WHO surgical safety checklist
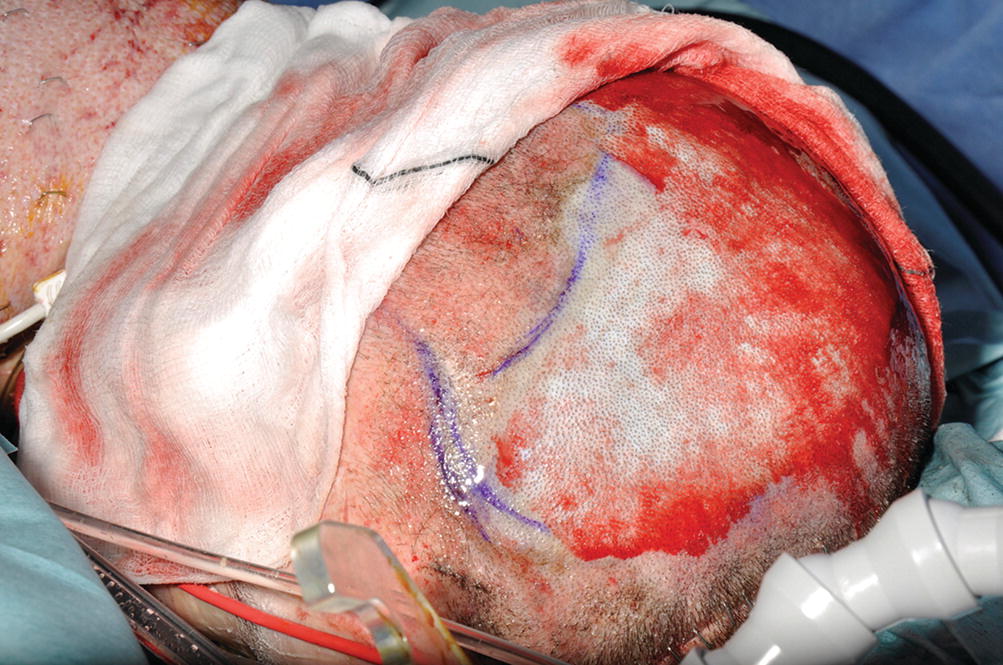
Adrenaline soaks controlling the bleeding of a scalp donor site
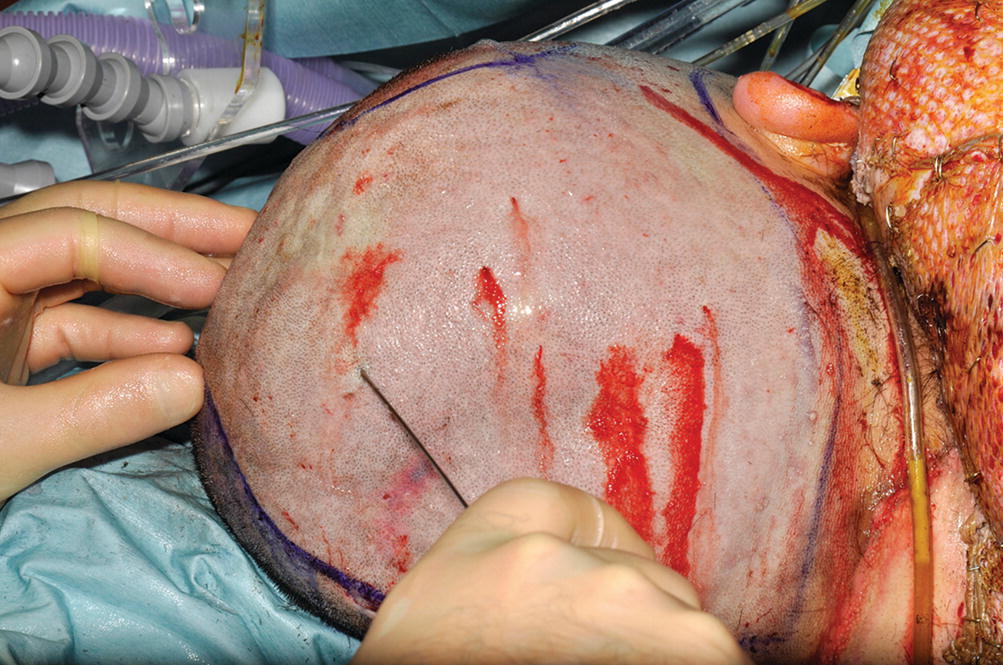
Adrenaline tumescent infiltration of a scalp donor site
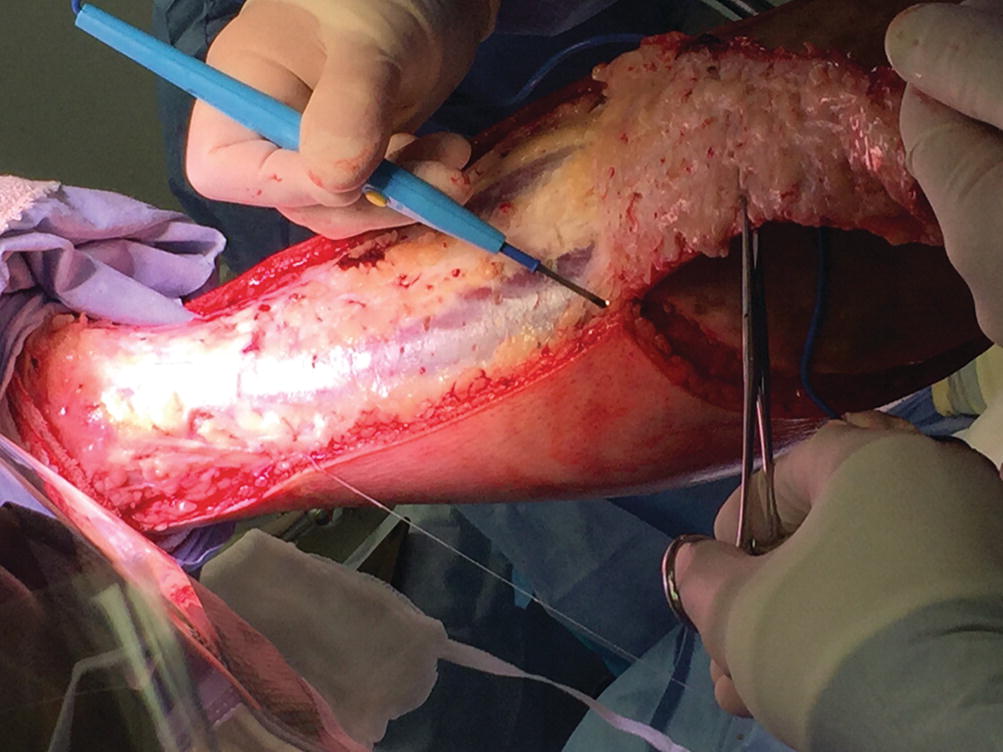
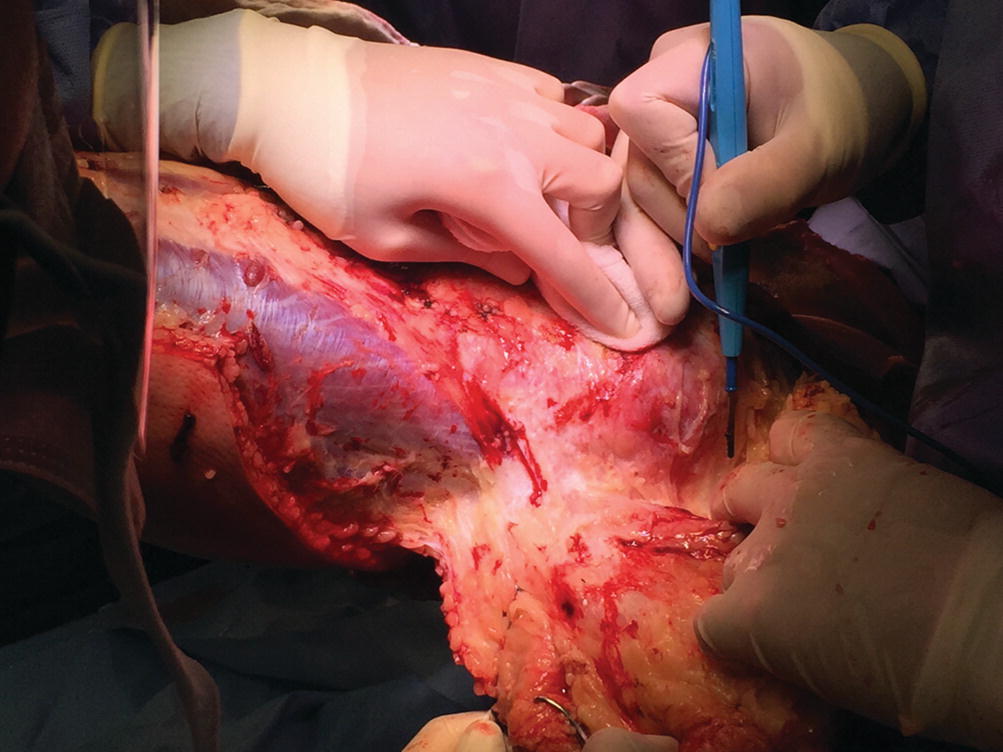
Fascial excision facilitated by hydro dissection with tumescent infiltration
An alternative approach to blood loss control during acute burns surgery is the use of topically applied or device delivered haemostatic agents that accelerate coagulation in tissue surfaces [28]. Fibrin sealants such as Artiss® and Tisseel® (Westlake Village, CA: Baxter Healthcare Corporation) are frequently used in acute burns surgery. These are slow-clotting mixtures of fibrin and prothrombin that act as alternatives to standard methods of graft fixation and donor and recipient site haemostasis. A recent admission to the armamentarium of fibrin sealants is Vivostat® System (Vivolution A/S, Allerod, Denmark). This is an autologous fibrin sealant and platelet rich fibrin (PRF) obtained through mechanical processing of a small sample of blood of the patient. This technique has so far shown promising results in promoting the healing of burn wounds, acting as a support for suspension of keratinocytes and as an enhancer in the successful take of micrografting techniques [29–31].
Sealant techniques can be complemented with systemic therapies such as the use of tranexamic acid. This is an anti-fibrinolytic agent that binds to plasminogen inhibiting breakdown of the fibrin clot. Even though there is limited evidence of its usefulness in acute burns surgery, the experience of its use in trauma suggests a reduction in the requirement for blood transfusion and a positive effect on graft take [32, 33].
34.2.5 Burns Surgery
Once stabilization of the burns patient is complete through prompt first aid, appropriate trauma management with accurate assessment of the burn wound in depth and extent, judicious resuscitation and physiology-protection measures to counterbalance the noxious multisystem effects of the hypermetabolic system, the need to restore anatomy and function becomes a priority. We have pointed out repeatedly how interlinked all these measures are and how their appropriate implementation decreases tissue damage and facilitates the debridement and soft tissue cover by instituting a dermal preservation approach. The practical translation of this approach is straightforward to understand.
Airway management and tracheostomy
Escharotomy
Early burn eschar excision
Wound cover
Urgent, essential and desirable burns reconstruction
34.2.6 Burns Surgery: Airway Management and Tracheostomy
The benefits of performing tracheostomy in burn patients include the ability to perform improved airway toilet and suctioning through a better tolerated and more secure airway, with improvement in the mechanics of ventilation [34]. Following tracheostomy, parameters of the work of breathing such as the airway resistance, peak inspiratory pressures and intrinsic positive end-expiratory pressure decrease facilitating comfort and weaning from mechanical ventilation [35]. Tracheostomy is, nevertheless, an invasive procedure that needs to be performed by experienced individuals either via a percutaneous or through a surgical approach. Clinically, whenever there are neck burns associated with the need for a lengthy period of mechanical ventilation, tracheostomy needs to be considered. To that effect, the burn surgeons perform a preferential debridement of the neck burned skin and resurface it with a sheet of skin graft as soon as possible with the aim of obtaining a healed surface for the tracheostomy site. Even though many studies have failed to show a definitive advantage of early tracheostomy on infection rates, ICU length of stay and hospital length of stay in the intensive care patient cohort [36, 37], burn patients tend to be considered for tracheostomy if there is no possibility of extubating or weaning the patient off the ventilator after 7–10 days of intubation. The options of surgical tracheostomy are reserved for patients with neck burns in which the percutaneous option is not feasible by the bedside, but in this case, the surgical approach is performed after 10 days of autografting of the neck. There does not appear to exist a clear difference in the complication rates for percutaneous vs. surgical tracheostomy [38]
In the paediatric burn population, tracheostomy is a safe method of airway management which appears to be related to the extent of burn injury, not to the age of the patient [39].
The surgical technique follows the steps of standard soft tissue dissection. Nevertheless, the tissue planes may be distorted due to swelling, tissue damage or the body habitus of the patient, which may be subjected to swelling and oedema. A thorough preparation and equipment check warrants lack of complications and a trouble-free insertion of the tracheostomy cannula.
34.2.7 Burns Surgery: Escharotomy
Prior to managing the burn wound with debridement and soft tissue cover, life and limb saving priorities need to be addressed. Unjustified assessment delay may result in catastrophic functional consequences and even death. On performing a structured protocol of assessment of the burn patient, inadequacy of the ventilation and compromise of circulation in the limbs may be ascertained. If circumferential deep burns of full-thickness pattern compromise the compliance of the chest and abdomen or the perfusion and viability of the distal perfusion of the limbs, the need for escharotomy needs to be considered. The consequences of not addressing these surgical alarms promptly, appropriately and by the most senior and experienced clinician, affect directly the viability of the soft tissues injured by the thermal injury and may have far-reaching fatal consequences.
When tissues are burned, the depth to which they do so depends on the intensity of the thermal injury. Deep injuries will not only damage the anatomical integrity of the skin, reducing its pliability and elasticity, but will also reduce the blood supply to its dermal component, making healing and self-regeneration unlikely. The clinical consequences of this scenario are a shift towards a deep pattern of injury and a migration towards tissue necrosis from the potentially salvageable zone of stasis. The resulting damage leaves the skin as a leathery, non-pliable structure that behaves as a tight restrain for deeper fascial layers, neurovascular bundles and muscular compartments. This alarming scenario will worsen when fluid shifts favoured by increased capillary permeability migrate towards the extracellular space. The tissue already damaged and hypoperfused will sustain further insult, potentially leading to interstitial oedema pain, hypoperfusion, vascular ischemia and hemodynamic and vascular compromise. Facing these concerns, not only escharotomies but also a full array of decompression strategies needs to be considered for chest, abdomen and limbs [40, 41]
Perform under general anaesthesia, in a warm theatre, with full resources including back up of blood products.
Use monopolar diathermy in cutting mode to perform initial incision from unburned skin to unburned skin. Do not advance in your incision unless you have full control of any bleeding points.
Check with fingertip full release of the eschar down to subcutaneous tissue.
Make a second pass along any tight unreleased areas by changing the mode of the diathermy to coagulation.
In the case of extremities, the upper limbs need to be placed in the anatomical position, with the forearm supinated and palms facing up. The natural tendency of the oedematous burned upper limbs is to go into a pronation position. Failure to supinate the forearm will lead to potential misplacement of the escharotomy incisions in the antecubital fossa.
Perform the escharotomies in upper and lower limbs along axial lines respecting anatomical structures of importance such as ulnar nerve in the upper limbs and (Fig. 34.5) the long saphenous vein and distal neurovascular bundles of the lower limb
Perform chest escharotomy in response to poor ventilation compliance, anaesthetic concerns and high peak ventilation pressures along anterior axillary lines joining the incisions along costal margin and clavicle if necessary.
Perform abdominal skin escharotomy to treat full-thickness burn of the abdominal wall but be ready to proceed to abdominal decompressing laparotomy, exploration and release together with general surgeons if abdominal compartment syndrome is suspected.
Success of abdominal release for abdominal compartment syndrome will improve parameters of intraabdominal hypertension, respiratory function, hypoperfusion and acidosis [43, 44].

Escharotomy of upper limbs
Complications of inadequate decompression escharotomy will lead to compartment syndrome muscle damage, neurovascular injury and potential amputation of the limb. Systemic complications include myoglobinuria, renal failure, metabolic acidosis and even death.
Burns surgeons recognize and accept that there is potential morbidity caused by escharotomy release. Nevertheless, certain mistakes should be avoided. Inadequate length or depth of the incisions will lead to unnecessary damage of underlying functional deep structures. Accurate assessment of the damaged tissue will stop unnecessary performing the procedure on likely-to heal skin and avoid complications such as unnecessary bleeding, infection and abnormal scarring.
The resulting escharotomy wounds are initially packed with a paraffin-impregnated dressing and loosely bandaged. They are eventually closed primarily once the tension of the tissues has subsided or split skin grafted.

Fasciotomy of the upper limb
34.2.8 Burns Surgery: Wound Excision
Wound excision starts once the preparations for surgery have been completed and the optimization of the patient is appropriate. The operative team, with an experienced team of 4–6 surgeons supported by 2 anaesthetists, 2 scrub team members, intensivists and nursing team will work in a self-contained and fully staffed operating theatre with efficient climate control, and ready access to blood, fresh frozen plasma and allograft from a skin bank. They will have the backup of a full intensive care facility for ventilation and hemofiltration and on-site paediatricians, geriatricians, psychiatrists, dieticians, pharmacists, bacteriologists, haematologists and biochemists.
The excision techniques will be tailored to the depth and extent of the burn, but also to the ability of the patient due to age, physiology and comorbidities to withstand the trauma of the surgery, together with blood loss, hypothermia, acidosis and cardiorespiratory depression.
The excision techniques can be classified into sharp, hydro surgical and enzymatic. Sharp techniques can be subdivided into tangential and fascial.
A recent study designed to assess burn surgeons’ preferences in excision and grafting to determine if surgical technique affects outcomes showed that clinical judgment is still the most likely method of assessment for excision. More than half of the surgeons perform excision as early as postburn day 1 and a clear majority of the surgeons surveyed would perform more than 20% TBSA in a single operation [45].

Tangential excision
Fascial excision
Hydro surgical techniques introduce an interesting element of addition to the armamentarium of the burns surgeon. The Versajet™ Hydro surgery System (Smith and Nephew Medical Ltd., Memphis TN, USA) is a debriding tool based on the Venturi effect that excises and removes necrotic tissue by emitting a pressurized saline stream acting like a scalpel. The debrided tissue is aspirated at high pressure into a cannister.
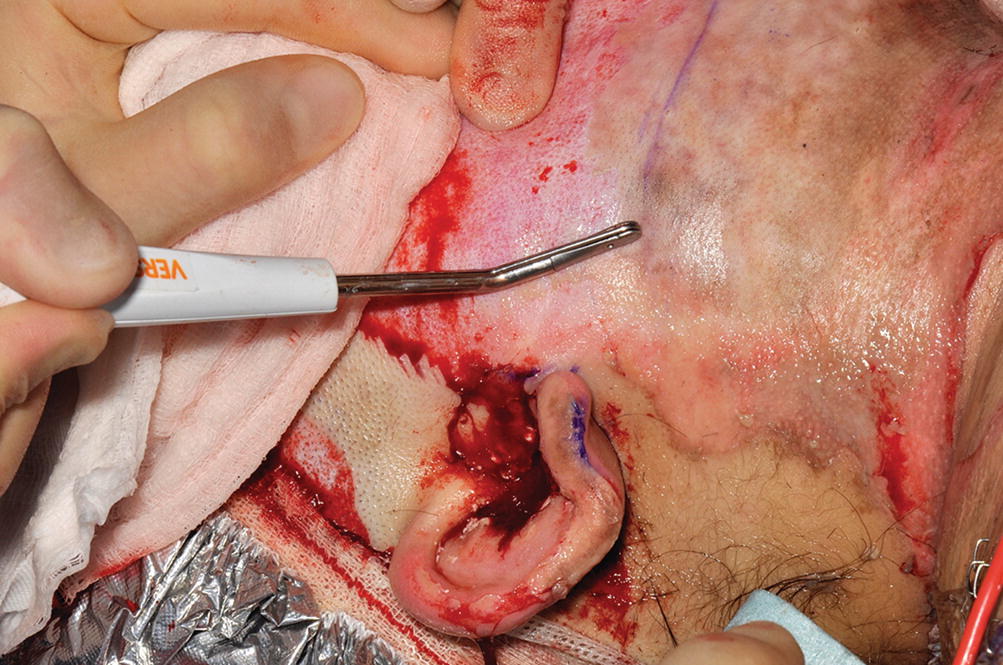
Versajet debridement of the face
Enzymatic debridement represents an extra innovative debriding tool for deep burn injuries. It is important to state from the beginning that this Bromelain-based substance is not a substitute to skin grafting or soft tissue cover, as self-regeneration and healing will only occur if enough viable dermis remains in the wound after the process of application, removal and dressing care. The process for preparation and application is straightforward and involves a cleaning of all non-viable skin debris, a wet pre-soak of the wounds with saline and chlorhexidine of several hours, application of the product (Nexobrid®, Mediwound, Israel) for 4 h after appropriate analgesia, removal of the debris of the wound and the product and overnight post procedure soak of the area with saline. It is reported in several trials that this debriding option is a powerful tool to remove eschar in burn wounds, reducing blood loss, the need for autologous skin grafting and the number of wounds requiring surgical excision [53]. A recent European consensus established guidance over application guidance, timing of the procedure, blood loss, analgesia and dressing care [54]. A myriad of papers has been produced on this technique, expanding the indications for its usage and anatomical areas that can be treated [55, 56].
34.2.9 Burns Surgery: Wound Cover
Tissue cover is not the final step of burn care, but if successful, it is the first landmark towards definitive recovery, as it allows the patient to seal the wound, decrease infection and restore, even in a limited way, physical integrity and facilitate the pathway towards rehabilitation, recovery and social reintegration. The coverage of wounds nevertheless comes at the expense to create donor sites and new wounds, that are submitted, until healing to a potentially lengthy period of dressing changes supported by infection surveillance, nutrition and physical and emotional therapies. There will be situations in which due to the wound environment, the TBSA involved or the age, physiology or comorbidities of the patient, it will not be possible (the deep extensive wound) or necessary (the superficial extensive wound) to cover the wound immediately or in a single operation, and a staged temporizing approach with dressings, allograft or dermal replacements will be necessary.
When the wound is ready for definitive cover, skin grafts in variable regimes of meshing, supported or not by allograft or skin replacement materials, cell suspension techniques or flaps get the wound sealed and healed and represent the final process in anatomical and functional restitution.
34.2.10 Temporizing Options
The concept of burn wound temporizing cover involves two types of wounds, partial thickness with healing potential or deeper wounds requiring debridement that may need a period of alternative alloplastic cover before definitive autologous grafting.
The temporizing options for wound management can be synthetic (Biobrane®, Suprathel®, dressings, etc.) or biological (Allograft, Xenograft).
In the case of partial-thickness wounds with healing potential, the patient is taken to theatre for gentle debridement and assessment of the viability of the dermis. The wound will then be treated with a temporary layer of alloplastic material to ensure dermal protection, avoid desiccation and promote epithelialization.
In these cases, there is usually no need for sharp debridement and the wound is usually debrided with hydro surgical methods (Versajet®) and covered with either xenograft [52], or specialized dressing material such as Biobrane® (Smith and Nephew, UK) [57, 58], Suprathel® [59, 60] (PolyMedics Innovations, Germany), or dressings. The debridement with the hydro surgery tool is carried at low power in order to get a fine punctate bleeding indicative of dermal viability. The resulting fibrin layer from the clots acts as a gentle adhesive for these skin substitute materials.
The combination of hydro surgery and alloplastic cover is especially useful as a temporizing option due to the ability of Versajet® to debride soft eschars very efficiently even in anatomically sensitive areas like hands and faces. Biobrane®, a transparent, temporary wound cover familiar to the burn surgeon, promotes epithelialization due to its combination of nylon mesh and porcine collagen in partial-thickness burns, and it is easy to use and handle both in adults and paediatric patients.
Suprathel® is produced from a synthetic copolymer mainly based on dl-lactide (>70%), trimethylenecarbonate and ε-caprolactone. The material is presented as a desiccated thin layer which tends to become gently elastic with heat and that adheres well to the wound. It has significantly shown to reduce pain, it is easy to handle, comfortable for the patient and comparable to Biobrane® in indications and results.
In cases of burn wounds that require temporizing before autograft due to their deep pattern of injury, wound environment or to the paucity of donor sites, allograft [61] remains the main option for temporary cover. Allograft is usually obtained from tissue banks either as glycerol preserved or in freeze-dried sheet or pre-meshed packets. They need to be washed out and thawed and appropriately meshed (if not done so before) and then applied to the wound bed to temporize either as a watchful waiting option to prime the tissues for healing or to prepare the wound bed for autografting.
Healthy bleeding from the wound helps in the adhesion of the allograft sheets, which are regularly inspected for infection, hematomas, seromas, shearing or detachment. Allograft options reduce the possibility of fluid loss and act as indirect markers of the potential for autografting, as it already possesses many of the desirable properties of autologous skin. Following adhesion and neovascularization, the graft will characteristically exhibit rejection of its cellular elements and will eventually need to be changed or substituted by autografting [62, 63].
34.2.11 Definitive Soft Tissue Cover
The aim of permanent skin cover following debridement of the burn wound is to restore as much as possible the integrity of the damaged burn skin with tissue options that provide prompt healing, pliability, elasticity and a recovery of all skin functions. The reality is that this aspirational wish of the burn surgeon is met with cover strategies that may be limited in their quantities or anatomical integrity. Autologous donor skin will be limited if the burn is extensive. Even the provision of skin grafts represents the substitution of the full thickness of the skin for a thin layer of epidermis and papillary dermis that will obviously contract and scar to the point of limiting function. Definitive cover may need to be preceded, as detailed above, by a period of wound temporizing. The options for permanent cover reside then in manipulating the available donor skin and make it wider and larger by different meshing regimes, culture it to provide cover in situations of donor site paucity or a large burn or make it resemble as much as possible as the uninjured skin by combining it with a skin replacement or dermal template.
Full-thickness grafts contain all skin layers and constitute the best attempt to provide pliability, elasticity, colour and texture match in the reconstructed site, Unfortunately, their harvesting leaves a defect that needs to be closed primarily and the donor site areas may be limited (groin, supraclavicular, pre- and postauricular areas, flanks, abdomen). Their use is characteristically limited to cover anatomically sensitive areas like the face and the hands [64, 65].


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








