18 Local flaps for facial coverage
Synopsis
 Always consider the defect when panning a flap.
Always consider the defect when panning a flap.
 Assess availability and laxity of local tissue.
Assess availability and laxity of local tissue.
 Rob Peter to pay Paul but only if Peter can afford it.
Rob Peter to pay Paul but only if Peter can afford it.
 Match the flap to the defect, not the defect to the flap.
Match the flap to the defect, not the defect to the flap.
 Keep your reconstruction as simple as possible.
Keep your reconstruction as simple as possible.
 Good cosmesis is vital but function trumps cosmesis.
Good cosmesis is vital but function trumps cosmesis.
 If unsure of how to proceed, for whatever reason, use a temporizing approach.
If unsure of how to proceed, for whatever reason, use a temporizing approach.
Introduction
The basic rule in local flap surgery of the face is that you can rob Peter to pay Paul but only if Peter is sufficiently wealthy. On the face, cosmesis is of prime importance. There is a tendency not to consider tissue expansion in local flap surgery. The surgeon should think of using this technique when indicated, since it supplies the ideal skin cover and the amount of skin is usually plentiful. Also, there is only one surgical area. A variant of tissue expansion is used in many reconstructive efforts. When a wound is closed tightly or a flap which seems too small is used and yet the defect is closed, the biomechanical properties of creep and stress relaxation have been harnessed, and the skin elongates over time (Table 18.1). There is a limit to these mechanisms, and skin blood supply must also be considered. Familiarity with such techniques is essential in all flap procedures, and this knowledge is a “must” for all plastic surgeons, regardless of seniority.1–3
Table 18.1 Viscoelastic properties of the skin
| Creep | When a sudden load is applied and kept constant, skin will stretch. |
| Stress relaxation | A constant load on the skin will cause lengthening. With time, the load required to maintain the lengthening decreases. This explains why white flaps will frequently become pink with time. |
There are many challenges in facial reconstruction. The reasons for this are variations in color, texture, areas of hair-bearing skin, wrinkles, nerve supply, and function. In addition to these significant challenges, there are specific three-dimensional anatomic areas, including the nose, lips, ears, eyelids, and eyebrows that require specific (and often difficult) reconstructive techniques in order to achieve optimal functional and aesthetic results.2
Forehead and scalp
The characteristics of the forehead vary considerably with age and nationality. The smooth forehead of youth becomes the wrinkled forehead of seniority. The high, hair-free forehead of the Caucasian individual is different from the Indian or Arab forehead, which is small in all dimensions because of the anterior encroachment of hair; the former makes for much easier reconstruction than the latter. All foreheads have a limited amount of spare skin and, as a result, wide undermining and freeing are necessary to deal with many skin defects. Also, the forehead is surrounded by a frame with distinct outlines, mainly of hair that should not be disturbed, where possible (Table 18.1).
Rhomboid flap
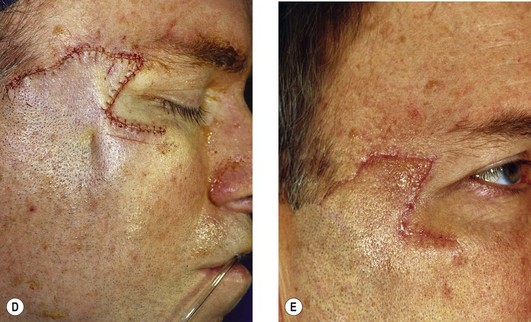
This flap can be used, but as with all flaps, it is important to check if the tissue is available. In the forehead, vertical donor sites are preferred to horizontal sites, which may cause an upward shift of the eyebrows or downward repositioning the forehead hairline (Fig. 18.1).3 Small rotation flaps or transposition flaps are also possibilities; however, these tend to “trap-door” because of their round or oval design. In larger defects, a triple rhomboid may be used; this necessitates an excision of a hexagonal design (Fig. 18.2). Careful planning and assessment of the availability of loose skin in all three areas of flap harvest is essential.3–5 In the temporal area, 3.5 cm flaps can be used, but this requires great care in order to prevent too great a shift of the hairline. This applies to reconstruction of any area on the nonhair-bearing scalp in proximity to the hairline edge (Fig. 18.3). Direct advancement flaps are possible but can only close smaller defects. Once again, the direction of hair growth must be considered. Island flaps are used only occasionally; they are frequently based on subcutaneous tissue rather than on definite blood vessels. This necessitates taking great care to maintain every subcutaneous strand possible and tension must be minimized.
Bilobed flaps can be used, but they tend to trapdoor or pincushion and are therefore obvious in any form of indirect lighting. Because of this, they are generally not recommended, though they do continue to be used and are sometimes the best way to reconstruct a given defect.6,7 A small forehead with a lot of surrounding hair encroaching onto the forehead represents a considerable problem. Laser hair removal should be considered in such a patient. Large forehead reconstruction is treated by tissue expansion; this allows reconstruction by simple advancement or one of the expanded flaps described previously (Fig. 18.4).8 Post-expansion size increases will decrease when the expander is removed and this must be taken into consideration when planning the reconstruction. Thus, a degree of over-expansion is strongly advised.
Eyebrow reconstruction
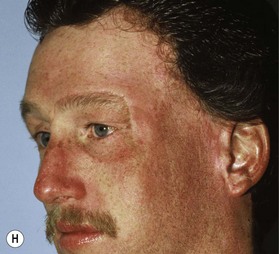
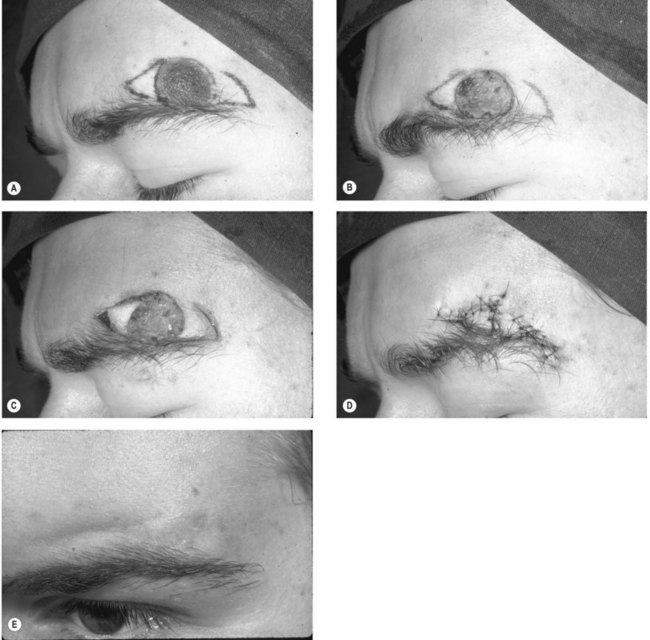
The eyebrow is complex and reconstruction is difficult, this is because hair grows in a fixed pattern that is not uniform and is difficult to reproduce exactly. A scalp island flap based on the temporal blood supply can be used, but the hair must be trimmed. The hair is often too dense and does not grow in the correct manner. In spite of this, the reconstructed eyebrow can be much appreciated by the patient, especially in the burned patient in whom both eyebrows are frequently involved. In such a patient, symmetry can be achieved. This, however, varies in degree. An alternative technique is micro-hair transplants with frequent trimming. These, unfortunately, rarely produce the unique anatomy and the density of the eyebrow hair. Eyebrow flaps must be designed with care to maintain the correct anatomic relationship (Fig. 18.5). Unfortunately, there may be a shortage of material available, and it may not be possible to have the eyebrow in the exactly desired anatomical position or size.
Nasal reconstruction
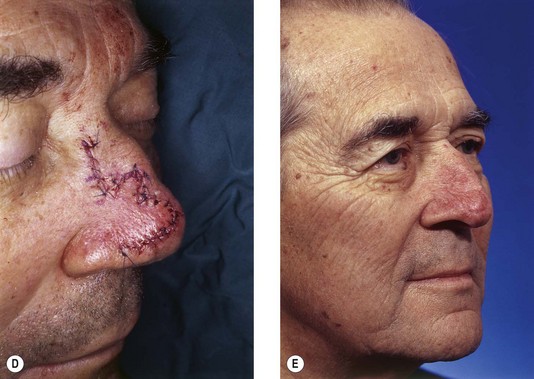
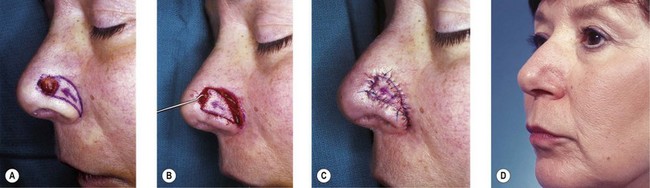
Many different flaps for nasal reconstruction have been described. In the bridgeline region, the glabella is the preferred donor site, and the variety of flaps can be the direct advancement type (Fig. 18.6), transposition (Fig. 18.7), bilobed (Fig. 18.8), rhomboid (Fig. 18.1), or island (Fig. 18.9). On the lateral aspect of the nose, bilobed (Fig. 18.8), rotation (Fig. 18.10), or transposition flaps (Fig. 18.11)5–8 – all can provide excellent results. Fortunately, there is often more skin available in this area than expected.
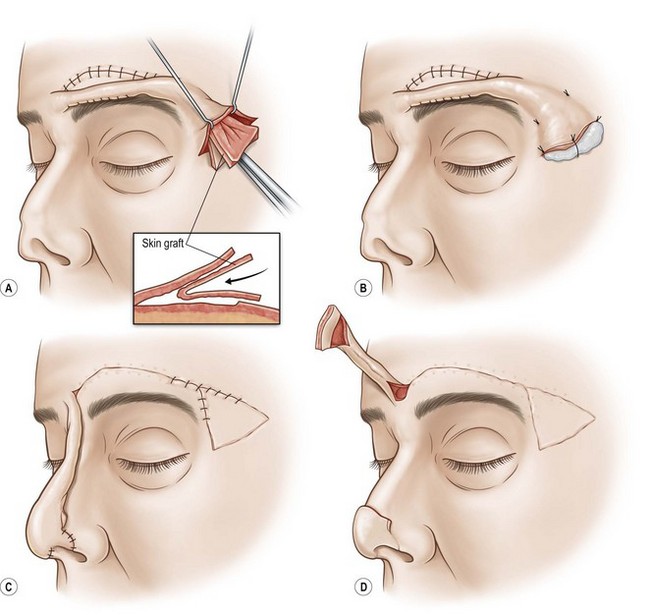
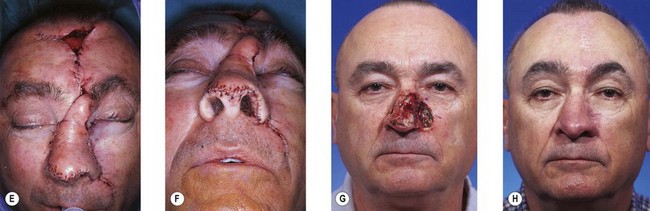
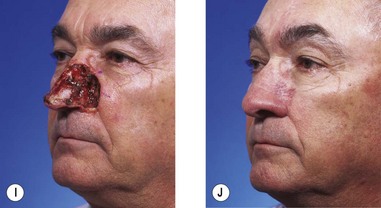
To provide an acceptable nasal tip reconstruction, the bilobed flap is ideal, though, as already mentioned, it does have a tendency to trapdoor. The long advancement flap of Rintala,9 which looks unreliable, usually works well but can cause some apprehension on the part of the surgeon and the patient due to skin color changes (Fig. 18.11). Another method is that of Schmidt,10 in which the supraorbital area (i.e., just above the eyebrow) is tubed to a dimension that will reach to the nasal tip. Laterally, a nostril is made by dissecting a skin pocket and lining it with a skin graft and cartilage. The latter provides the required support and is placed if possible and if necessary. Remember – simple surgery if possible! Approximately 2–3 weeks after the initial reconstruction, this composite is brought down to reconstruct the rim and the alar region (Fig. 18.11). In the author’s experience, this procedure is reliable and yields good results.
A composite graft from the ear is an excellent choice when the nostril is to be reconstructed. A cutout of the planned defect is made and transferred to the ear. A portion of the rim of a satisfactory size and shape is marked out. Using the markings, a full-thickness segment of the ear is removed. Lateral to or inferior to this, a long triangular full thickness of skin is taken in continuity with the posterior surface of the ear. Closure of the ear defect causes only a minor size reduction, which rarely seems to be a problem. The nose lesion is resected with lateral skin excess. The ear graft is then sutured in place with meticulous accuracy so that raw skin edges of the graft and ear oppose exactly, and the ear rim becomes the nostril rim. In this way, revascularization of the composite graft from the full-thickness replacement area will occur with excellent results. The maximal dimensions of a composite graft are approximately 1 cm2; for defects greater than this, a composite flap of helical root is an excellent solution. A thin vertical forehead flap can also be used, but this must be based correctly (see below). When a more complex reconstruction is required (e.g., bilateral alar rims and columella), the total central forehead should be used. This area should be mapped and marked carefully to ensure that there is adequate tissue for the columella and alar rims. The flap is now elevated. The key to complete survival of the flap is the position of its base; this should be at the medial canthal level or below. In this way, the vascular anastomosis on the side of the nose between the cheek and forehead vessels can provide a satisfactory flap to close the defect. With the base correctly positioned, the midline flap will comfortably reconstruct the nasal tip and the columella without tension and with absolute safety. The reason for poor results and failures is usually due to elevating the flap pedicle based on the brow area. Another problem is lack of understanding of the vascular anatomy (i.e., anastomosis between the facial and the forehead vascular systems in the superolateral area of the medial orbitolateral nasal area). The forehead is closed directly, but if there is tension in the area just anterior to the hairline, it should be left to close spontaneously. The scar resulting from this rarely, if ever, requires any reconstruction The pedicle is divided at 2–3 weeks, depending on the inset, and the nasal tip is fashioned. Apart from thinning, it is unusual to require further adjustments (Fig. 18.12). If there is any concern about vascularity, the flap base is delayed.
If a total nasal reconstruction is required, a larger amount of forehead skin is harvested in the transverse dimension, but again, the base should be positioned at or below the medial canthal ligament. The septal mucosa is used for lining. For closure of the midline forehead defect, the skin can frequently be mobilized extensively and advanced. If there is concern, a tissue expander can be inserted to expand the whole forehead. This gives a large amount of skin with a good blood supply. If nasal support is needed, a cranial bone graft from the outer table of the skull is taken from an area where the curvature is similar to that required for the defect reconstruction, the shape can be chosen to some extent.11 This may be done at the same time with secure screw stabilization of the bone graft in the forehead/nose junction. It may be safer to delay grafting to the time of flap division or to a third procedure. A less common method to reconstruct the tip of the nose is to use a donor site from the neck, but there can be problems with color and texture of the neck skin and the contours, due to the softness of the subcutaneous tissue.
Noses may be prefabricated elsewhere (e.g., on the forearm using a radial flap) and subsequently transferred by microvascular techniques. Initially the results left a lot to be desired but with experience and technique refinement, the results are now much better and complications less troublesome.12
Eyelids
Partial lower lid defects
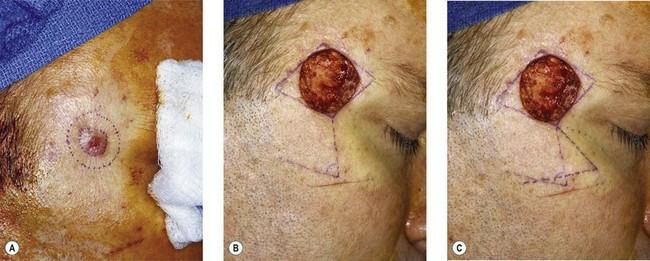
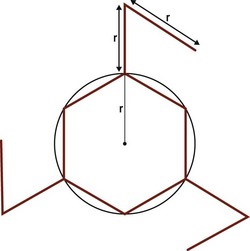
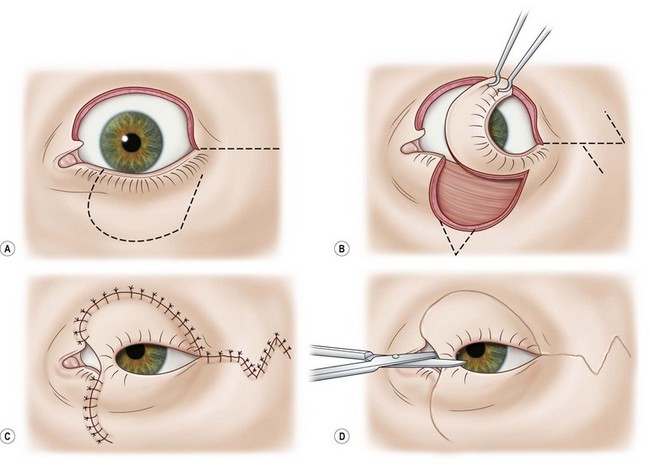
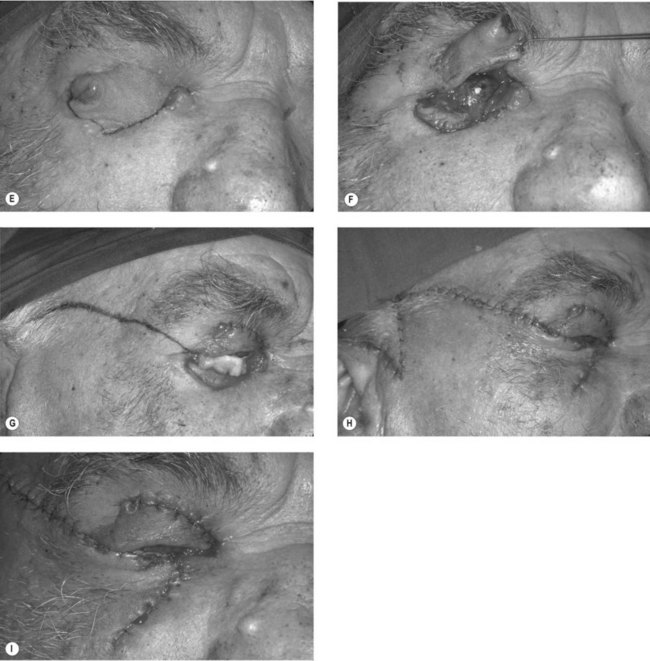
Lesions are frequently resected in a V fashion and the resulting defect can be carefully closed in layers. If this is not possible, the lower portion of the lateral canthal ligament is divided through a small lateral canthal incision. This allows the lid to move medially, and closure can be obtained without tension. If there is too much tension, the incision and dissection are taken further laterally on the cheek. Closure is then obtained without difficulty. The lateral incision is closed with a Z-plasty in order to reduce any skin tension (Fig. 18.13A–D)(Fig. 18.13E–I).13
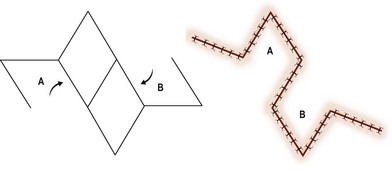
An extensive defect requires that a portion of nasal septum, with mucosa attached on one side, be inserted with the mucosa toward the globe in order to form an internal lamella.14 A portion of ear cartilage, with perichondrium in place of the mucosa, can also be used for support. Mucosalization of the inner surface occurs fairly rapidly. A cheek rotation flap of the required size then provides external cover (Fig. 18.14). If the cheek skin is insufficient, prior expansion of the lateral cheek skin should be performed, or a narrow midline forehead flap can be used. The latter has the advantage of being a little more rigid. This, however, requires accurate sizing in all dimensions, also there will be a forehead scar.