Lower Body Lift and Thighplasty
Joseph P. Hunstad
Remus Repta
LOWER BODY LIFTS
Key Points
The lower body lift is recommended for patients with circumferential body laxity who have achieved significant weight loss through surgical bariatric intervention or diet and exercise regimens (see Chapter 66). The procedure is performed in both prone and supine positions requiring patient repositioning intraoperatively. The circumferential component of the procedure allows for the treatment of buttocks ptosis, lateral and anterior thigh laxity, abdominal tissue redundancy, as well as mons ptosis. The lower body lift procedure can be combined with various ancillary procedures such as autologous buttocks augmentation, fleur-de-lis abdominal contouring, thigh lift, and mons reduction. There is overlap between this chapter and Chapter 66 on abdominoplasty. We encourage the reader to study both chapters.
INTRODUCTION
The lower body lift serves as the “keystone” procedure upon which all subsequent body contouring procedures are based.1,2,3 It is important for patients to understand that there is no exercise for skin! This is frustrating for patients who exercise regularly but have skin laxity of the trunk secondary to genetics. The lower body lift procedure is far more than a “belt lipectomy” where circumferential excess skin is removed from the midwaist area of the trunk (Chapter 66). By placing the resection lower, near the trunk-lower body junction, more powerful lifting of the buttocks and thighs is accomplished. Circumferential resection allows for maximum tissue resection without concern for dog-ears. Ancillary procedures including vertical thighplasty, mons resection, and autologous buttock augmentation can be included.
Patient Selection
Patients who present in consultation for a lower body lift usually seek improvement primarily in the appearance of the abdomen and buttocks. Patients must be educated regarding the resulting scar and should be at or near their goal weight. It is necessary that the patient be well informed and compliant. This is a big operation and cooperation in the postoperative period can impact the risk of complications, such as deep vein thrombosis (DVT), and the final result.
Indications
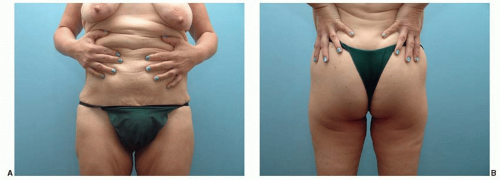
During consultation, patients frequently demonstrate their desired surgical outcome by lifting the excessive tissue laxity of the lower abdomen, buttocks, and thighs (Figure 67.1). Massive weight loss patients who have reached a normal BMI (they do not require additional liposuction) and normal weight individuals are the ideal candidates for this procedure.
Contraindications
Relative contraindications for lower body lift surgery include smoking, diabetes, malnutrition, wound healing issues, and immunodeficiency. The use of anticoagulant medications, lower extremity venous insufficiency, lymphedema, a previous history of venous thromboembolism (VTE), and other medical issues such as renal insufficiency, anemia, and pulmonary issues may also be prohibitive. Patients who have a significant amount of excess fat and only a mild or moderate amount of skin laxity should be educated regarding the benefit of weight loss through diet and exercise or through bariatric surgery. The lower body lift is ideally suited to correct skin and softtissue laxity and not as a fat reduction procedure.
Preoperative History and Preparation
Patients who have achieved massive weight loss may be malnourished and/or suffer from other metabolic abnormalities.4 Laboratory blood work including complete blood count, basic metabolic panel, coagulation profile, pregnancy test, and total protein/albumin levels is recommended. Abnormal laboratory values warrant additional nutritional analysis and intervention to avoid postoperative wound healing problems. A history is obtained regarding VTE (Chapter 11). A factor V Leiden analysis can be performed to rule out this unusual form of coagulopathy. Hormone replacement therapy and birth control medications are discontinued for several weeks prior to surgery if possible. Patients are encouraged to stop smoking for 6 weeks before surgery and not to resume until 3 weeks post-op. Sequential compression devices are used on the lower extremities throughout the surgical procedure and until discharge. The use of proper intraoperative positioning with the knees partially flexed, perioperative prophylactic medication such as Lovenox, and early postoperative ambulation are also employed.5
Existing abdominal scars are evaluated since they can adversely impact the blood supply to the abdominal apron.1 A lower body lift procedure usually eliminates the inferior and central blood supply to the abdominal soft tissue, basing the remaining vascular supply on the intercostal perforators (Chapter 66). Preexisting scars can also impact the final aesthetic result of the lower body lift procedure if they cannot be included in the resection. The presence of scars may alter the tissue pliability in that region and the surgical markings should take this into consideration.
Operative Approach
Preoperative photographs are obtained. Existing scars are marked and included, whenever possible, in the proposed skin resection. When the patient desires the final incision within the boundary of a specific undergarment or swimwear, we mark the outline of the garment and position the incision accordingly. With the patient lifting the abdominal skin superiorly, the lower transverse mark is made at the level of the pubic symphysis (Figure 67.2). The patient then releases the abdominal soft tissue and the incision is lengthened laterally to the level of the iliac crest following a natural skinfold. The desired final location of the posterior incision is marked along the upper portion of the buttocks (Figure 67.3A). If autologous buttocks augmentation is anticipated, the final incision line over the buttocks should be a continuation of a line from the pubic symphysis to the greater trochanter and extended to the posterior midline (Figure 67.3B). This line will indicate the area of maximum projection of the buttocks.1,6 Starting in the midaxillary line with the patient bent slightly away from the surgeon to prevent over-resection the extent of the resection is estimated bilaterally (Figure 67.4A). The posterior resection is marked, noting that the amount of resection is conservative
in the midline because of the strong zone of adherence and reduced laxity. When autologous buttocks augmentation is planned, the amount of resection of the posterior segment is reduced to accommodate the volume that will be added. From the upper marking in the midaxillary line a dotted line is continued anteriorly across the abdomen, representing the estimated amount of resection. The exact amount of the resection will be determined intraoperatively (Figure 67.3A). Areas for concurrent liposuction are then marked as well.
in the midline because of the strong zone of adherence and reduced laxity. When autologous buttocks augmentation is planned, the amount of resection of the posterior segment is reduced to accommodate the volume that will be added. From the upper marking in the midaxillary line a dotted line is continued anteriorly across the abdomen, representing the estimated amount of resection. The exact amount of the resection will be determined intraoperatively (Figure 67.3A). Areas for concurrent liposuction are then marked as well.
A V-Y mark is made within the planned resection amount at the midaxillary line which will allow temporary closure of this area when the patient is repositioned from prone to supine (Figure 67.4B). For patients with significant transverse as well as vertical tissue laxity, a concurrent vertical resection, commonly referred to as a fleur-de-lis resection can be utilized (Figure 67.5). Most massive weight loss patients are willing to accept a vertical midline scar in return for correction of laxity.1 The final shape of the fleur-de-lis resection should be closer to an ellipse than a triangle, to prevent excessive tension at the junction of the vertical and horizontal closure (Figure 67.5). All markings are rechecked to ensure symmetry and to avoid over-resection.
General anesthesia is initiated, antibiotics and steroids are given (Ancef 1 g and Decadron 4 mg), and a Foley catheter is inserted. When concurrent liposuction is planned, thorough tumescent infiltration of all areas to be suctioned is performed.
The patient is carefully rolled in the prone position on the operating room table that has been arranged with padded chest rolls, kneepads, and a roll or pillow beneath the ankles.
The patient is surgically prepped and draped taking care to include the most anterior point of the planned V-Y closure in the midaxillary line bilaterally.
Once prepped and draped, the markings are checked for tension and symmetry. The posterior resection is performed without undermining, forming a “V”-shaped resection. This inward beveling allows closure to occur without dead space. When autologous buttocks augmentation is performed, the intervening tissue between the upper and lower incisions is deepithelialized. This flap of tissue can be molded with suture in a purse-string method or partially elevated and rotated as a flap.4,7,8
Laterally, the resection continues to the midaxillary line where the temporary V-Y resection and closure is performed (Figure 67.6). Undermining is suggested at this point over the trochanter to release the retaining elements in this area of adherence. The posterior drain is placed and the end is coiled and inserted beneath the skin of the V-Y closure to be brought out anteriorly when the patient is turned supine. Hemostasis is obtained and a three-layer closure is performed. The most important layer of the closure, the superficial fascia, is closed with either a number 1 or 0 Vicryl or equivalent suture. Repair of the superficial fascial layer is performed under tension. Doing so allows the dermis to be approximated under minimal tension which increases the chance of obtaining a thin, inconspicuous scar. Size 2-0 or 3-0 Vicryl or equivalent suture is used in an interrupted buried fashion to approximate the dermis at each vertical oriented/tattoo mark and then at approximately 1 cm intervals. Finally, a running intradermal number 4-0 Monocryl or equivalent suture is used to approximate the skin edges. The patient is carefully repositioned into the supine position. Foam rolls are placed beneath the knees and the heels are padded. The arms are abducted and placed on padded arm boards. Warm air blankets are placed over the lower extremities. A standard surgical prep and drape of the anterior body surface is performed. When indicated, liposuction is performed throughout the areas that were previously infiltrated.
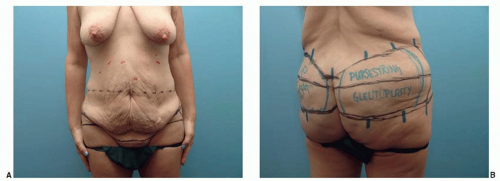 FIGURE 67.3. Lower body lift markings (A and B). Preoperative markings are demonstrated with the patient relaxed. A. Note how low the anterior incision is in the midline, removing a significant portion of the hypertrophied mons. B. Realignment marks are added. In this case, a buttocks augmentation using a purse-string gluteoplasty will be performed and the markings for this are evident.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|