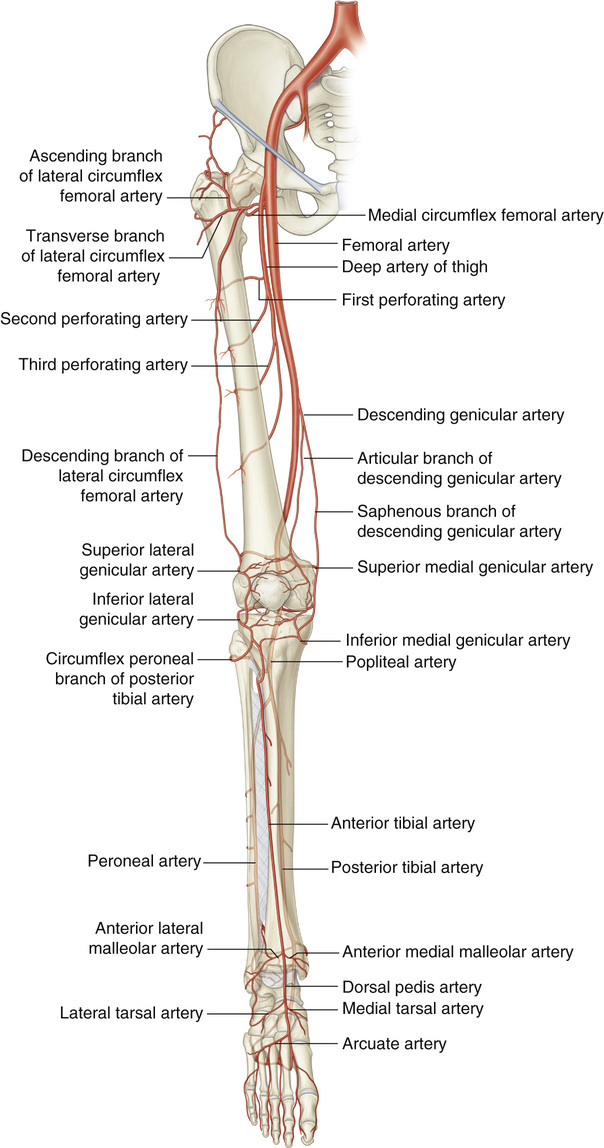
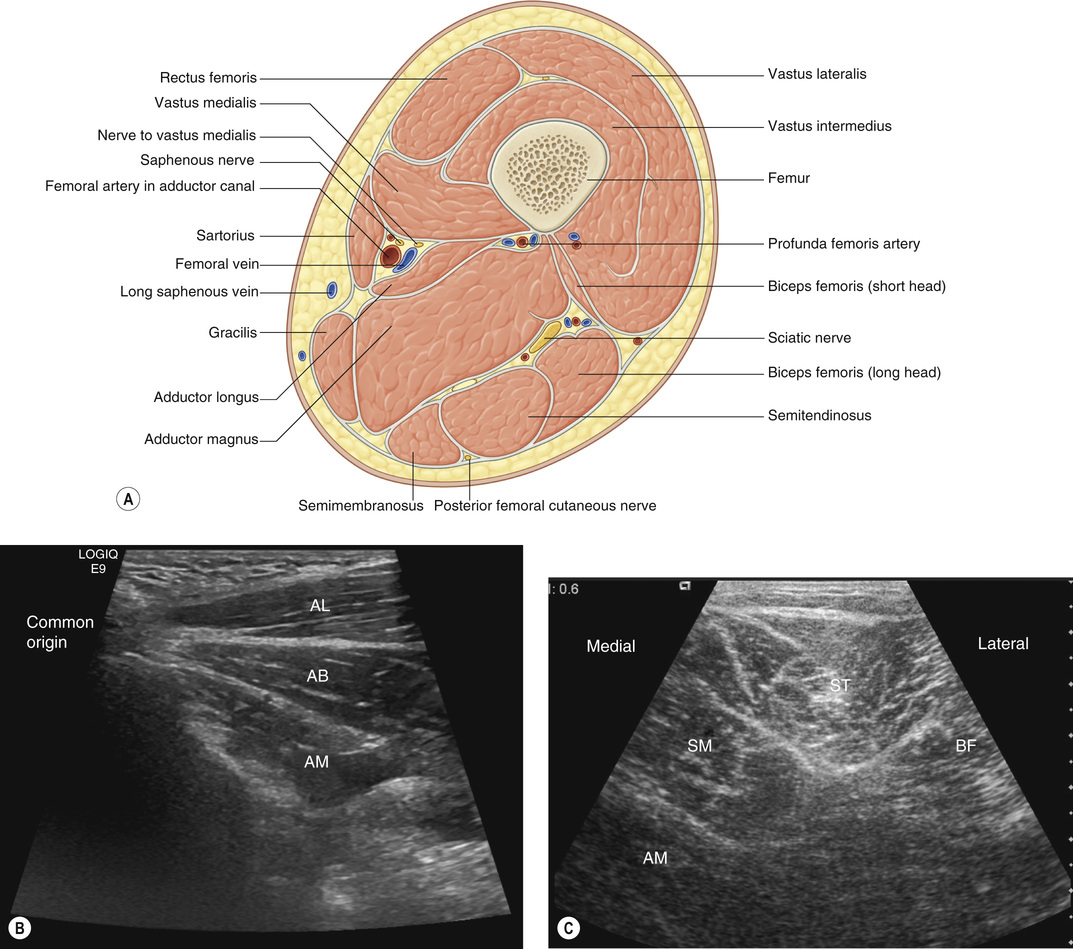
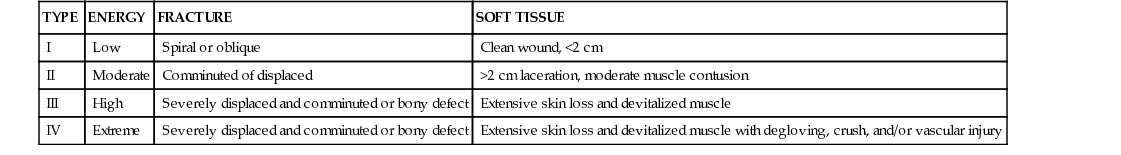
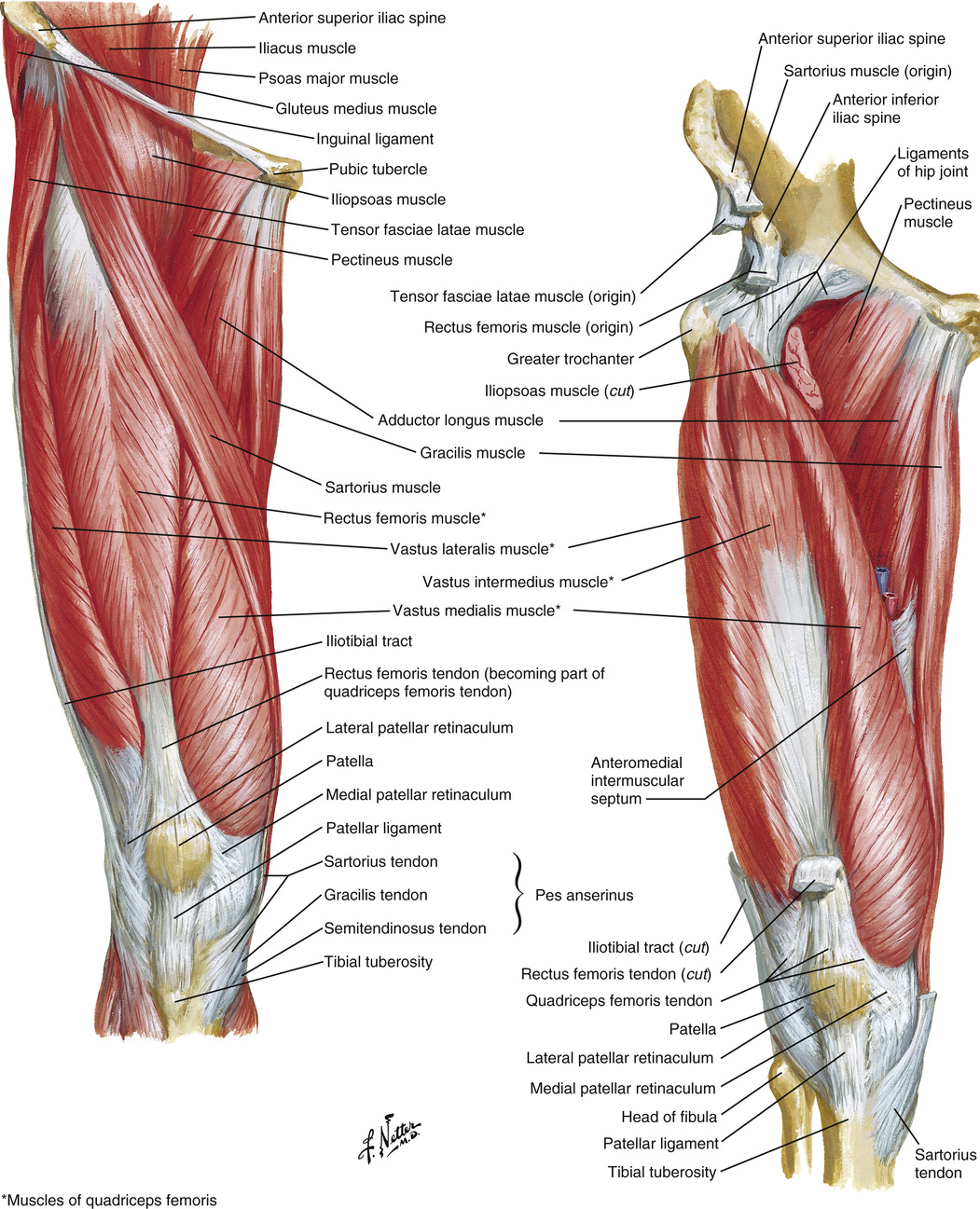
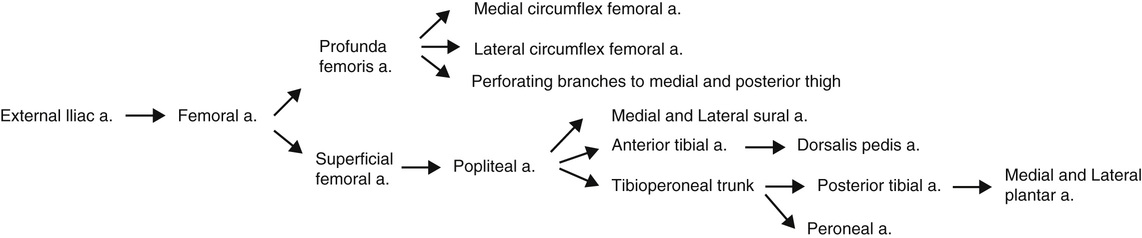
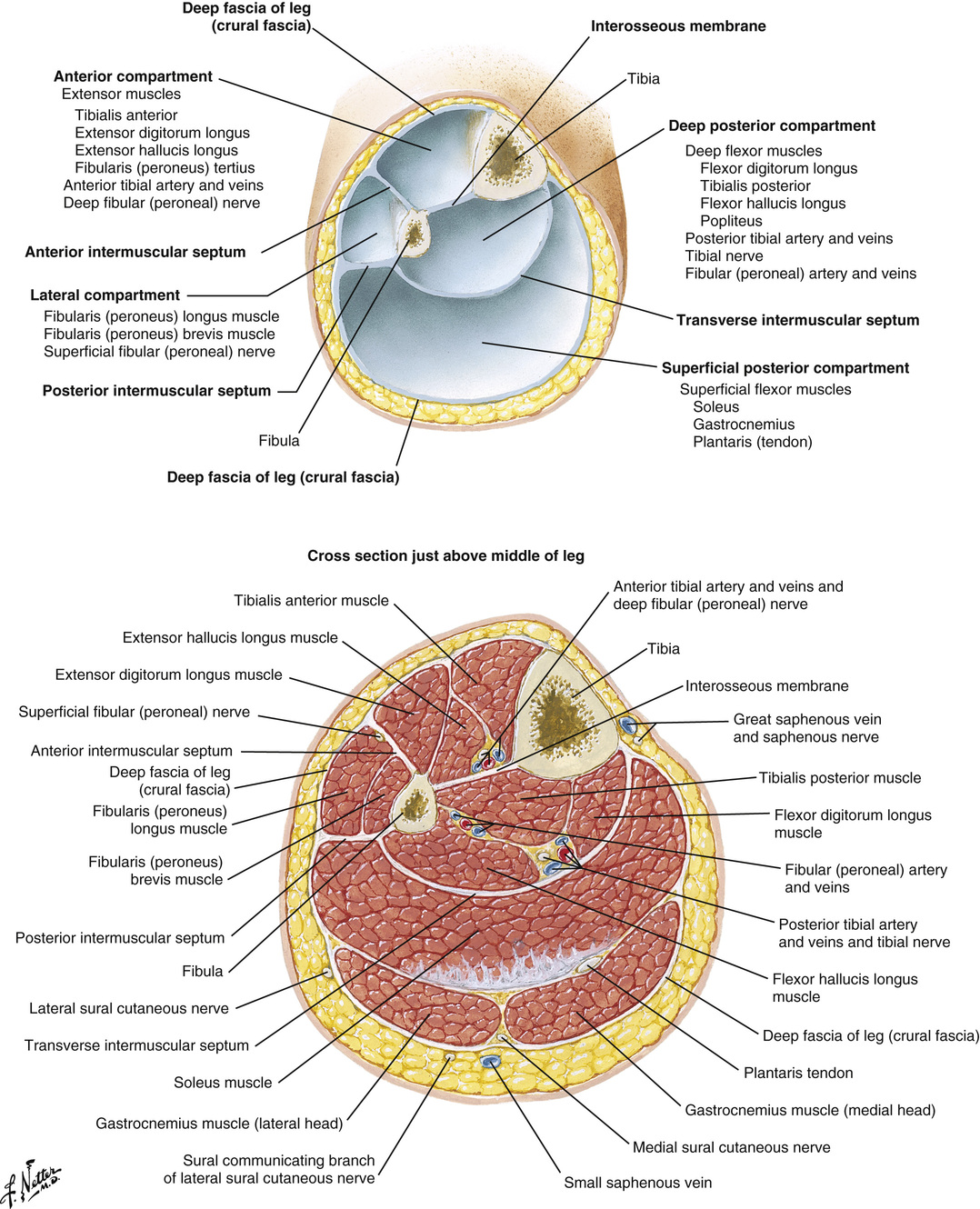
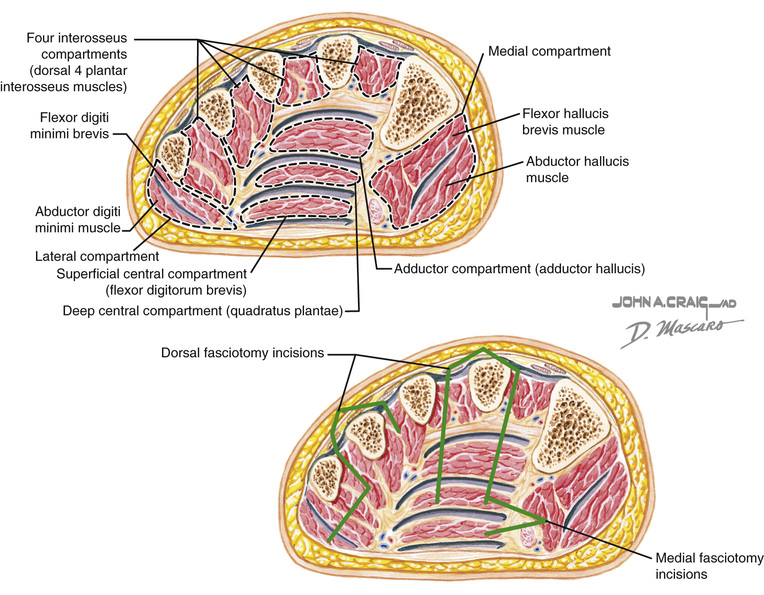
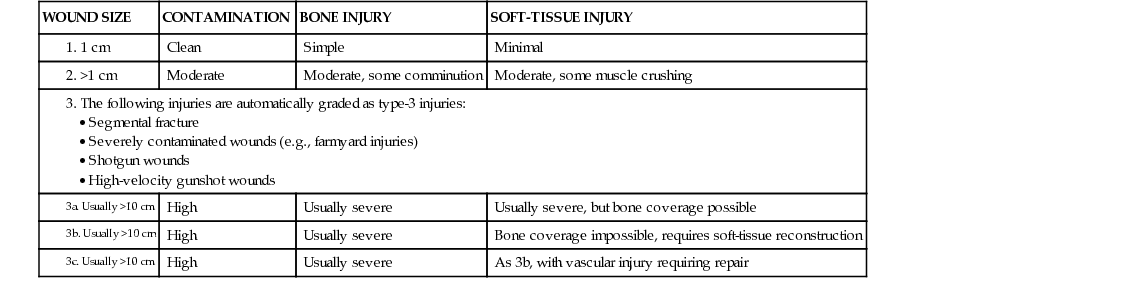
1. General lower extremity (LE) anatomy • Vascular supply (see Figures 13.1 and 13.2) ▪ Thigh ○ Anterior ♦ Sartorius m., rectus femoris m., vastus lateralis m., vastus intermedius m., vastus medialis m. ♦ Biceps femoris m., semitendinosus m., semimembranosus m. ○ Medial ♦ Gracilis m., adductor longus m., adductor brevis m., adductor magnus m. ♦ Obturator n. (see Figure 13.3) ○ Anterior ♦ Tibialis anterior m., extensor hallucis longus m., extensor digitorum longus m., peroneus tertius m. ○ Lateral ♦ Peroneus longus m., peroneus brevis m. ♦ Tibialis posterior m., flexor hallucis longus m., flexor digitorum longus m., popliteus m. ♦ Gastrocnemius m., plantaris m., soleus m. ▪ Foot ○ Medial ♦ Abductor hallucis m., flexor hallucis brevis m. ○ Lateral ♦ Abductor digiti minimi m., flexor digiti minimi brevis m. ♦ Flexor digitorum brevis m., quadratus plantae m., adductor hallucis m. (see Figure 13.5) 2. LE trauma ○ Description based on degree of soft-tissue injury and presence of vascular injury ○ Major vascular injury requiring repair is automatically a class IIIC. ○ Classes I and II can generally be managed with local wound care. ○ Class III generally requires flap coverage. ♦ Classes A, B, and C distinguished according to size of wound and presence of vascular injury ➔ A: Wound <10 cm, soft-tissue coverage is usually possible ➔ B: Wound >10 cm, regional or free flap needed ➔ C: Presence of major vascular injury requiring repair for limb salvage ♦ IIIB/C: Often requires initial stabilization with external fixator (see Table 13.1) Table 13.1 Classification of Open Fractures 1. 1 cm 2. >1 cm 3. The following injuries are automatically graded as type-3 injuries: • Severely contaminated wounds (e.g., farmyard injuries) 3a. Usually >10 cm 3b. Usually >10 cm 3c. Usually >10 cm ○ Established based on force of injury and degree of bony comminution ♦ Type I: Low-energy, spiral, or oblique fracture with clean wound <2 cm ♦ Type IV: Extreme energy, same as class C with degloving or crush injury and/or vascular injury (see Table 13.2) ▪ Computed tomography (CT) angiography provides the most rapid method for evaluating LE vasculature. ▪ Free flaps are often required for large defects because of paucity of available local tissue (IIIB/C). • Reconstruction versus amputation ▪ Goal: Preserve a limb that will be more functional than an amputation ○ If the extremity cannot be salvaged, the goal is to maintain the maximum functional length. ♦ Minimum of 6 cm is required for adequate prosthetic fitting of below-knee amputation. ▪ Absolute contraindications for reconstruction • Vascularized bone flaps versus allogeneic bone grafts ○ Demonstrate increased osteocyte viability ○ Osteogenesis through osteoinduction versus depending solely on creeping substitution (allogeneic) ○ Indicated for bony defects >6 cm ▪ Increased pressure in a confined space ➔ Pain out of proportion (often first sign) ➔ Pallor 3. Commonly used LE flaps (see Figure 13.6) ▪ Origin: Anterior superior iliac spine ▪ Insertion: Anteromedial surface of tibia ▪ Function: Flex, laterally rotate, and abduct hip; weak knee flexor ▪ Arterial supply: Superficial femoral a. provides segmental blood supply (type-IV muscle). ▪ Function: Flex, medially rotate, and adduct hip; weak knee flexor ▪ Arterial supply: Medial circumflex femoral a. • Anterolateral thigh myocutaneous or perforator flap ▪ Arterial supply: Descending branch of lateral circumflex femoral a. ▪ Nerve: Lateral femoral cutaneous n. ▪ Underlying muscle: Vastus lateralis m. ▪ Origin: Femoral condyles (medial and lateral) ▪ Insertion: Calcaneus through achilles tendon ▪ Function: Plantarflexion; knee flexion ▪ Arterial supply: Sural arteries (medial and lateral) ▪ Medial muscle: Indicated for medial upper leg 1/3 defects, longer than lateral gastrocnemius, and does not risk damage to the peroneal nerve (see Figure 13.7) ▪ Origin: Fibula, medial border of tibia ▪ Insertion: Calcaneus through achilles tendon ▪ Arterial supply: Peroneal artery ▪ Often used for bony defect reconstruction ▪ Arterial supply: Medial plantar artery ▪ Nerve: Medial plantar n. (L4 to 5) ▪ Most reliable sensate flap with glabrous skin for coverage of the plantar calcaneus • First dorsal metatarsal artery (FDMA) flap ▪ Arterial supply: FDMA from dorsalis pedis a.
Lower Extremity Reconstruction and Lymphedema
WOUND SIZE
CONTAMINATION
BONE INJURY
SOFT-TISSUE INJURY
Clean
Simple
Minimal
Moderate
Moderate, some comminution
Moderate, some muscle crushing
High
Usually severe
Usually severe, but bone coverage possible
High
Usually severe
Bone coverage impossible, requires soft-tissue reconstruction
High
Usually severe
As 3b, with vascular injury requiring repair
![]() Compartment pressure >30 mm Hg
Compartment pressure >30 mm Hg
Lower Extremity Reconstruction and Lymphedema
Chapter 13