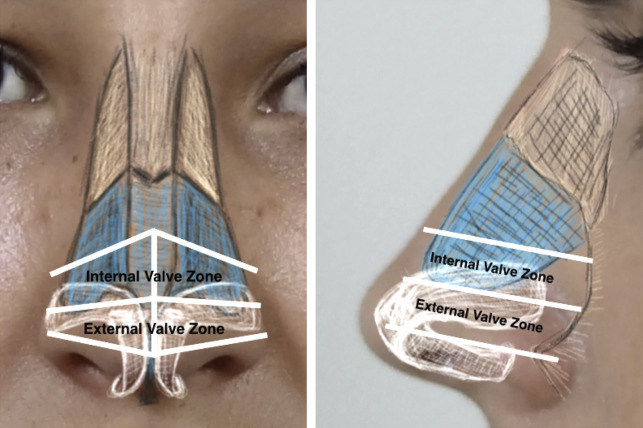
It is obvious that the anatomy of this region is complex, which has led to difficulties characterizing it in such a way that it can be treated in a standardized fashion. It is the authors’ opinion that, though using the characterizations of the internal and external valves can be helpful for communication and surgical planning, it is important to be as specific as possible in regard to the anatomic structures affected by the pathologic process in order to select the best possible surgical technique.
Physiology
Normal airflow through the nasal valve depends on the Bernoulli principle and Poiseuille’s law. The Bernoulli principle states that as the flow of air increases through a fixed space, the pressure in that space decreases. If the decrease in pressure overcomes the inherent rigidity of the flexible nasal sidewall, collapse can occur resulting in obstruction. Clinically, the collapse of the nasal sidewall during inspiration is termed dynamic obstruction .
Pouseille’s law states that flow is inversely proportional to the fourth power of the radius, which means that small decreases in the radius of a space have dramatic impacts on the flow of air through the nose. In the clinical setting, an anatomically narrowed portion of the nasal valve is defined as a static obstruction.
All surgical techniques in the management of the nasal valve are focused on optimizing the aforementioned physical principles. Surgical maneuvers either increase the cross-sectional area of the valve, strengthen the nasal sidewall to resist dynamic collapse, or both.
Terminology
The terminology regarding nasal valve management is varied, confusing, and in need of standardization. There are several terms in the literature that reference pathology of the nasal valve as well as its component structures, the internal and external nasal valves. Some of the terms in the literature referencing the valve include NVD, nasal valve collapse, nasal valve compromise (NVC), and nasal valve stenosis. Similar terms have been applied to both the internal and external valves.
The use of some of these terms can be misleading. For example, nasal valve collapse has been used to reference both insufficiency and weakness of the nasal sidewall and narrowing of the internal nasal valve. The former is a function of a dynamic problem whereby the sidewall collapses with inspiration, whereas the latter is a static and constant narrowing of the valve. Both clinical entities are managed differently. This point highlights the need for standardized nomenclature that accurately describes the clinical problem at hand.
The use of the terms NVC or NVD when referencing a general pathologic issue affecting the nasal valve is least confusing. The former is the term used in a recent clinical consensus statement, whereas the latter has been proposed as an alternative that avoids confusion with the term nasal valve collapse if abbreviated.
When referencing the pathology of the internal or external nasal valves, it is important to distinguish between narrowing, which is a static process, or collapse, which is dynamic. In regard to the internal nasal valve, in most cases, the process is static. The main components of the internal valve, the caudal ULC, septum, and inferior turbinate, typically do not vary dynamically during nasal inspiration. Therefore, internal valve narrowing is preferred in such cases. This narrowing often results from trauma or previous rhinoplasty in which weakening of the ULC support structures resulted in a narrowed angle. If indeed there is dynamic collapse of the caudal ULC with inspiration at the internal valve, then internal nasal valve collapse should be used instead. Dynamic collapse of the internal nasal valve can be seen in patients with an overprojected septal cartilage seen commonly in tension nose deformities. These patients have thin skin and weak ULC prone to dynamic collapse with inspiration, which can be seen on frontal inspection as collapse of the middle third with inspiration.
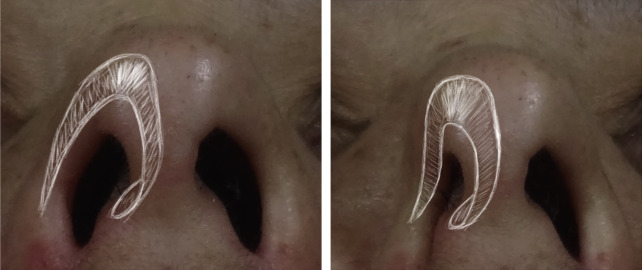
Dysfunction of the external valve is more commonly the result of a dynamic process. As it is classically described, external valve collapse occurs at the alar rim and is visible externally, most notably on the base view ( Fig. 3 ). However, collapse of the nasal sidewall can in fact occur at different points and is not simply confined to the classically described external valve. Ballert and Park noted that the epicenter of nasal sidewall collapse is often at the intervalve area, which is cephalic to the classically defined external valve and immediately deep to the supra-alar crease. Most and Lee and Most described 2 zones of lateral sidewall collapse. In his description, Most noted that collapse can occur either in zone 2 at the area of the classic external valve or in zone 1, which is more cephalad at the scroll region and corresponds to the Ballert and Park intervalve area. If the term external valve collapse is used to describe dynamic collapse in this region, it would be helpful to also provide a more specific description of the location of collapse as suggested by Most. In cases of a static problem involving the external valve, such as a severe caudal septal deviation or lateralization of the medial crura without a dynamic problem, external valve narrowing should be used.
Historical perspective
Traditionally, treatment of nasal obstruction centered on a septoplasty. The original submucous resection (SMR) consisted of removal of the deviated portion of the septum with preservation of a dorsal and caudal strut (L-strut). The SMR was made popular by Killian and Freer in early 1900s; however, this technique failed to address the dorsal or caudal portions of the septum. In 1948, Cottle and Loring advocated an incision at the mucocutaneous junction instead of the Killian incision as well as addressing all deviated portions of the bony and cartilaginous septum. Multiple techniques have since developed to address various types and locations of septal deviations while preserving structural support. Unfortunately, both the literature and experience have shown that septoplasty alone is often an insufficient means of treating nasal obstruction in isolation. Success rates of septoplasty have ranged from 43% to 85% depending on the assessment tool used.
The inferior turbinates were another surgical target identified causing nasal obstruction. Many techniques have been described to treat enlarged turbinates. Initial procedures centered around inferior turbinate resection, though this resulted in significant morbidity, including empty nose syndrome, rhinitis sicca, and atrophic rhinitis.
More recently, surgery for the inferior turbinate has shifted to reductive techniques with better outcomes and less morbidity. Inferior turbinate reduction has shown to be effective in improving nasal obstruction due to inferior turbinate hypertrophy, though many of the studies had a short follow-up period. A study by Garzaro and colleagues showed improvement in the Nasal Obstruction Symptom Evaluation (NOSE) scores at the 2-year mark in patients who underwent inferior turbinate reduction by radiofrequency ablation. It is important to note that the preoperative symptom severity of this group preoperatively was relatively low (mean preoperative NOSE score: 23.14). A recent randomized controlled trial of patients undergoing septorhinoplasty with or without inferior turbinate reduction showed no improvement in quality-of-life outcome measures between the groups. Although turbinate reduction is a useful adjunctive technique where indicated, it is unlikely to be effective when used in isolation, especially with other concomitant pathologies.
The need to address the nasal valve as a contributor to nasal obstruction was not recognized until 1984, when Sheen first described the use of spreader grafts to open the internal nasal valve. Sheen recognized the need to correct the nasal dorsum following hump reduction and avoid a narrowed middle vault and inverted V deformity. The spreader graft was noted to increase the angle of the internal valve by laterally displacing the ULC subsequently recreating aesthetic lines. Since Sheen’s article, the spreader graft has become the gold standard for management of the internal nasal valve. However, this technique alone is often not sufficient in isolation to effectively manage the nasal valve. Today, there are several surgical techniques to target specific areas of NVC.
Diagnosis
Diagnosis of NVD is based on history and physical examination. Subjective assessment should include onset, laterality, duration, exacerbating and alleviating factors, trauma, history of nasal surgery, and impact on daily life. A history of use of nasal splints, such as BreatheRight Strips (CNS Inc, Minneapolis, MN), and their effectiveness is helpful as it may provide an indication of surgical success. Physical examination should include inspection of the outward appearance, palpation, and intranasal examination. External inspection should include evaluation of the nose on frontal, lateral, and base views in both the natural state and during inspiration. A pinched middle third, evident on frontal view, should provoke suspicion of internal valve dysfunction. Tip bossae, deep supra-alar creases, and medial sidewall movement on deep inspiration indicate a potential nasal sidewall issue. Manual palpation should also be performed, as this provides information on the inherent strength of the nasal cartilages, alar rim strength, and nasal tip support.
Internal inspection should be performed to evaluate septal deviation, inferior turbinate hypertrophy, lateral crural recurvature, lateral wall collapse, and valve narrowing. Some advocate the use of nasal endoscopy to evaluate the internal nasal valve ; however, there is no consensus regarding routine usage.
The Cottle maneuver has historically been a popular examination technique and involves stenting the nasal sidewall with lateral traction on the cheek. This maneuver is nonspecific in that it enhances nasal airflow even in patients without NVC. The modified Cottle maneuver involves the use of an ear curette or Q-tip to stent the lateral nasal sidewall and has been proposed as an alternative diagnostic tool. This maneuver is thought to be predictive of surgical outcomes. Interestingly, only one study was found in the authors’ review supporting the predictive ability of the modified Cottle on postoperative outcomes. Fung and colleagues used the rhinoplasty outcomes evaluation, a validated quality-of-life survey, to show that the modified Cottle maneuver was predictive of positive surgical outcomes.
Objective outcome measures
Objective measures in nasal valve surgery serve 2 purposes. They are useful in the assessment of clinical outcomes determining whether surgery accomplished the goal of improving patient outcomes. Secondly, and perhaps most importantly, these measures would theoretically have diagnostic utility in predicting surgical success. Such measures would ideally be inexpensive, readily accessible, and easy to administer. Unfortunately, no such tool currently exists. Most objective measures are cumbersome and difficult to administer, belying their clinical utility. Likewise, objective measures have been often incongruous with patient-reported severity of nasal valve obstruction.
Although measures may show an effective surgical change, the correlation with improved patient symptoms has not been definitively shown with any objective measure. A recent systematic review correlating objective outcome measures with subjective sense of nasal patency found several studies with conflicting findings. Likewise, in a consensus statement by Rhee and colleagues, a panel of experts did not find imaging, acoustic rhinometry, or rhinomanometry useful in clinical diagnosis.
Nonetheless, the current perspective on objective measures in nasal valve surgery may change as new methods are designed and better clinical investigations are performed. The objective measures currently used in assessment of NVC include acoustic rhinometry, rhinomanometry, peak nasal inspiratory flow, and computed tomography (CT) imaging.
Acoustic rhinometry uses reflected acoustic pulses to calculate the nasal cross-sectional area. Nasal volumes can be calculated from a series of cross-sectional area measurements. Acoustic rhinometry has been found to correlate well with other objective measures; consequently, hundreds of studies have used this objective measure in clinical research. Acoustic rhinometry has not been found to correlate well with subjective outcomes.
Rhinomanometry is an objective physiologic measure that evaluates transnasal pressure and nasal airflow volume to calculate nasal airway resistance during inspiration. Nasal peak inspiratory flow is another noninvasive physiologic tool that measures maximum airflow during a forced nasal inspiration. Although this method has been validated against rhinomanometry, this tool depends on patient effort and pulmonary function and, therefore, may not be consistently reliable.
CT imaging has shown promise as an objective measure as it is readily available to the clinician and can directly measure nasal dimensions and the angle of the internal nasal valve. It has been successfully validated against acoustic rhinometry. However, as with the other objective measures, there has been limited evidence supporting the correlation of CT imaging to subjective outcomes. One study by Menger and colleagues did find a correlation between improved postoperative NOSE scores and the change in minimal cross-sectional area on CT, though the validity of this correlation is questioned as the statistical analysis seems to have violated the principle of statistical independence in their analysis.
Recently, clinician-derived measures have been developed to allow the clinician to standardize physical examination findings in assessing surgical outcomes. Tsao and colleagues developed a methodology for description of lateral sidewall insufficiency. In this method, the clinician evaluates each nasal sidewall zone, as previously defined earlier, and rates collapse on a scale of 0 to 3. This measure has been validated in reporting surgical outcomes, though its use has remained limited.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





