Classification
Assessment criteria
Minor burn injury
<15% TBSA burn in adults <40 years age
<10% TBSA burn in adults >40 years age
<2% TBSA full-thickness burn without risk of functional or esthetic impairment or disability
Moderate uncomplicated burn injury
15–25% TBSA burn in adults <40 years age
10–20% TBSA burn in adults >40 years age
<10% TBSA full-thickness burn without functional or esthetic risk to burns involving the face, eyes, ears, hands, feet, perineum, or major joints
Major burn injury
>25% TBSA burn in adults <40 years age
>20% TBSA burn in adults >40 years age
OR >10% TBSA full-thickness burn (any age)
OR injuries involving the face, eyes, ears, hands, feet perineum, or major joints, likely to result in functional or esthetic disability
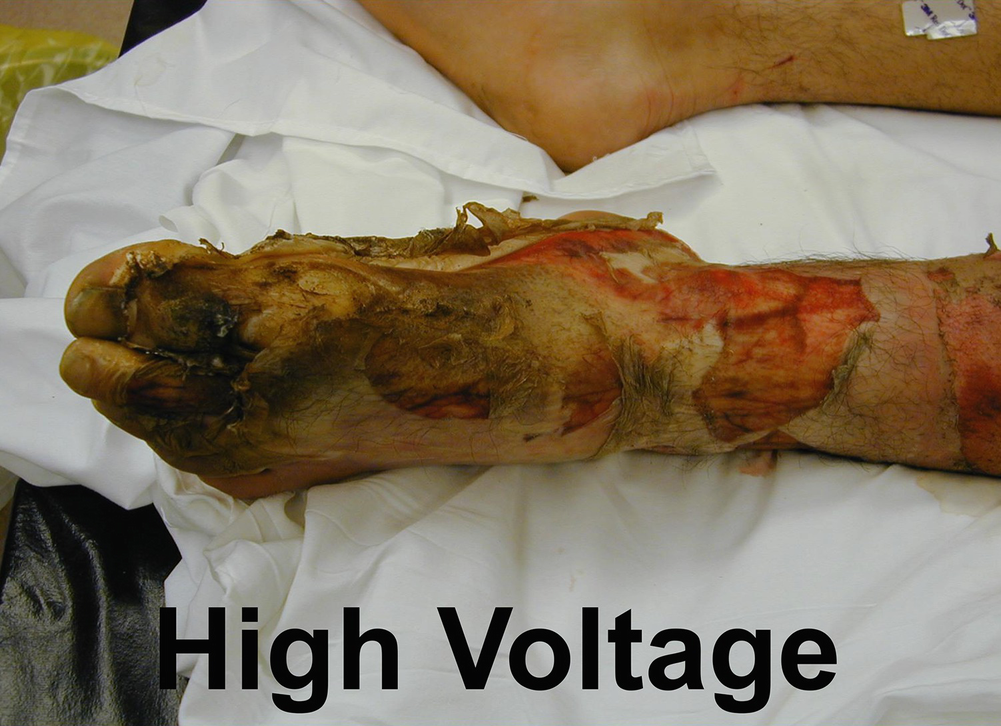
OR high-voltage electrical burn
OR all burns with inhalation injury or major trauma
27.2.4 Etiology and Risk Factors
Causes of burn injuries
Home and leisure | Workplace |
|---|---|
• Hot water heaters set too high (140 °F or 60 °C) • Overloaded electrical outlets • Frayed electrical wiring • Carelessness with cigarettes, lighters, matches, candles • Pressure cookers • Microwaved foods and liquids • Hot grease or cooking liquids • Open space heaters • Gas fireplace doors • Radiators • Hot water bottles and heating pads • Hot sauna rocks • Improper use of flammable liquids: – Starter fluids – Gasoline – Kerosene • Electrical storms • Overexposure to sun | • Electricity: – Power lines – Outlet boxes • Chemicals: – Acids – Alkalis • Tar • Hot steam sources: – Boilers – Pipes – Industrial cookers • Hot industrial presses • Flammable liquids: – Propane – Acetylene – Natural gas |
27.3 Pathophysiology
27.3.1 Severity Factors
There are five factors to be considered when determining the severity of a burn injury (Box 27.1).
Box 27.1 Burn Severity Factors
- 1.
Extent of body surface area burned
- 2.
Depth of tissue damage
- 3.
Age of person
- 4.
Part of body burned
- 5.
Past medical history
- 1.
Extent—There are several, paper-based methods available to accurately calculate the percentage of body surface area involved. The simplest and most easily recalled is the Rule of Nines (Fig. 27.1). However, it is only for use with the adult burn population. The Lund and Browder method (Fig. 27.2) is useful for all age groups, but is more complicated to use. For the pediatric population, there is a modified version of the Lund and Browder method (Fig. 27.3). If the burned areas are small and irregularly shaped, the Rule of Palm can be used. The palmer surface of the burned person’s hand, including the extended fingers, represents 1% body surface area. Reliability of the palmar surface area tool for obese patients has been questioned and alternative methods suggested [11]. There are also a number of internet-based or mobile technologies available to calculate the extent of the body burn, which might help to decrease the problems with both over- and under-estimation of burn size by pre-hospital, hospital, and burn team personnel [12–16].
- 2.
Depth—Two factors determine the depth of a burn wound—temperature of the burning agent and duration of exposure time. Previously, the terminology used to describe burn depth was first, second, and third degree. In recent years, these terms have been replaced by those more descriptive in nature: superficial partial-thickness, deep partial-thickness, and full-thickness (Table 27.3). The skin is divided into three layers, which include the epidermis, dermis, and subcutaneous tissue (Fig. 27.4). The dermis, which is about 30–45 times thicker that the epidermis, contains connective tissue, blood vessels, hair follicles, nerve endings, sweat glands, and sebaceous glands. Skin-reproducing cells are located along the shafts of the hair follicles, sweat glands, and sebaceous glands. The sufficient presence or absence of these re-epithelializing cells determines whether the wound will heal on its own or require skin grafting. At the present time, visualization with the naked eye, by experienced burn practitioners, is used to determine burn depth. However, there is ongoing research exploring the use of newer laser technologies to determine burn depth [17].
- 3.
Age—In patients less than 2 years of age and greater than 50, there is a higher incidence of morbidity and mortality. Infants, toddlers, and the elderly have thinner skin, making the risk of a deeper burn greater in these age groups. Persons of this age also have weaker physical resources to mount a resistance against the debilitating effects brought on by a burn [18, 19].
- 4.
Part of the body burned—Patients with burns to the face, eyes, neck, hands, feet, joints, or perineum have greater functional and esthetic challenges to overcome and require the specialized care offered by a burn center.
- 5.
Past medical history—A burn injury will exacerbate pre-existing conditions. Persons with diabetes or peripheral vascular disease have a more difficult time with wound healing, a central factor in burn recovery, particularly if the burns are on the legs and/or feet [20, 21]. Burn patients with poor nutritional status pre-burn or with previous drug and/or alcohol abuse patterns have fewer physical reserves to draw from and, as such, require more resources for a prolonged period of time.
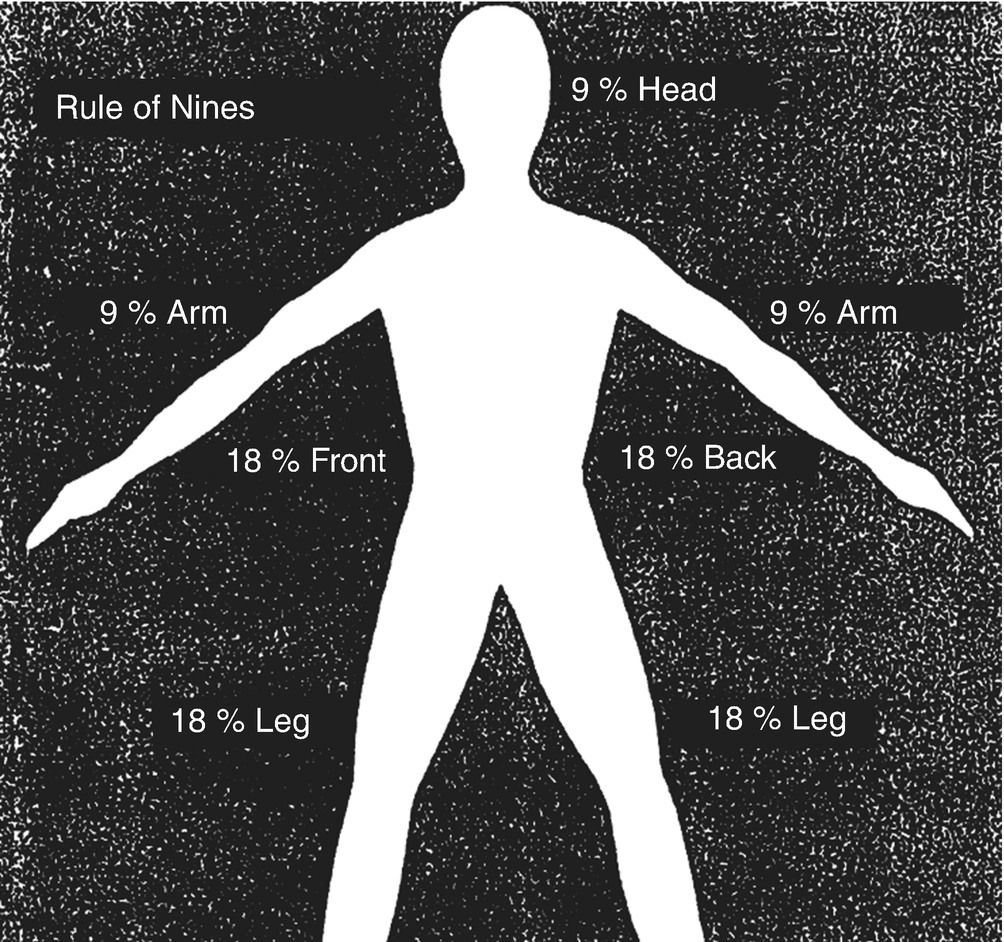
Rule of Nines method for estimating extent of burn
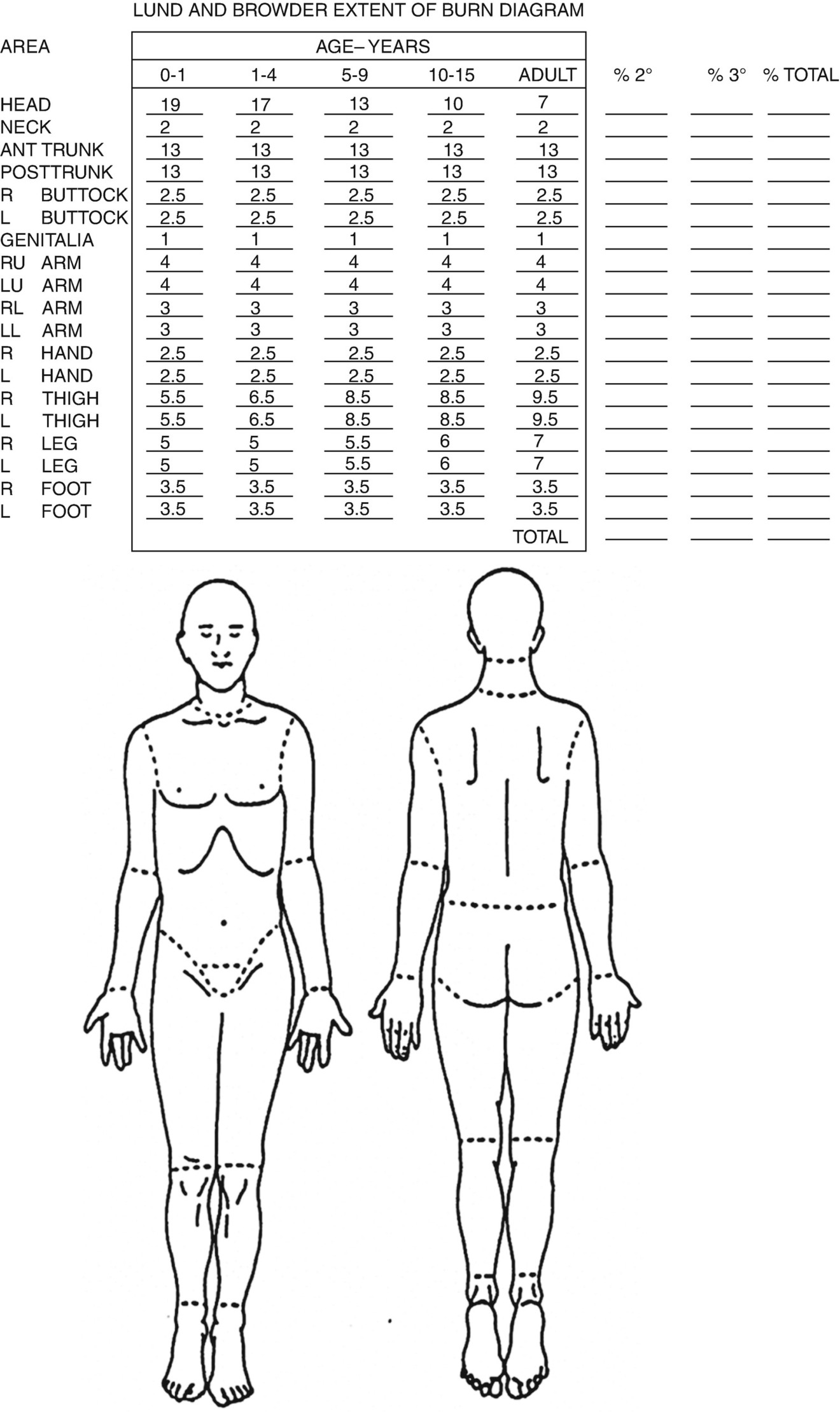
Lund and Browder method for estimating extent of burn
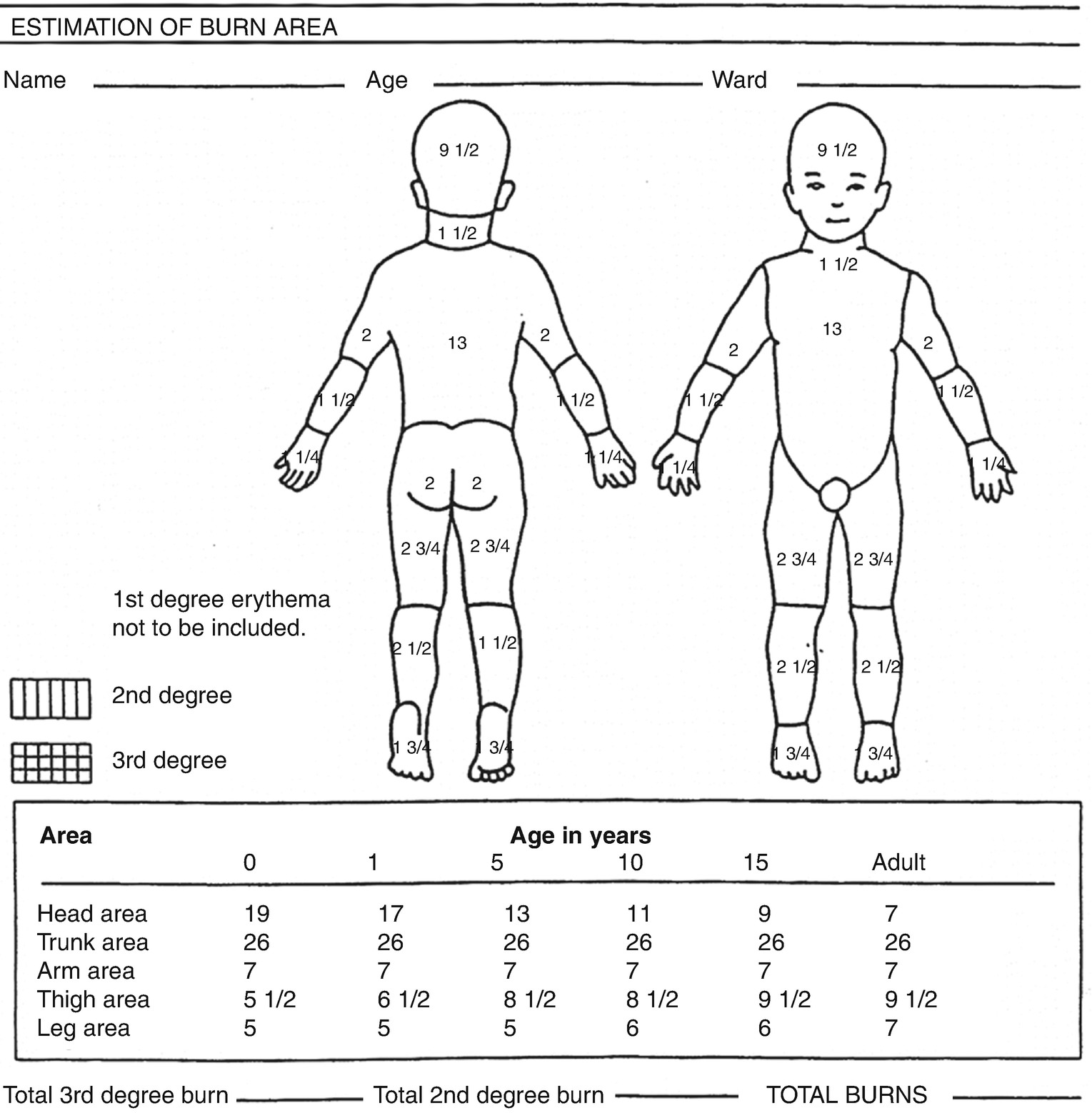
Pediatric estimation of burn area using modified Lund and Browder
Classification of burn injury depth
Degree of burn | Cause of injury | Depth of injury | Appearance | Treatment |
|---|---|---|---|---|
First degree | Superficial sunburn Brief exposure to hot liquids or heat flash | Superficial damage to epithelium Tactile and pain sensations intact | Erythematous, blanching on pressure, no blisters, sensate | Complete healing within 3–5 days with no scarring |
Superficial partial-thickness (second degree) | Brief exposure to flame, flash, or hot liquids | Destruction of epidermis, superficial damage to papillary layer of dermis, epidermal appendages intact | Moist, weepy, blanching on pressure, blisters, pink or red color, sensate | Complete healing within 14–21 days with no scarring |
Deep partial-thickness (deep second degree) | Exposure to flame, scalding liquids, or hot tar | Destruction of epidermis, damage to reticular layer of dermis, some epidermal appendages intact | Pale and less moist; no blanching or prolonged, deep pressure sensation intact, pinprick sensation absent | Prolonged healing time usually >21 days with scarring. Skin grafting may be necessary for improved functional and esthetic outcome |
Full-thickness (third degree) | Prolonged contact with flame, steam, scalding liquids, hot objects, chemicals, or electrical current | Complete destruction of epidermis, dermis and, epidermal appendages; injury through most of the dermis | Dry, leathery, pale, mottled brown or red in color; visible thrombosed vessels insensitive to pain and pressure | Requires skin grafting |
Full-thickness (fourth degree) | Major electrical current, prolonged contact with heat source (i.e., unconscious patient) | Complete destruction of epidermis, dermis, and epidermal appendages; injury involving connective tissue, muscle, and bone | Dry, black, mottled brown, white or red; no sensation and limited movement of burned limbs or digits | Requires skin grafting and likely amputation |
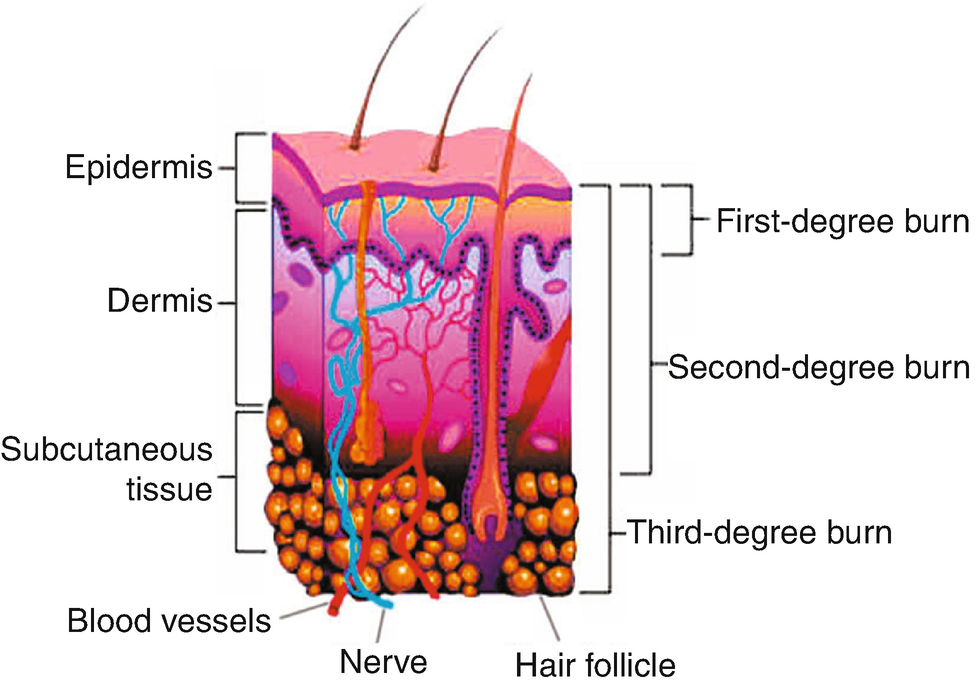
Anatomy of burn tissue depth
27.3.2 Local Damage
Local, burn wound damage varies, depending upon the temperature of the agent, duration of contact time, and the type of tissue involved. The deepest zone of damage, coagulation (full-thickness), is the site of irreversible cell death, where blood vessels and re-epithelializing cells have been completely destroyed. These areas require skin grafting for permanent coverage. The middle layer, or zone of stasis, is the area of deep, partial-thickness injury where there are some skin-reproducing cells present in the dermis and circulation to the area is partially intact. Healing will occur generally within 14–21 days, as long as infection or desiccation is prevented. The outermost zone of hyperemia is the area of least damage. This superficial, partial-thickness wound has minimal cell involvement and will generally recover spontaneously within 7–10 days. Areas of partial-thickness injury , devoid of infection and desiccation, will heal by primary intention from the edges of the wound and from below. Full-thickness wounds require early excision and skin grafting. Over time, the collagen fibers and re-epithelializing cells continue to heal and add strength to the newly formed tissue. The healed areas initially look pale and flat. However, as the blood supply increases to those areas over the next month or so, they become red and raised. In addition to these scars forming, there is a natural tendency for burned tissue to shorten and contractures to develop. Over the next year to 18 months, the burn scars will fully mature and become less red and less raised [22, 23].
27.3.3 Fluid and Electrolyte Shifts
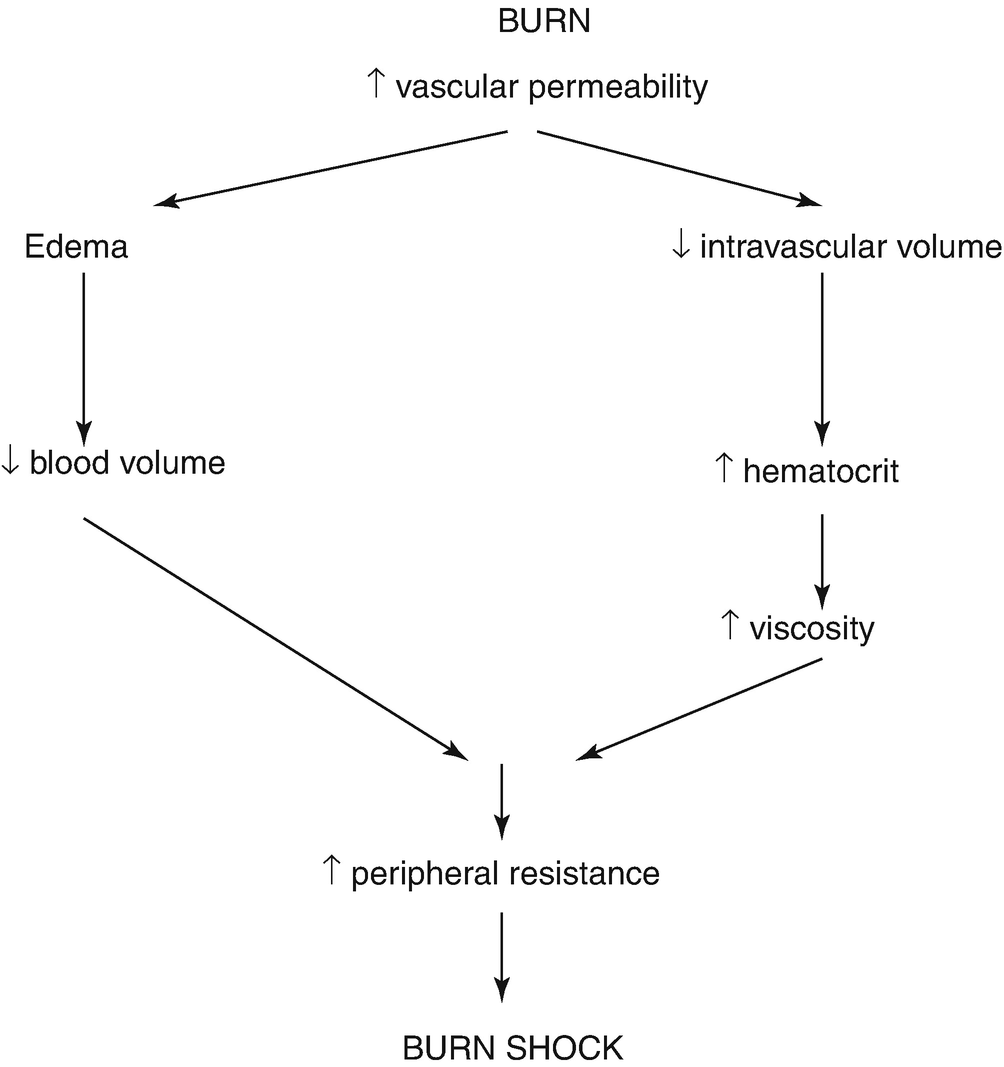
Burn shock
27.4 Types of Burn Injuries
Burns can be grouped into numerous categories: thermal, chemical, electrical, and smoke/inhalation. The causative agent does influence both the management and outcome of each injury.
27.4.1 Thermal
Causes of thermal burns
Cause | Examples |
|---|---|
Dry heat—Flame | • Clothing catches on fire • Skin exposed to direct flame |
Dry Heat—Flash | • Flame burn associated with explosion (combustible fuels) |
Moist Heat—Hot liquids (scalds) | • Bath water • Beverages—coffee, tea, soup • Cooking liquids or grease |
Moist Heat—Steam | • Pressure cooker • Microwaved food • Overheated car radiator |
Contact—Hot surfaces | • Oven burner and door • Barbecue grill |
Contact—Hot objects | • Tar • Curling iron • Cooking pots/pans • Heating pad • Hot water bottle |

Flame burn

Scald burn
27.4.2 Chemical

Chemical burn
27.4.3 Electrical
Electrical burn
The person, who has sustained an electrical burn injury, may have also experienced cardiac arrhythmias or asystole post-injury. Immediate CPR is essential following cardiac arrest. He/she then continues to be at risk for cardiac arrhythmias for 24 h post-burn and must be monitored and have an electrocardiogram performed on admission to hospital.
Severe metabolic acidosis develops shortly after the injury occurs because of extensive tissue destruction and cell rupture. Assessment includes arterial blood gas analysis and, if needed to maintain normal serum pH levels, infusions of sodium bicarbonate. The kidneys also need to be closely monitored because of potentially high circulating levels of hemoglobin from damaged red blood cells and myoglobin from damaged muscle. In small amounts, the kidney tubules can filter them sufficiently. In larger concentrations, however, there is a significant risk of developing acute tubular necrosis and possible renal failure. Treatment consists of the early initiation of Lactated Ringer’s solution at a rate that maintains a good urinary output of between 75 and 100 mL/h until the color of the urine is sufficient to suggest adequate dilution. In addition, an osmotic diuretic (e.g., mannitol) is usually given to establish and maintain acceptable urinary output.
27.4.4 Smoke and Inhalation Injury

Inhalation injury
- 1.
Inhalation injury above the glottis. Most smoke/inhalation injury damage (60%) is limited to the upper airway (pharynx, larynx, vocal cords) since the vocal cords and glottis close quickly as a protective mechanism following exposure to smoke or thermal agents, such as hot air or steam. There is redness and blistering. Edema and the onset of rapid airway obstruction, resulting in a respiratory emergency, are the primary concerns with this type of inhalation injury.
- 2.
Inhalation injury below the glottis. Most injuries below the glottis are chemically produced through the inhalation of noxious products of combustion, resulting in tracheobronchitis. Major airway involvement (tracheobronchial tree) occurs about 30% of the time, with bronchopneumonia being the chief concern. Patients may not show symptoms until 12–24 h post-burn . Since gases are usually cooled before they reach the lung parenchyma, there is only a 10% injury occurrence at the level of the terminal bronchioles and alveoli. Primary concerns are pulmonary edema and adult respiratory distress syndrome (ARDS).
- 3.
Carbon monoxide and hydrogen cyanide poisoning . Most fatalities at a fire scene are caused by carbon monoxide, hydrogen cyanide poisoning, or asphyxiation. Carbon monoxide is produced by the incomplete combustion of burning materials. It then displaces the oxygen being carried by the hemoglobin molecules, resulting in less oxygen being delivered throughout the body. Carboxyhemoglobin and hydrogen cyanide levels should be measured, following admission of the person to an emergency department or burn center (Table 27.5). Treatment consists of aggressive fluid resuscitation and the administration of 100% humidified oxygen.
Signs and symptoms of carbon monoxide poisoning
Carboxyhemoglobin saturation (%) | Signs and symptoms |
|---|---|
5–10 | Visual acuity impairment |
11–20 | Flushing, headache |
21–30 | Nausea, impaired dexterity |
31–40 | Vomiting, dizziness, syncope |
41–50 | Tachypnea, tachycardia |
>50 | Coma, death |
27.5 Clinical Manifestations
Recovery from a burn injury involves successful passage through three phases of care: emergent, acute, and rehabilitative. Principles of care for the emergent period involve resolution of the immediate problems resulting from the burn injury. The time required for this to occur is usually 1–2 days. The emergent phase ends with the onset of spontaneous diuresis. Principles of care for the acute period include avoidance, detection and treatment of complications, and wound care. This second phase of care ends when the majority of burn wounds have healed. During the third, and final, phase of rehabilitative care, the goals are for the burn patient to return to an optimal place in society and to accomplish any remaining functional and cosmetic reconstruction. This phase ends when there is complete resolution of any outstanding clinical problems resulting from the burn injury.
27.5.1 Subjective Symptoms
It is essential, throughout all phases of a burn patient’s recovery, to seek out his/her perspective, when possible, and attempt to incorporate individual wishes into the plan of care. During the emergent period, patients and their families are likely in a state of physical and psychological shock. As a result of hypoxia, patients may also be disoriented or not able to recall what happened. Others remain very lucid throughout the ordeal and recall events with remarkable clarity. Some may not realize how serious their injuries are and be unrealistic about the care they require. Others may be intubated and sedated and not be aware for weeks to come. Pain may be a concern, while some may experience little discomfort. Thirst may be a symptom, depending upon the degree of fluid loss.
Some may complain of feeling cold or shiver as a result of heat loss, anxiety, and pain. The combination of hypovolemic shock, facial edema, intubation, and analgesics/sedative agents may alter a patient’s sensory perception significantly over the first few days post-injury. If he/she is able to talk, common themes include “Will I die? What happened? Why me? I can’t believe this is happening.” In the acute phase, patients may experience varying levels of pain during dressing changes and physical/occupational therapy and might describe significant muscular discomfort, resulting from functional positioning and use of splinting materials. Unable to do any number of self-care activities, patients may become very frustrated about how dependent they have become on others. Concerns may be expressed regarding finances, family, and work obligations. Adaptation to the hospital environment and necessary treatments may absorb a considerable amount of the patient’s physical and emotional energy. Adjustment to a variety of losses (personal and property), feelings of grief, guilt and blame, a need for information about what to expect over the coming weeks, and a search for meaning behind the event, are also experienced. Patients may feel angry or depressed post-injury. Relationships with family may become strained as everyone seeks to readjust and cope with this unexpected and traumatic event. During the rehabilitative phase of care, patients come to realize that they have completed the most difficult part of their recovery. However, many experience impatience with the time required for complete healing and physical rehabilitation. There is usually a desire to resume as much independence as possible, sometimes coupled with slight fear and hesitation about leaving the protective environment of the burn center. Questions, such as “What will it be like when I leave the hospital? How will I manage when the nurses and therapists are no longer around to help?” reflect the primary concerns for patients and family members at this time. There may be concerns about resumed sexual intimacy with a partner and self-acceptance of an altered body image. A request may be made to speak with a recovered burn survivor, who can offer words of support and advice based on personal experience. Over time, burn patients express feelings of pride at having overcome such tremendous physical and emotional challenges and begin to reflect on the path their lives will take post-burn as they move from burn “victim” to “survivor” and, perhaps, burn “thriver.”
27.5.2 Objective Signs
The initial assessment of the burn patient is like that of any trauma patient and can best be remembered by the simple acronym “ABCDEF” (Box 27.2). Recently, recommendations for burn care management have been published to address the educational needs of both non-burn and burn specialists around the world [25, 26]. During the emergent period, burn patients quickly begin to exhibit signs and symptoms of hypovolemic shock (Box 27.3). Lack of circulating fluid volumes will also result in minimal urinary output and absence of bowel sounds. The patient may also be shivering due to heat loss, pain, and anxiety. If inhalation injury is a factor, the patient may demonstrate a number of physical findings upon visual assessment, laryngoscopy, and fiberoptic bronchoscopy (Box 27.4). The patient likely experiences pain, as exhibited by facial grimacing, withdrawing, and moaning when touched, particularly if the injuries are partial-thickness in nature. Some areas of full-thickness burn may be anesthetic to pain and touch, if the nerve endings have been destroyed. The loss of sensation may be temporary if the nerves have been compressed by resulting edema in the hypovolemic shock phase. It is important to examine areas of circumferential full-thickness burn for signs and symptoms of vascular compromise, particularly the extremities (Box 27.5).
Box 27.2 Primary Survey Assessment
A—Airway
B—Breathing
C—Circulation
C-spine immobilization
Cardiac status
D—Disability
Neurological Deficit
E—Expose and evaluate
F—Fluid resuscitation
Box 27.3 Signs and Symptoms of Hypovolemic Shock
Restlessness, anxiety
Skin—pale, cold, clammy
Temperature below 37 °C
Pulse is weak, rapid, ↓ systolic BP
Urinary output <20 mL/h
Urine specific gravity >1.025
Thirst
Hematocrit <35; BUN ↑
Box 27.4 Physical Findings of Suspected Inhalation Injury
Deep facial burns
History of being trapped in an enclosed space/exposed to smoke
Laryngoscopic examination shows vocal cord swelling
Box 27.5 Signs and Symptoms of Vascular Compromise
Pallor
Deep tissue pain
Progressive paresthesias
Diminished or absent pulses
Sensation of cold extremities
Areas of partial-thickness burn appear reddened, blistered, and edematous. Full-thickness burns may be dark red, brown, charred black, or white in color. The texture is tough, leathery, and no blisters are present.
If the patient is confused, health care professionals need to determine if it is the result of hypovolemic shock, inhalation injury, substance abuse, pre-existing history or, more rarely, head injury sustained at the time of the trauma. It is essential to immobilize the c-spines until a full assessment can be performed and the c-spines cleared. At this time, a secondary survey assessment is performed (Box 27.6). Additional objective data can then be collected, analyzed, and a plan of care developed, which includes a set of Admission Orders. In the acute phase, the focus is on wound care and prevention/management of complications. At this point, the burn wounds should have declared themselves as partial-thickness or full-thickness in nature. Eschar on partial-thickness wounds is thinner and, with dressing changes, it should be possible to see evidence of eschar separating from the viable wound bed. Healthy, granulation tissue is apparent on the clean wound bed, re-epithelializing cells are seen to migrate from the wound edges, and the dermal bed will slowly close the wound within 10–14 days. Full-thickness wounds have a thicker, leathery eschar, which does not separate easily from the viable wound bed. Those wounds require surgical excision and grafting. Continuous assessment of the patient’s systemic response to the burn injury is an essential part of an individualized plan of care. Subtle changes, quickly identified by the burn team, can prevent complications from occurring or worsening over time. Physical examination by burn team staff and specialist consultants, laboratory tests, and diagnostic procedures will assist in the rapid identification and treatment of complications.
Box 27.6 Secondary Survey Assessment
Head-to-toe examination
Rule out associated injuries
Pertinent history
circumstances of injury
medical history
During the final, rehabilitative phase, attention turns to scar maturation, contracture development, and functional independence issues [27–29]. The areas of burn, which heal either by primary intention or skin grafting, initially appear red or pink and are flat. Layers of re-epithelializing cells continue to form and collagen fibers in the lower scar tissue add strength to a fragile wound. Over the next month, the scars may become more red from increased blood supply and more raised from disorganized whorls of collagen and fibroblasts/myofibroblasts. The scars are referred to as hypertrophic in nature. If oppositional forces are not applied through splinting devices, exercises, or stretching routines, this new tissue continues to heal by shortening and forming contractures. A certain amount of contracture development is unavoidable, but the impact can be lessened through prompt and aggressive interventions.
The scar maturation process takes anywhere from 6 to 18 months. During this time, the scars will progress from a dark pink/red to a pale pink/whitened appearance. The final color is usually lighter than the surrounding unburned skin. For people with darkly pigmented skin, the process of color return may be prolonged as the melanocytes work to produce pigment in the areas where it has been lost [30]. Increasing amounts of pressure may be necessary to gently and continually flatten the scars which, in turn, push the extra blood from the area, making them lighter in color. Custom-fitted pressure garments and/or acrylic face masks apply constant pressure over a gradual wearing period of up to 23½ h a day [31]. Extra pressure over concave and difficult-to-fit areas can be provided through elastomer inserts or silicone sheeting under the garments or face mask [32]. The length of time a person might have to wear the garments varies, but is in the range of 1–1½ years, depending upon the intensity of the scarring and the body’s response to pressure therapies. Patients will often experience itchiness and dry skin [33]. One of the best ways to decrease the itchiness is to get at the source of the problem: the dry skin. However, burned skin is different from healthy skin. Once the skin has been damaged by a burn injury, there are less natural oils available since the oil-reproducing glands have been destroyed, in whole or in part. In other words, the skin is “internally” dry as opposed to “externally” dry, such as when hands get chapped in the cold weather. Burned skin benefits from products that will be absorbed through the outer layer of the epidermis into the dry, dermal tissues. Water-based products do this. The more predominant products available are oil-based and contain mineral oil, petrolatum or paraffin. These ingredients coat the surface of the skin and, in essence, block the pores. This prevents loss of natural oils from the dermis, oils which burned skin is lacking. These ingredients are not absorbed into the dry dermis and do not bring moisture back into the skin. Mineral oil also breaks down elastic fibers in pressure garments and should be avoided. Suggested water-based products include Vaseline® Intensive Care Advanced Repair or Smith and Nephew’s Professional Care®. Medications, such as diphenhydramine (<Atarax>, <Benadryl>), gabapentin (<Neurontin>), or pregabalin (<Lyrica>) can also be ordered to help with moderate to severe itchiness on a short-term basis, as can massage therapy.
27.6 Diagnostic Findings
There are a number of baseline diagnostic studies used to monitor a patient’s clinical condition at the time of the injury and evaluate responses to care throughout the recovery period. They include laboratory tests, such as complete blood cell count (CBC), hemoglobin and hematocrit, group and screen, serum electrolyte levels, blood glucose, blood urea nitrogen (BUN), serum creatinine, calcium profile, serum lactate, liver function tests, and coagulation studies (PT, PTT, INR). Drug and alcohol screens may be indicated, upon admission, if the circumstances of the accident and/or patient’s clinical presentation warrant it. If inhalation injury is suspected, a serum carboxyhemoglobin, serum cyanide, and arterial blood gas should be obtained, along with a chest X-ray. Laryngoscopy and/or fiberoptic bronchoscopy may also be indicated for inhalation-injured patients. Routine urinalysis, along with urine for hemoglobin and myoglobin in cases in electrical injury, also need to be collected. For patients with pre-existing cardiac disease or those sustaining electrical injuries, a 12-lead electrocardiogram (ECG) should be performed. For patients with suspected, head or spinal injury, fractures or internal trauma, X-rays or scans are indicated. Antibiotic resistant organism (MRSA and VRE) screening and wound swabs for culture and sensitivity (C + S) monitor the microbiological organisms present on admission. Blood cultures, along with urine and sputum for C + S, are helpful when investigating patients who become febrile or who may be developing sepsis. As the patient’s condition changes, medical specialists from various services may be consulted and they may order various diagnostic tests, such as ultrasound, magnetic resonance imaging (MRI), or computerized axial tomography (CAT) scans to rule out or confirm diagnoses. Placement and monitoring of transduced, invasive central and arterial lines provide the team with information on a patient’s cardiac and pulmonary functioning. Access to this wide variety of diagnostic information allows for timely clinical interventions by members of the burn team.
27.7 Possible Complications
Complications can arise throughout all phases of burn care although the potential for development is greater in the acute stage of recovery. Prompt identification and management are essential in order to reach the best possible patient outcome. The systems most commonly affected are cardiovascular, respiratory, gastrointestinal, and renal.
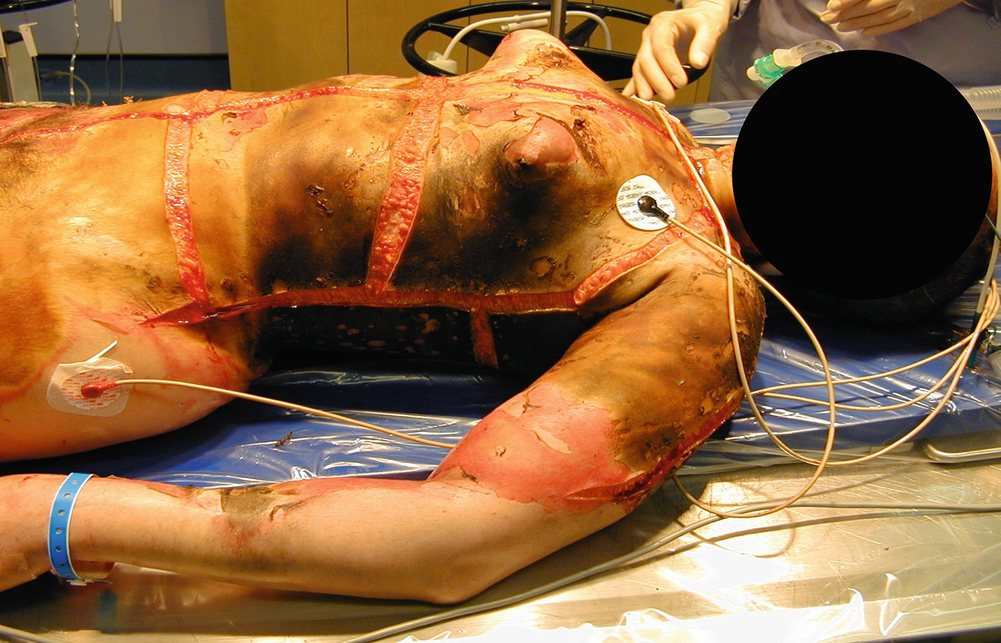
Chest escharotomy
Respiratory system—There are , generally, two ways in which the respiratory system can be affected by a burn injury. One involves mechanical, upper airway obstruction due to heat injury and edema formation and/or constricting circumferential burns to the neck and chest. The other involves inhalation of noxious products of combustion, which produces a chemical irritation reaction to the middle and lower airways. Early in the emergent phase of care, the upper airway can close off very quickly because of massive facial and neck edema. Upon initial assessment, if there is any indication that the patient has a pharyngeal burn, is hoarse or has stridor, the patient should be nasally or, preferably, orally intubated with an uncut endotracheal tube. This action serves to splint the airway open and maintain patency. Arterial blood gases (ABGs) should then be drawn and oxygen saturation levels monitored. If necessary, the patient may need to be mechanically ventilated in order to maintain sufficient levels of oxygenation. Mechanical ventilation protocols should be instituted and ventilator settings titrated to maintain desired PaCO2, PaO2, and SaO2 readings.
When the edema subsides and/or ventilation parameters improve, the patient can be appropriately assessed and extubated safely. In most clinical settings, tracheostomies are performed if the patient is intubated for longer than 3 weeks. Patients, who do not have inhalation injury, may benefit from a face mask or nasal cannula to maintain oxygen saturations >92%. If there are circumferential flame burns to the chest and back, escharotomies of the chest and/or abdomen may need to be performed in order to release the constricting eschar, decrease respiratory distress, and improve chest expansion and ventilation. With an inhalation injury, it is not as obvious that there is damage to the middle or lower airways. At times, patients may present with bronchial and bronchiolar injury, such as bronchorrhea and/or expiratory wheezing. Examination of the lower respiratory tract, using fiberoptic bronchoscopy, should be performed. However, some may have an invisible injury at the level of respiratory gas exchange. This condition is often delayed and diagnosed by arterial blood gas analysis, rather than a chest X-ray. Impaired gas exchange may be related to carbon monoxide poisoning. Carboxyhemoglobin levels should be drawn on admission (Table 27.5). Treatment of inhalation injury includes aggressive chest physiotherapy, tracheobronchial suctioning, administration of nebulized heparin and acetylcysteine, use of bronchodilators (ipratropium) to treat severe bronchospasm, and mechanical ventilation with positive end expiratory pressure (PEEP). PEEP prevents collapse of the alveoli and the development of progressive respiratory failure. If the patient’s condition deteriorates and conventional ventilation strategies prove to be inadequate, newer forms of ventilation have been utilized in recent years and include strategies such as high frequency oscillation and implementation of prone positioning techniques. Patients, who have pre-existing respiratory problems, such as a history of frequent pneumonia or chronic obstructive pulmonary disease, are more likely to succumb to respiratory infection. Pneumonia is commonly seen in these patients since they are relatively immobile, may be debilitated, and have an abundance of microbial organisms that can settle in the lungs and require aggressive therapy to eradicate. Bundled, preventative measures may reduce the risk and incidence of ventilator-associated pneumonia (VAP) [34]. Older, more debilitated patients are also more prone to the development of pulmonary edema as a consequence of the fluid resuscitation required by inhalation-injured patients.
Maintaining the airway is crucial in these patients and frequent assessments of tube placement and stability are an essential part of care. Before patients are extubated, there is a weaning process which involves adjusting ventilator settings, so the machine is doing less of the work associated with breathing and patients are essentially breathing on their own. If they meet certain criteria, patients are extubated, placed in high Fowler’s position, and given 100% oxygen. In addition, they require chest physiotherapy, suctioning, frequent repositioning, and deep breathing and coughing exercises. Mobilization at the bedside and in the hallways is also helpful in moving secretions from the upper and lower airways. Sometimes, patients tire too easily post-extubation and need to be reintubated. In situations where a patient cannot be weaned in the near distant future, a decision is made to perform a tracheostomy until such time as he/she can breathe unaided.
Gastrointestinal system—The gastrointestinal system is initially affected in the emergent phase by a lack of circulation to the splanchnic area. This hypoperfusion, secondary to hypovolemic shock, causes paralytic ileus and an absence of bowel sounds. The stress response post-burn causes a decrease in mucous production and an increase in gastric acid secretion, resulting in stress (Curling’s) ulcers. Prompt and effective fluid resuscitation and a restoration of circulation to the gastrointestinal region result in a return of bowel sounds and indicate a functional gut. Bladder pressures should be measured q4h for 72 h in body surface area burns >30% and pressures >20 mmHg reported. Abdominal compartment syndrome is a life-threatening complication of high-volume fluid resuscitation. Management includes keeping the patient NPO for a few hours post-admission until things stabilize and then, beginning early enteral feeds to address the profound hypermetabolic effects of a burn injury. Anti-catabolic, anabolic agents, such as oxandralone and propanolol, may also prove to valuable adjuncts to therapy. Enteral feeding also maintains the integrity of the gut and avoids bacterial translocation. The hourly rate of feeds is increased, in a timely manner, to the desired goal rate, usually arrived at in consultation with the burn center dietitian. A nasogastric (NG) tube, connected to either straight drainage or wall suction, can be inserted for the purposes of gastric decompression and medication administration. Water flushes pre- and post-medication help ensure the tubes remain patent. Medications include prophylactic use of intravenous H2 antagonists (i.e., ranitidine) to decrease hydrochloride secretion. During the acute phase of care, patients frequently become constipated as a result of codeine-containing pain medication received during their hospitalization and immobility. Prompt institution of a bowel regimen, upon admission, and attention to diet and/or choice of tube feedings can prevent or rectify the situation before it causes the patient unnecessary discomfort. Patients may also develop diarrhea, caused by certain tube feedings or antibiotics. Excessive diarrhea may warrant Clostridium difficile testing. Recommendations from the dietitian or pharmacist should be sought to correct the problem. A bowel management system may need to be inserted if loose stools interfere with optimal wound care. Sepsis is the most common cause of gastric ileus occurring in the acute phase of care and should be monitored closely [35]. Some burn centers are administering an anti-oxidant protocol, which includes selenium, acetylcysteine, ascorbic acid, vitamin E, zinc, and a multivitamin [36]. It is also important to monitor and, if necessary, institute potassium, calcium, magnesium, and phosphate replacements, and administer thiamine and folic acid, particularly if the patient has a history of alcohol abuse. Blood glucose point-of-care testing should be performed and an insulin nomogram commenced, as per ICU protocol, in order to maintain strict glucose control of 80–110 mg/dL [37].
Renal System—With the renal system post-burn, an early warning sign of complications is an increase in the specific gravity, which usually occurs before the urinary output falls. Acute tubular necrosis is the most frequent emergent phase complication and is due to hypovolemic shock. Fluid resuscitation is usually sufficient to correct such problems. Careful attention to trends in urinary output and specific gravity is a more helpful strategy than haphazardly increasing or decreasing the intravenous fluids. Insertion of a urinary catheter should occur, upon admission, to allow for accurate intake/output. If the injury is deep to the tissue and/or muscle, there is the additional complication of high circulating levels of hemoglobin (red blood cell breakdown) or myoglobin (muscle cell breakdown) pigments blocking the renal tubules. This situation is so common in electrical burns that the fluid resuscitation formula requires very aggressive resuscitation and the infusion of an osmotic diuretic (i.e., mannitol). In the acute phase of care, a decrease in urinary output or the development of high output renal failure, with rising levels of BUN and creatinine, may be indicative of a septic episode. Consultation with the renal service is essential if the patient doesn’t respond to fluid challenges or diuretics. In the most serious of situations, the patient may require dialysis as a life-saving measure. Rising glucose levels indicate stress response, due to catecholamine release, and sepsis. High levels lead to compensatory osmotic diuresis, which means the burn patient needs more fluid.
Infection—Burn patients are at risk for the development of infection due to both the high bacterial loads on their devitalized, burn eschar and the loss of their primary barrier against infection—the skin. Infection is the leading cause of morbidity and mortality in burn patients. The degree of risk is increased due to the presence of devitalized burn eschar, which serves as an excellent breeding ground for organisms, invasive catheters and tubes, and a state of immunosuppression that continues long after the wounds have healed. The larger the burn wound, the greater the risk of infection. However, the advent of early burn excision and prompt wound closure has decreased the overall incidence of burn wound infection and, consequently, the incidence of sepsis and death. Evidence-based procedures for the insertion of central lines have resulted in impressive reductions in central line bloodstream infection rates. Ventilator-acquired pneumonia (VAP) rates have also declined since the advent of evidence-based practice bundles, such as chlorhexidine mouth rinse, head-of-bed elevation to 30°, gastrointestinal prophylaxis and turning patients, from side to side, q2h.
The primary sites for organisms are the burn wound, oral and pulmonary secretions, perineal and anal regions. Gram-negative organisms, such as E. coli, Klebsiella, Pseudomonas, and Serratia, are largely responsible for more than 50% of all septic episodes. They release endotoxins, which serve as key triggers for the sepsis cascade. All burn wounds are colonized with bacteria, which can be identified through qualitative wound swabs. More specific determinations can be made using quantitative, burn wound biopsies. If the bacterial count on a wound rises above 1 × 105/g of tissue, the wound is said to be infected, with the organisms having invaded into viable tissue. Local signs of burn wound infection include a change in wound exudate, alteration in wound appearance, increase in wound pain, erythema, edema, cellulitis, and induration at the wound edges. In the presence of a burn wound infection, a partial-thickness wound can convert to a full-thickness wound. If the organisms enter the lymphatic system, the patient can develop septicemia. Sepsis accounts for about 70% of deaths post-burn. Multisystem organ failure, often secondary to sepsis, is a serious and frequently fatal consequence of septicemia. Signs and symptoms of sepsis include an elevated temperature, increased pulse and respiratory rate, and decreased blood pressure and urinary output. The patient may become confused, feel and look unwell, have a diminished appetite and experience chills. It is important to identify and treat the source of sepsis as quickly as possible before multiple organ systems begin to fail. Cultures should be obtained from the blood, urine, sputum, invasive device sites and wounds. Multi-lumen catheters should be inserted in order to provide multiple access ports [38, 39]. Intravenous antibiotics may then be ordered by the burn center physicians, in consultation with the Infectious Disease service in the hospital. Initially, antibiotics can be ordered on speculation, pending culture and sensitivity reports from the lab. If necessary, the antibiotics may be changed to provide coverage specific to the organisms cultured. If the burn wounds, grafted areas or donor sites appear infected, topical antimicrobial coverage on the burn wound may need to be changed or instituted in order to provide treatment at a local level. In general, a patient’s antibiotics can be discontinued when his/her WBC count is normal, when he/she is afebrile and when source control is obtained.
27.8 Clinical Management
27.8.1 Non-surgical Care
Therapeutic management of the burned person is conducted within these same three phases of burn recovery—emergent, acute, and rehabilitative. The emergent phase priorities include airway management, fluid therapy, and initial wound care. The goals of care are initial assessment, management, and stabilization of the patient during the first 48 h post-burn.
Assessment: During the rapid, primary survey, performed soon after admission, the airway and breathing assume top priority. Particularly with a large body surface area burn admission, some staff may feel a tendency to be overwhelmed by the sight and smell of the burn wound. The wounds are, however, a much lower priority than the airway. A compromised airway requires prompt attention and breath sounds verified in each lung field. If circumferential, full-thickness burns are present on the upper trunk and back, ventilation must be closely monitored as breathing might be impaired and releasing escharotomies necessary. The spine must be stabilized until c-spines are cleared. The circulation is assessed by examining skin color, sensation, peripheral pulses, and capillary filling. Circumferential, full-thickness burns to the arms or legs need to be assessed via palpation or Doppler for evidence of adequate circulation. Escharotomies might be required. Typically, burn patients are alert and oriented during the first few hours post-burn. If that is not the case, consideration must be given to associated head injury, (including a complete neurological assessment), substance abuse, hypoxia, or pre-existing medical conditions. All clothing and jewelry need to be removed in order to visualize the entire body and avoid the “tourniquet-like” effect of constricting items left in place as edema increases. Adherent clothing needs to be gently soaked off with normal saline to avoid further trauma and unnecessary pain. Attention then turns to prompt fluid resuscitation to combat the hypovolemic shock. The secondary, head-to-toe survey then rules out any associated injuries. A thorough assessment ensures all medical problems are identified and managed in a timely fashion. Circumstances of the injury should be explored as care can be influenced by the mechanism, duration, and severity of the injury. The patient’s pertinent medical history includes identification of pre-existing disease or associated illness (cardiac or renal disease, diabetes, hypertension), medication/alcohol/drug history, allergies, and tetanus immunization status. A handy mnemonic can be used to remember this information (Box 27.7).
Box 27.7 Secondary Survey Highlights
A—allergies
M—medications
P—previous illness, past medical history
L—last meal or drink
E—events preceding injury

Cart shower for hydrotherapy
Box 27.8 First Aid Management at the Scene
Steps | Action |
|---|---|
Step 1 | Stop the burning process—remove patient from heat source |
Step 2 | Maintain airway—resuscitation measures may be necessary |
Step 3 | Assess for other injuries and check for any bleeding |
Step 4 | Flush chemical burns copiously with cool water |
Step 5 | Flush other burns with cool water to comfort |
Step 6 | Protect wounds from further trauma |
Step 7 | Provide emotional support and have someone remain with patient to explain help is on the way |
Step 8 | Transport the patient as soon as possible to nearby emergency department |
Box 27.9 Treatment of the Severely Burned Patient on Admission
Steps | Action |
|---|---|
Step 1 | Stop the burning process |
Step 2 | Establish and maintain an airway; inspect face and neck for singed nasal hair, soot in the mouth or nose, stridor, or hoarseness |
Step 3 | Administer 100% high flow humidified oxygen by non-rebreather mask. Be prepared to intubate if respiratory distress increases |
Step 4 | Establish intravenous line(s) with large bore cannula(e) and initiate fluid replacement using Lactated Ringer’s solution |
Step 5 | Insert an indwelling urinary catheter |
Step 6 | Insert a nasogastric tube |
Step 7 | Monitor vital signs including level of consciousness and oxygen saturation |
Step 8 | Assess and control pain |
Step 9 | Gently remove clothing and jewelery |
Step 10 | Examine and treat other associated injuries |
Step 11 | Assess extremities for pulses, especially with circumferential burns |
Step 12 | Determine depth and extent of the burn |
Step 13 | Provide initial wound care—cool the burn and cover with large, dry gauze dressings |
Step 14 | Prepare to transport to a burn center as soon as possible |
Airway management includes administration of 100% oxygen if burns are 20% body surface area or greater. Suctioning and ventilatory support may be necessary. If the patient is suspected of having or has an inhalation injury, intubation needs to be performed quickly. Circulatory management includes intravenous infusion of fluid to counteract the effects of hypovolemic shock for adult patients with burns >15% body surface area and children with burns >10% body surface area. Upon admission, two large bore, intravenous catheters should be inserted, preferably into unburned tissue. However, if the only available veins are in a burned area, they should be used. Patients who have large burns, where intravenous access will be necessary for a number of days, benefit from a central venous access device inserted into either the subclavian, jugular, or femoral vein. The overall goal is to establish an access route that will accommodate large volumes of fluid for the first 48 h post-burn. The aim of fluid resuscitation is to maintain vital organ function, while avoiding the complications of inadequate or excessive therapy. Fluid calculations are based on the extent of the burn, the weight and age of the patient, pre-burn conditions (dehydration), or pre-existing chronic illnesses (respiratory, renal). The most commonly used fluid resuscitation regimen is the Parkland (Baxter) formula (Box 27.10). It involves the use of crystalloid (Lactated Ringer’s) solution. Fluids are calculated for the first 24 h post-burn with “0” hours being the time of the burn, not the time of admission to hospital. One-half of the 24 h total needs to be administered over the first 8 h post-burn as this is the period during which extravasation of fluid into the interstitial space is greatest, along with the risk of renal tubule blockage from hemoglobin and myoglobin pigments. The remaining half of the estimated resuscitation volume should be administered over the subsequent 16 h of the first post-burn day. It is important to remember that the formula is only a guideline. The infusion needs to be adjusted based on the patient’s clinical response, which includes vital signs, sensorium, and urinary output. For adults, 30–50 mL urine per hour is the goal and 1 mL/kg/h in children weighing less than 30 kg. An indwelling urinary catheter needs to be inserted at the same time as the IVs are established in order to reliably measure the adequacy of the fluid resuscitation. Vital signs should be trending around a systolic BP of ≥90–100 mgHg, a pulse rate of ≤120 for the older child/adult, <140 bpm in the child between 2 and 5 years of age and <160 bpm in the child under 2 years of age, with respirations at 16–20 breaths/min. The patient’s sensorium should be such that he/she is alert and oriented to time, person, and place. An exception is made regarding the sensorium assessment for the intubated patient. During the second 24 h post-burn, the need for aggressive fluid resuscitation is generally less as capillary permeability begins to return to normal. Colloids, such as albumin, can be given as volume expanders to replace lost protein and minimize ongoing fluid requirements. Earlier administration of colloid would result in leakage out of the vascular space because of the increased capillary permeability. Some patients require extra fluid above and beyond the formula guidelines in order to produce satisfactory urinary output, stabile vital signs, and an adequate sensorium. They include those with (a) high-voltage injury, (b) inhalation injury, (c) delayed resuscitation, or (d) prior dehydration. Those patients with a high-voltage injury require administration of a diuretic to produce a urinary output of 75–100 mL/h in order to clear the tubules of hemoglobin and myoglobin pigments. The usual choice is Mannitol 12.5 g/L of fluid. Since the heme pigments are more soluble in an alkaline medium, sodium bicarbonate can be added to the resuscitation fluid as needed to maintain a slightly alkaline urine. Patients with severe inhalation injury and body surface area burns may require 40–50% more fluid in order to achieve adequate tissue perfusion. The need for extra fluid must be balanced against the risk of pulmonary edema and “fluid creep”/overload. There are others who are considered “volume sensitive.” They are (a) ≥50 years of age, (b) ≤2 years of age, or (c) have pre-existing cardiopulmonary or renal disease. Particular caution must be exercised with these patients.
Box 27.10 Fluid Resuscitation Using the Parkland (Baxter) Formula
Formula | Administration | Example |
|---|---|---|
4 mL Lactated Ringer’s solution per kg body weight per % total body surface area (TBSA) burn = total fluid requirements for the first 24 h post-burn (0 h = time of injury) | ½ total in first 8 h ¼ total in second 8 h ¼ total in third 8 h | For a 65 kg patient with a 40% burn injured at 1000 h: 4 mL × 65 kg × 40% burn = 10,400 mL in first 24 h ½ total in first 8 h (1000–1800 h) = 5200 mL (650 mL/h) ¼ total in second 8 h (1800–0200 h) = 2600 mL (325 mL/h) ¼ total in third 8 h (0200–1000 h) = 2600 mL (325 mL/h) |

Initial wound care post-admission
Objectives of burn wound care
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








