9 Local anesthetics in plastic surgery
Synopsis
 Local anesthesia is widely used for minor surgery.
Local anesthesia is widely used for minor surgery.
 Local anesthesia use can be extended to incorporate larger surgeries.
Local anesthesia use can be extended to incorporate larger surgeries.
 The benefit to the patient is to avoid general anesthesia while breathing spontaneously.
The benefit to the patient is to avoid general anesthesia while breathing spontaneously.
 Using bupivacaine in the anesthetic solution, four to six hour surgeries are also possible and bupivacaine provides some hours of postoperative pain relief.
Using bupivacaine in the anesthetic solution, four to six hour surgeries are also possible and bupivacaine provides some hours of postoperative pain relief.
 In each region, an intelligent infiltration anesthesia technique is preferable to tumescent technique.
In each region, an intelligent infiltration anesthesia technique is preferable to tumescent technique.
 For large procedures, the assistance of the anesthesiologist provides better sedation as well as the benefit of shared responsibility.
For large procedures, the assistance of the anesthesiologist provides better sedation as well as the benefit of shared responsibility.
Historical perspective
Old reports show that since 1880 Maximilian Oberst, in Halle, had been operating on patients by injecting cocaine under the skin while an assistant was compressing the veins to avoid the rapid absorption of the toxic effects of the cocaine. Some other German surgeons were using subcutaneous cocaine for minor surgeries; however, some cases of overdose as well as some fatal outcomes were also reported. In 1890, Carl Schleich,1 a German surgeon from Berlin, demonstrated in the German Congress of Surgeons the anesthetic properties of different dilutions of cocaine to perform surgeries in order to avoid toxic doses. The era of using dilutional anesthetics had begun.
At that time, William Halstead,2 an American surgeon, son of a German family, was in Berlin learning the use of cocaine as a local anesthetic. He took this practice back to America and began to use cocaine at the Johns Hopkins Hospital in Baltimore.
In 1905 a synthetic alkaloid named novocaine, similar to cocaine but with less toxic effects, was developed by A Einhorm in the Hoechst laboratories in Darmstadt. From then on, this new, less toxic anesthetic was used for local anesthesia and more extensive surgeries could therefore be performed. When Takamine and Aldrich in the Parke Davis laboratories in London developed suprarenine (later named adrenaline or epinephrine) and its vasoconstrictive effects, a surgeon from Heidelberg named Heinrich Braun3 adopted this drug and began to use it in combination with novocaine to avoid bleeding as well as to slow the absorption of anesthetic. In 1905, Braun published his first book, which went on to be reprinted seven times; it was a complete compilation of all local-regional anesthesia for almost all sorts of surgery. Braun is recognized as “the father of local anesthesia.”
Carl Gross,4 a German surgeon, also reported that the action of local anesthetics would last longer if they were diluted in a saline solution. As we can see, a very old idea was rediscovered at the end of the last century. Läwen5,6 in 1910 experimented on himself with novocaine diluted in a bicarbonate solution, reporting that in this way he obtained a more rapid and lasting anesthetic effect With regard to injection methods, Moskowicz7 in 1901 replaced injection syringes with an infusion bottle filled with anesthetic solution, following the same principle used by Matas,8,9 and later perfected by Kirschner in 1931,10 when he developed a device using carbon anhydride gas. This device facilitated infiltration under pressure, and was known as Hochdruckanestesierunapparat. Different devices powered by an electric-driven motor or using the principle of the infusion bottle are largely used nowadays in plastic surgery.
The Russian surgeon Alexandr Vishnevsky11 reported the use of novocaine diluted in 1000–2000 mL saline solution for thoracic and cardiac surgery. In the Berlin Congress of Surgery in 1955, he reported having an experience of 1193 thoracic and cardiac surgeries with this anesthesia.
Today, many plastic surgeons perform different aesthetic and reconstructive procedures under local anesthesia. These include rhinoplasties, facelifts, breast surgery, liposuction, and some lipectomies. However it has to be remembered that the idea of performing surgery under local anesthesia, new anesthetics, vasoconstrictors, large anesthetic dilutions, alkaline anesthetic solutions, devices for infiltrations, and almost everything that is used today in plastic surgery throughout the world was developed or described at the end of the 18th century and at the beginning of the 19th century by German and Russian surgeons.12–14
Patient selection
Patients with abnormal or exaggerated fears should not be accepted for local anesthesia, but others who are afraid of only some aspects of the surgery can be deemed suitable and placed in the group of ideal candidates, following a very good explanation of how the surgery is performed. This explanation should include a description of the level of anesthesia, and perhaps a visit to the operating room before surgery with someone who can answer the patient’s questions and help to ease anxiety and nervousness.15
Choice of sedation
There are several ways to sedate a patient. There are also different levels of sedation. Some surgeons use only a mild sedative, choosing to perform operations with the patient awake. Others have the patient under moderate sedation but maintaining verbal contact, while others prefer to have the patient completely asleep, that is, in deep sedation. Deep sedation may be accompanied by a partial or complete loss of protective reflexes and may include the inability to maintain a patent airway. Planned deep sedation should be administered preferably by an anesthesiologist or certified registered nurse anesthetist under the direction of an anesthesiologist or an operating physician.16
Premedication
Lorazepam has been demonstrated to be a very effective drug. It is usually administered the night before surgery and again when the patient wakes up on the morning of surgery. In this way anxiety as well as gastric secretions are reduced.17 Premedication should also vary according to each patient.
Sedation
Drugs used for sedation include diazepam, midazolam, or propofol, while for analgesia ketamine and fentanyl can be used. Some surgeons like Thomas Baker18 or Charles Vinnik19–22 use a combination of midazolam–ketamine. This is referred to as dissociative anesthesia. Ketamine is a short-acting drug that provides a rapid dissociative anesthesia lasting 45 minutes IM and 10–15 minutes IV. It has a short recovery time and is especially indicated for hypotensive patients. According to Ersek,23,24 it also decreases platelet aggregation.
The initial decision is whether the patient needs sedation, analgesia, or both.
Selection of local anesthetics
Anesthetic drugs
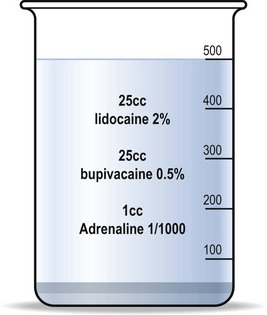
Lidocaine is a very old and safe anesthetic drug that allows 90 minutes of numbness. Its standard dose is 500 mg for a 70-kg person, or 7 g/kg, or 25 mL of lidocaine 2%, but it is known that these doses can be augmented many times (some papers mention up to five times the maximum recommended dose) (Fig. 9.1).
Vasoconstricting agents
Ornipressin is a vasoconstrictive agent without central action (it does not raise the blood pressure nor alter the cardiac rhythm). Its vasoconstrictive effect lasts 4–6 hours. One milliliter can be diluted in 250, 500, or 1000 mL of saline solution and can be combined with any anesthetic. All vasoconstrictors have the capacity to produce ischemia in the peripheral nerves that blocks the conduction of stimulus. As long as the vasoconstriction lasts, so does the anesthesia. The trade name for omnipressin was Por-8 (Sandoz) but for the moment, it has been discontinued.25
Carbonated anesthesia
There are many formulae that combine different anesthetics and vasoconstrictors.
For large aesthetic surgeries Mottura’s formula26–33 is to combine 20 mL lidocaine 2% (7 mg/kg), 20 mL bupivacaine (1.5 mg/kg), and 1 mL epinephrine 1 : 1000. These drugs can be diluted in 400–1000 mL saline solution or lactated Ringer’s (Fig. 9.1).
Selection of technique
For facelift
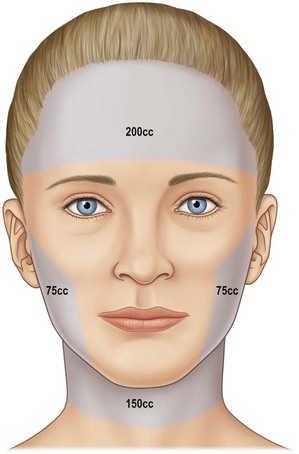
In general, the infiltration extends 2 cm beyond the whole marked area of the face and neck because the dissection can cross premarked limits (Fig. 9.2).
For breast reduction
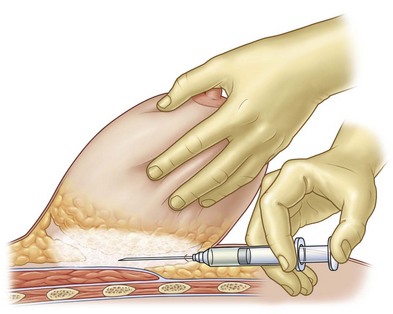
Infiltration begins in the submammary fold with 20–40 mL of the solution. The entire breast is then held firmly with one hand and pulled away from the chest wall to present the retroglandular space for infiltration. This maneuver reduces the surfaces to be anesthetized (Fig. 9.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree