9 Lips and Chin
Summary
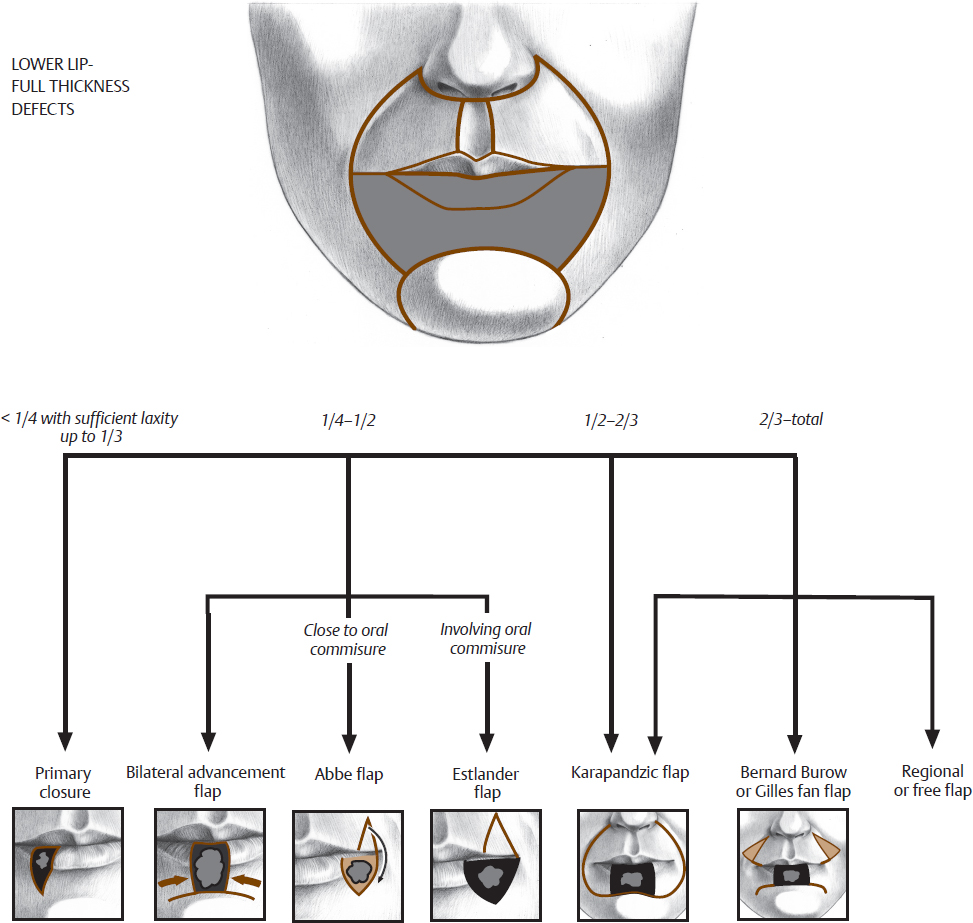
This chapter focuses on reconstruction of lip and chin defects with the goal of provide oral competence for speech and oral feeding. Lip reconstruction algorithm is directed by size with smaller defects predominantly closed with primary closure and larger defects requiring closure with well-designed flaps. The oral commissure is of added challenge and such reconstruction principles are discussed in this chapter.
Keywords: estlander flap, Abbe flap, bilateral advancement flap, karapandzic flap, Bernard–Burow flap, Gilles fan flap, oral commissure, vermilion border
The lower third of the face is dominated by the lips, which serve as the focal point for both spoken and expressive communications. Reconstruction is influenced by both functional and aesthetic considerations. The goals of perioral reconstruction are oral competency, adequate oral access, mobility, and normal anatomical proportions. When all reconstructive goals cannot be met, oral competency and access take priority.
The lip is composed of three layers: mucosa, orbicularis oris muscle, and skin. With age, there is a decrease in the skin thickness and perioral elasticity. The resulting lip redundancy is accentuated by loss of dentition and premaxillary bone. In many cases, these changes provide excess tissue for reconstruction.
The orbicularis oris muscle comprises the bulk of the lips and lacks bony attachments. Blood supply to the lips is from the superior and inferior labial branches of the facial artery. The main arterial branches are between the intraoral mucosa and the orbicularis oris muscle.
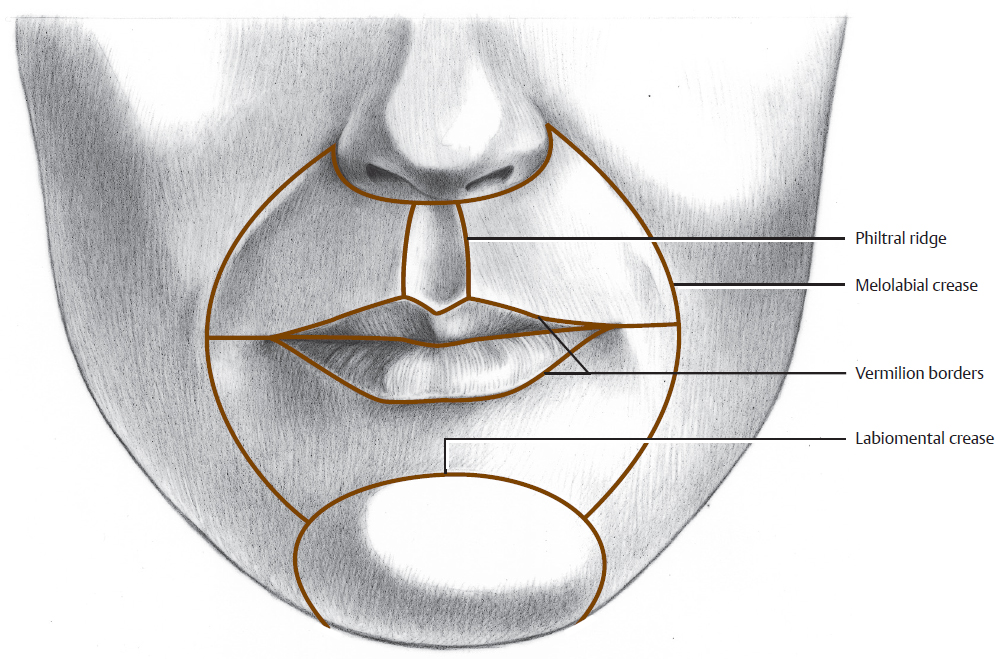
The lips and the surrounding perioral region form the oral (labial) facial aesthetic unit (Fig. 9.1). The upper lip region is divided into two lateral subunits and one medial subunit, each of which should be reconstructed as a totality when possible. The lower lip region is comprised of one skin subunit. The mucosal lips are each a separate subunit. The chin is a separate aesthetic unit, separated from the lower lip by the mental crease, bordered laterally by an extension of the crease and inferiorly by the inferior border of the mandible. Because of the close proximity of the chin and the relative rarity of cutaneous defects of the chin, this unit will be discussed in this chapter.
 Lower Lip and Chin
Lower Lip and Chin
Partial Thickness
Because the majority of lower lip carcinomas involve the vermilion, their excision usually involves a full-thickness resection. In addition to the treatment of tumors (especially squamous cell carcinoma), leukoplakia or actinic damage of the lower lip mucosa is common and should be treated with a vermilionectomy (Fig. 9.2). The mucosa is excised from the mucocutaneous junction posteriorly as far as the lesion extends and to the depth of the orbicularis oris musculature. The mucosa on the buccal surface of the lip is then sharply and bluntly undermined and advanced to the previous mucocutaneous junction. Minimizing the amount of mucosa sharply elevated maximizes the preservation of cutaneous sensory innervation to the mucosa and future lip sensation. This procedure can be done on the upper or lower lips or to re-create the mucosa of the lip in total lip reconstruction. If there is not enough local mucosa for advancement, a pedicled flap can be elevated from the ventral surface of the anterior tongue. This flap is left pedicled on the dorsal anterior tongue for 10 to 14 days prior to division and inset. Using the undersurface of the tongue avoids placing the irregular surface of the dorsal tongue onto the lips.
Fig. 9.2 (a) Lower lip lesion. (b) Lower lip vermilion mucosal advancement. (c) Appearance after closure. (d) Postoperative appearance mouth closed. (e) Postoperative appearance mouth open.
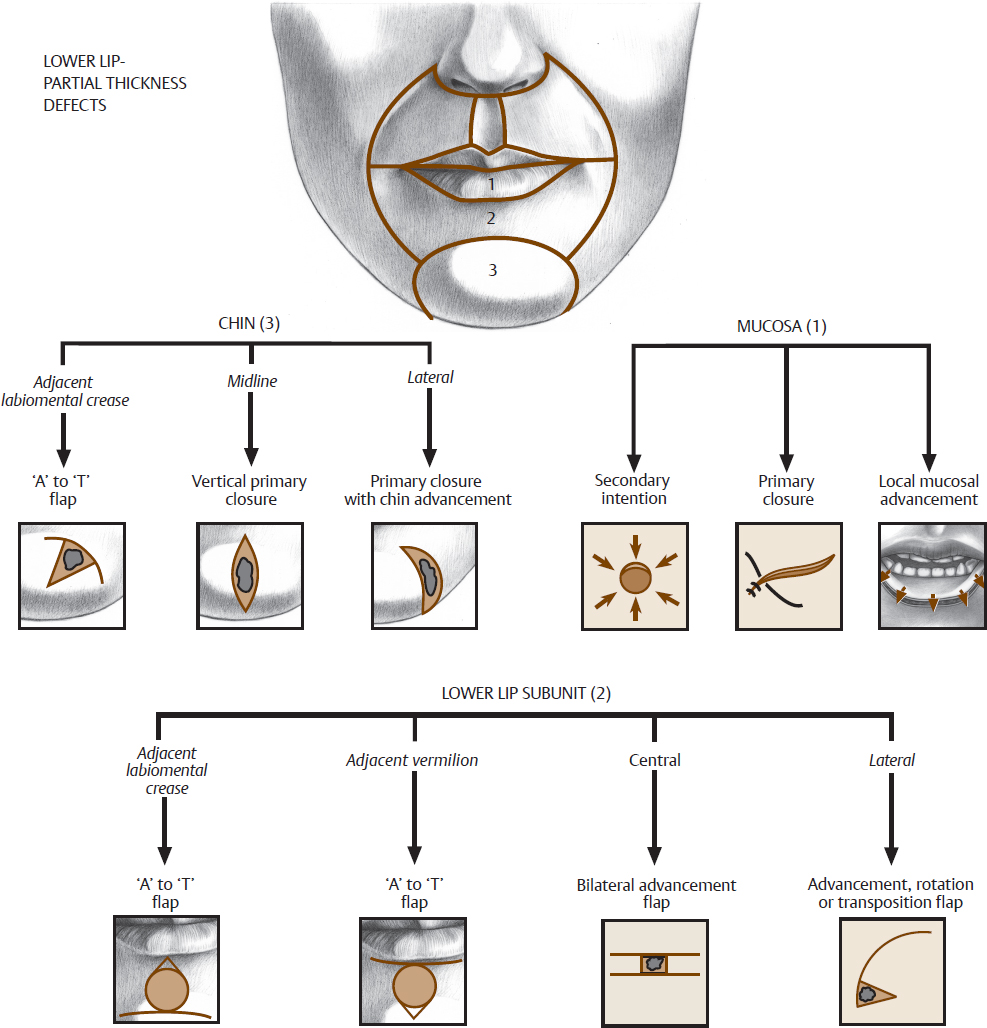
Skin-only defects of the lower lip are less common and can usually be closed primarily or with local skin flaps (Fig. 9.3). Lesions adjacent to the labiomental crease or the vermilion are closed using the A-to-T flap (Fig. 9.4). The releasing incisions are placed in the labiomental crease or the vermilion border, respectively, depending on the location of the lesion. The primary defect is then closed parallel to relaxed skin tension lines (RSTLs).
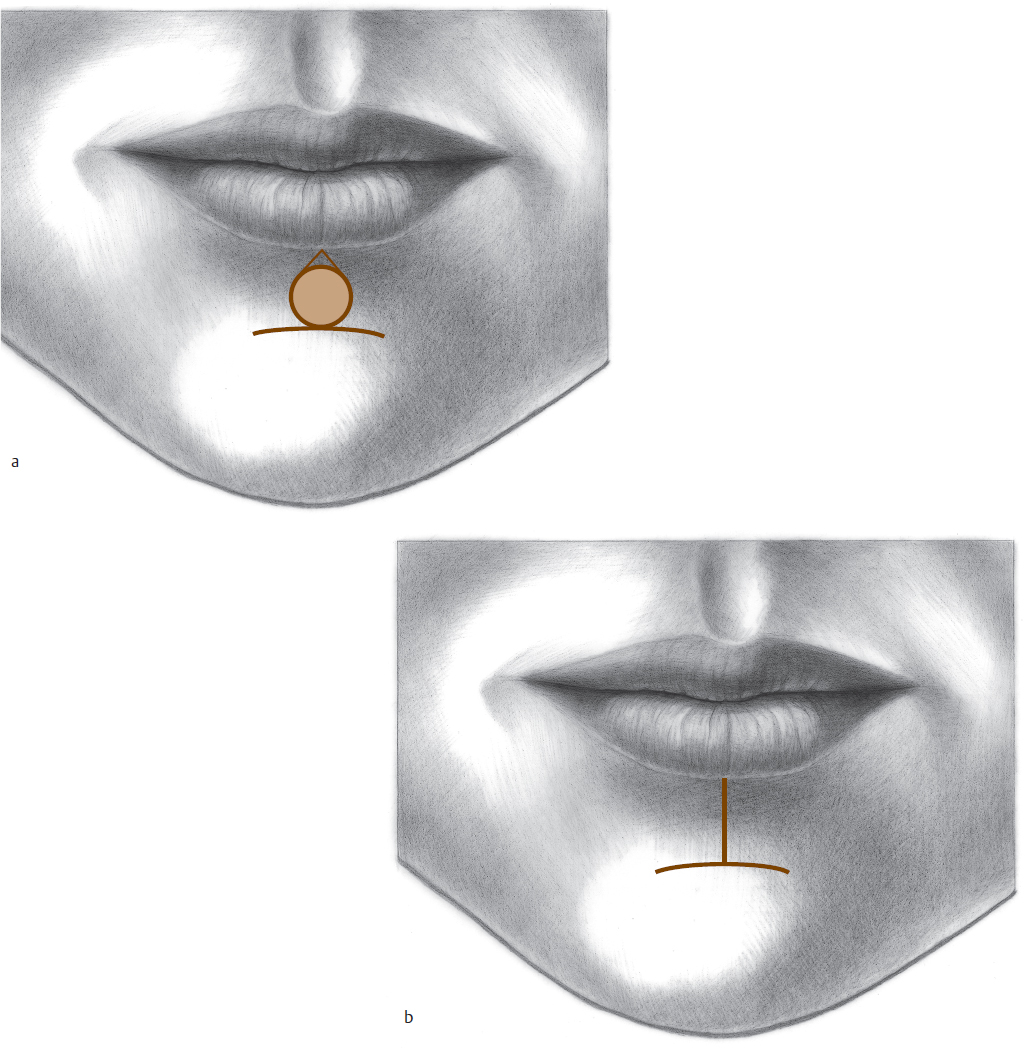
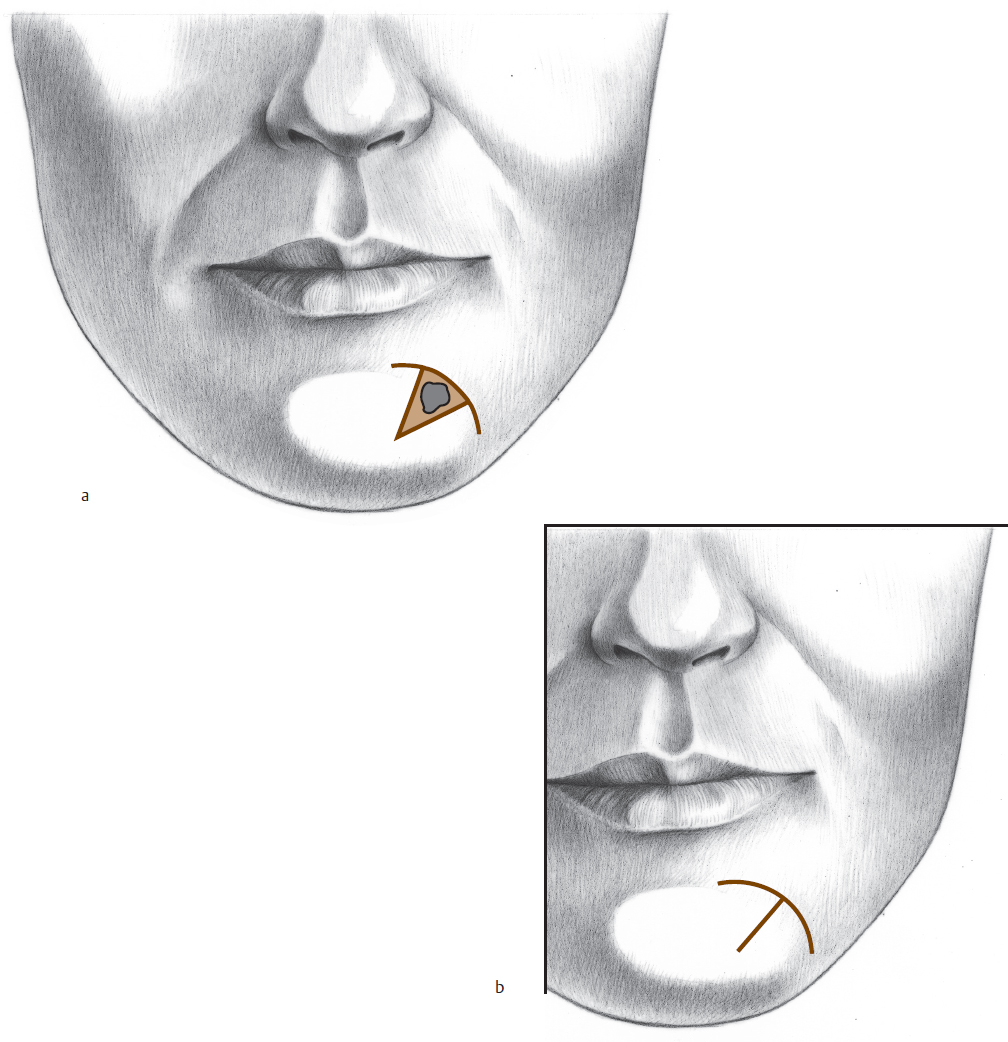
Defects of the chin adjacent to the labiomental crease can be closed with an A-to-T flap of appropriate depth (Fig. 9.5 and Fig. 9.6). Defects of the chin in the midline can be closed with a primary vertical or horizontal closure (Fig. 9.7). Soft tissue can be debulked in the midline to make the chin symmetric. If the mandible is asymmetric or overly protuberant, the bone can be reduced to facilitate closure. If the defect is located offto one side, the chin can be advanced to the deficient side and contoured appropriately with subcutaneous dissection (Fig. 9.8). Fat “flip-flop” flaps can be used to maintain symmetry. If significant subcutaneous tissue is lost, chin augmentation with an implant may be necessary at a later time.
Fig. 9.6 (a) A-to-T flap planned for the chin. (b) After closure. (c) Late postoperative appearance.
Full Thickness
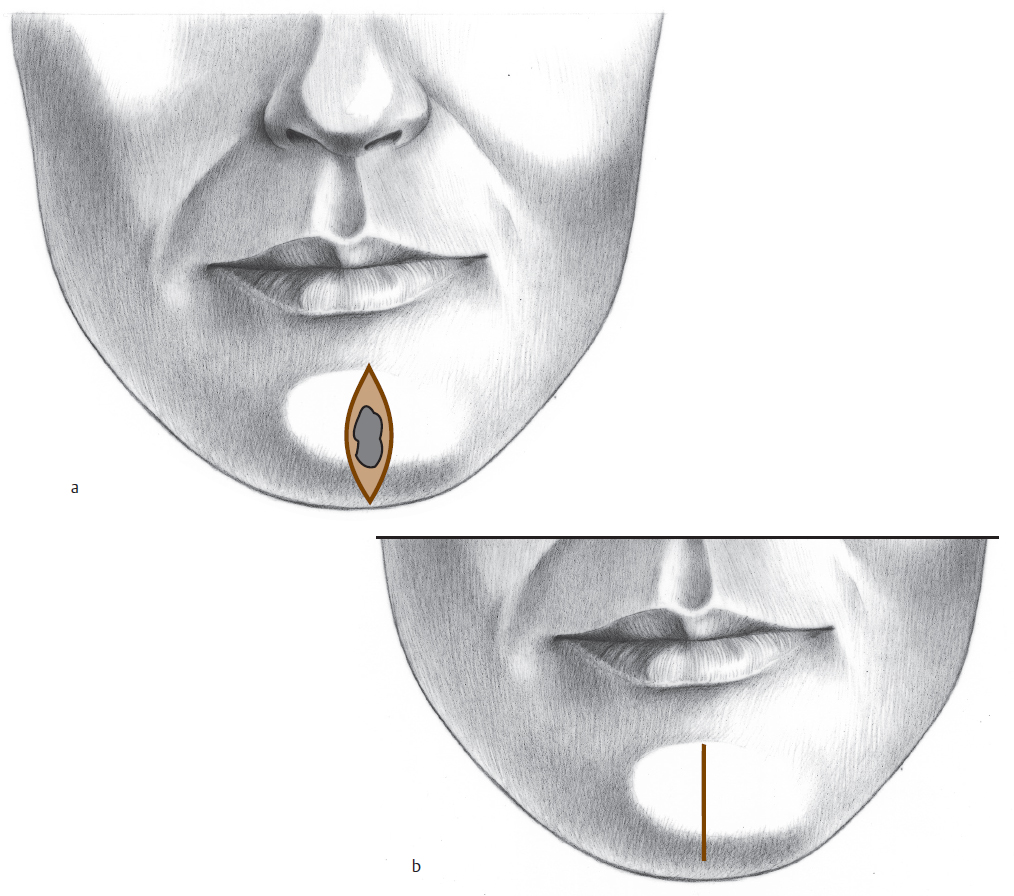
Because of the great elasticity of the lower lip, full-thickness lesions involving one-fourth to one-third of the lower lip can be excised and repaired primarily (Fig. 9.9). For the smallest lesions, a standard V excision is often used. The V excision should not cross the labiomental crease and should be planned so as to parallel RSTLs (Fig. 9.10). The mucocutaneous junction should be tattooed or scratched prior to all full-thickness lip excisions, to facilitate exact alignment of this important surface landmark at the end of the procedure. The wound is closed in three layers of mucosa, muscle, and skin. The anterior vermilion border should be approximated with the first cutaneous suture. The muscle layer is approximated with 3–0 and 4–0 absorbable sutures. The skin is closed with 5–0 or 6–0 nonabsorbable sutures, and the mucosa is loosely closed with absorbable sutures.
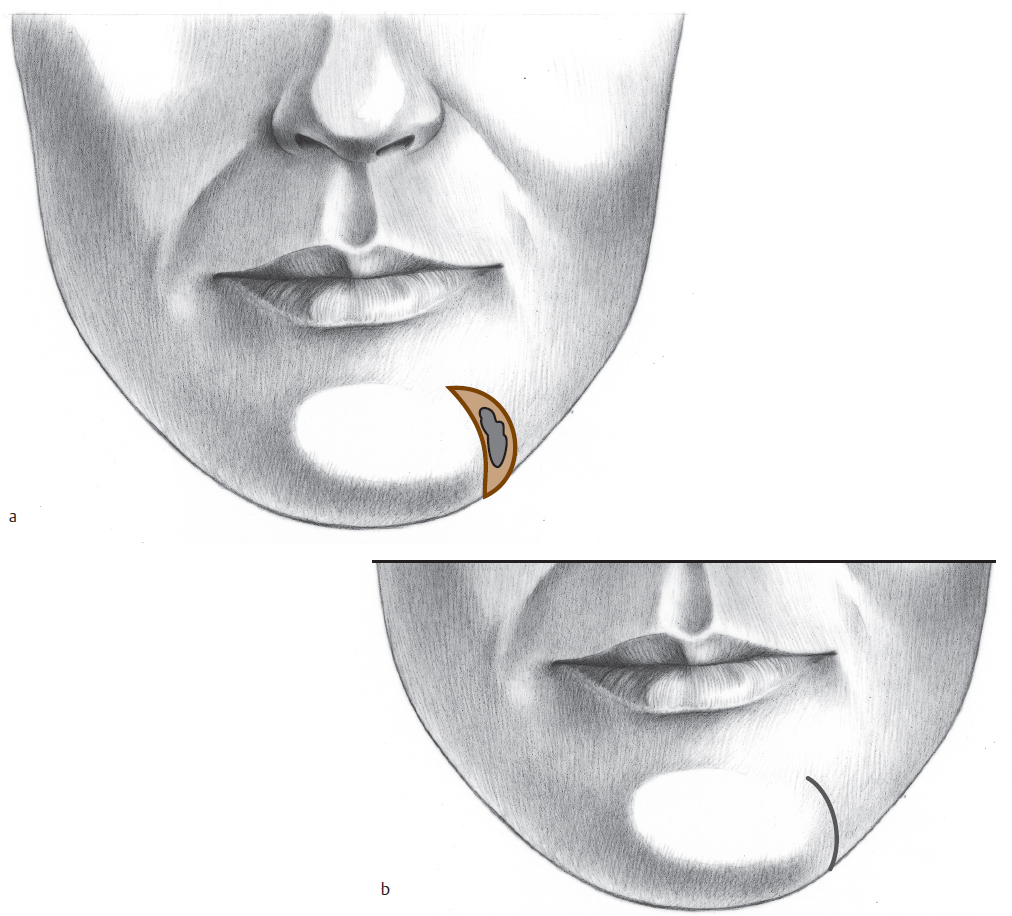
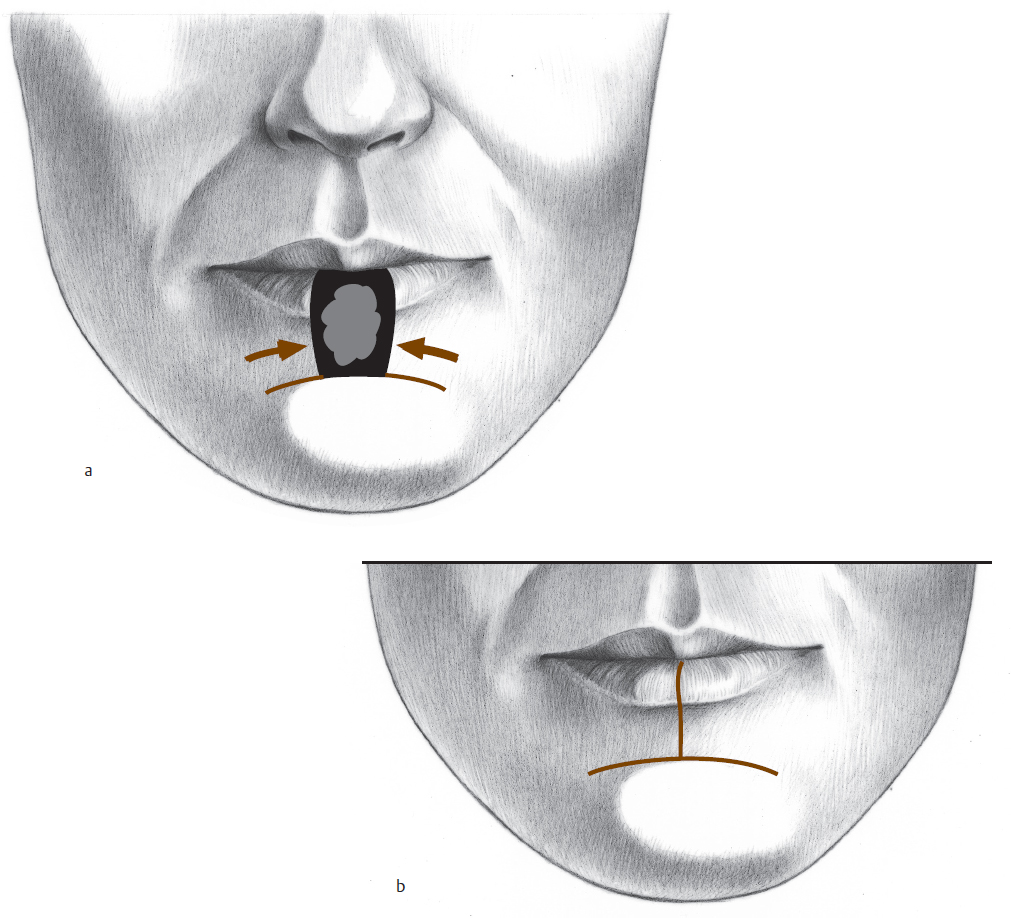
For more centrally located tumors occupying up to one-half the lower lip, a rectangular excision with full-thickness bilateral advancement flaps incised in the labiomental sulcus will facilitate closure (Fig. 9.11 and Fig. 9.12). Burow triangle excisions at the labiomental sulcus may be necessary for proper wound alignment (Fig. 9.13). The wound is closed in three layers.
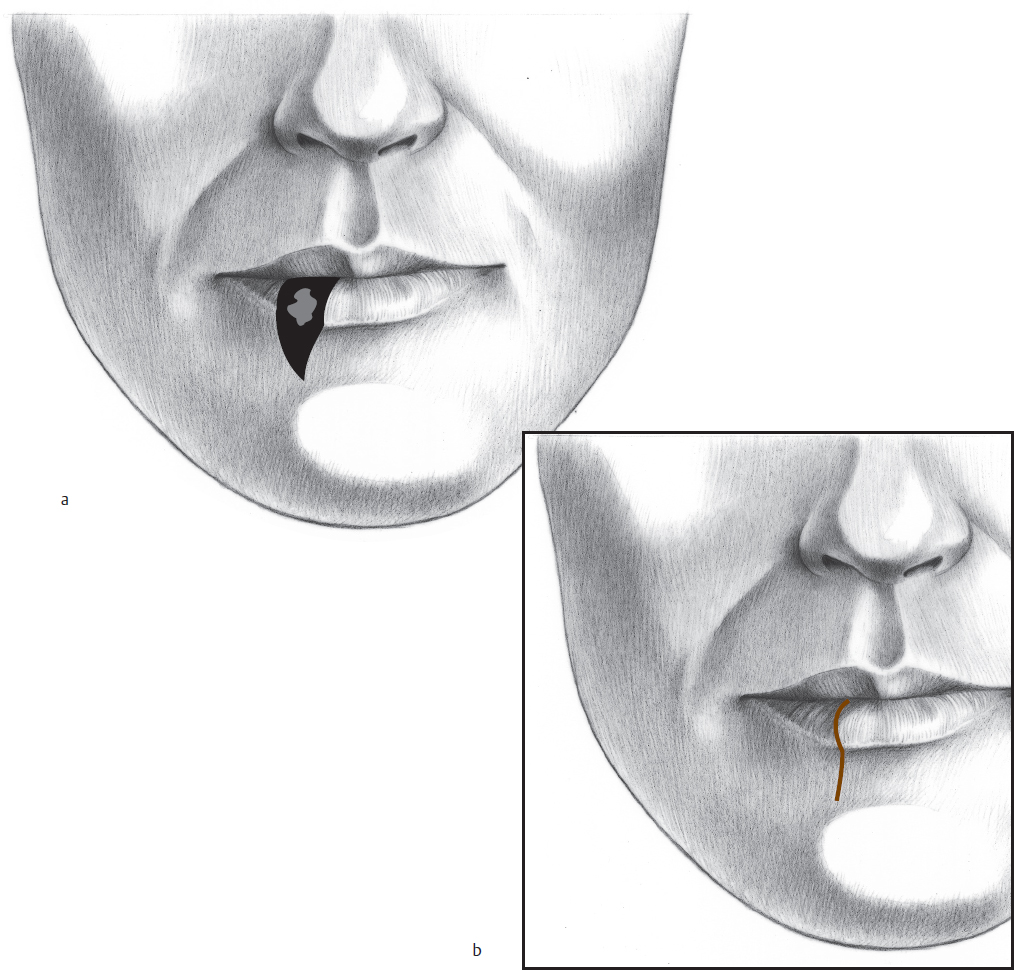
It is helpful to visualize lower lip reconstruction as a spectrum from wedge excision to bilateral advancement flaps to Abbe flaps and/or the Bernard–Burow repair. One can begin with a wedge excision and if there is excessive tension or distortion create bilateral advancement flaps. If there is a need to do a simultaneous excision of the vermilion, mucosa can be advanced from the oral surface of the advancement flaps. Although for defects of intermediate size one would normally use an Abbe flap, occasionally a unilateral Bernard–Burow is indicated. This would be the case, for instance, in someone for whom a staged repair was logistically impossible.
Fig. 9.12 (a) Full-thickness defect of the lower lip with planned bilateral advancement flap closure in the labiomental crease. (b) Flap incised. (c) After closure.
Fig. 9.13 (a) Lip lesion planned for vermilionectomy, full-thickness excision, and M-plasty excision at the labiomental sulcus to facilitate primary wedge closure. (b) After excision and three-layer closure. (c) Early postoperative appearance. (d) Oral competency and muscle function are intact with primary wedge closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree