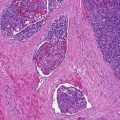
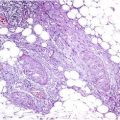
Fig. 29.1
Low-grade fibromyxoid sarcoma. Histological appearance with spindle and stellate-shaped cells, in a whorled or linear arrangement, and with collagenized and myxoid areas
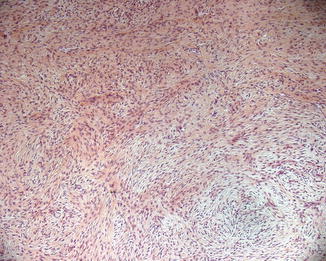
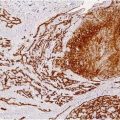
Fig. 29.2
Low-grade fibromyxoid sarcoma. Collagenized and myxoid areas with spindle cell proliferation
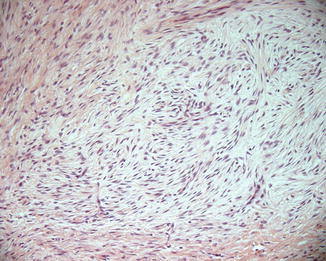
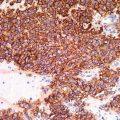
Fig. 29.3
Low-grade fibromyxoid sarcoma. The spindle cells have a deceptively benign appearance, with no or slight nuclear pleomorphism
Some recurrences and metastases have demonstrated zones of increased cellularity and somewhat increased mitotic activity. However, such areas have typically regular cells without pleomorphism.
Neoplastic cells stain with vimentin and show variable focal positivity for muscle-specific actin; smooth muscle actin, desmin, and calponin; and CD34, while they are negative for S-100 protein, nuclear β-catenin, h-caldesmon, CD31, Leu-7, neuron-specific, cytokeratin, and epithelial membrane antigen. Recently, MUC4, a transmembrane glycoprotein that functions in cell growth signaling pathways, has been reported as a highly sensitive and specific immunohistochemical marker for LGFMS. Moreover, 90 % of LGFMS exhibit the t(7;16)(q34;p11) translocation encoding a FUS/CREB3L2 fusion oncoprotein. Less frequently, FUS/CREB3L1 fusion oncoprotein is expressed.
Differential Diagnosis
The differential diagnosis encompasses a number of entities characterized by spindle cell proliferations with myxoid morphologies. Being LGFMS a low-grade tumor, it can mimic both malignant and benign entities. Regarding soft tissue tumors, the main differential diagnosis includes low-grade myxofibrosarcoma, myxoid neurofibroma, peripheral nerve sheath tumor, schwannoma, myxoid solitary fibrous tumor, desmoid fibromatosis, epithelioid sarcoma, sclerosing epithelioid fibrosarcoma, superficial angiomyxoma, superficial acral fibromyxoma, and acral myxoinflammatory fibroblastic sarcoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree