IN THIS CHAPTER
- •
Introduction 15
- •
Preoperative preparation 15
- •
Perioperative data 21
- •
Drains 23
- •
Postoperative considerations 23
- •
Liposuction of the abdominal flap 23
Liposuction is an important part of abdominoplasty and abdominal contouring procedures. It should be performed in a well thought-out and organized manner in order to optimize safety and the aesthetic result. It can be used concurrently with abdominoplasty procedures to appropriately thin the abdominal flap while maintaining vascularity. If the patient is actively smoking or has other potential healing issues, less aggressive liposuction, less tension during closure, or both should be performed. Smoking cessation is strongly preferred.
Introduction
Liposuction plays an integral role in abdominal contouring procedures. Most patients presenting for abdominal contouring benefit from the concurrent use of liposuction. Whether liposuction is used to thin the abdominal flap, to contour adjacent areas such as the hips and thighs, or to contour the posterior trunk, it is indispensable in achieving an optimum aesthetic result. The goal of most body contouring procedures is not only to improve the contour and shape of the abdomen, but to achieve a smooth, flowing, harmonious contour by improving the overall silhouette and appearance of the region. In this chapter we will discuss the specific caveats of liposuction in abdominoplasty, including the technical aspects of tumescent infiltration, power-assisted liposuction (PAL), ultrasound-assisted liposuction (UAL), and a review of the instruments and techniques used to achieve optimal results.
Introduction
Liposuction plays an integral role in abdominal contouring procedures. Most patients presenting for abdominal contouring benefit from the concurrent use of liposuction. Whether liposuction is used to thin the abdominal flap, to contour adjacent areas such as the hips and thighs, or to contour the posterior trunk, it is indispensable in achieving an optimum aesthetic result. The goal of most body contouring procedures is not only to improve the contour and shape of the abdomen, but to achieve a smooth, flowing, harmonious contour by improving the overall silhouette and appearance of the region. In this chapter we will discuss the specific caveats of liposuction in abdominoplasty, including the technical aspects of tumescent infiltration, power-assisted liposuction (PAL), ultrasound-assisted liposuction (UAL), and a review of the instruments and techniques used to achieve optimal results.
Preoperative Preparation
There are several decisions that must be made before the patient is brought to the operating room. Among these are the preoperative markings that will guide the surgeon as to the areas and extent of liposuction, the entry sites, whether UAL will be needed, the volume of tumescent fluid needed, concentration of lidocaine and epinephrine per liter of infiltration fluid, as well as patient positioning. Addressing these decisions preoperatively will facilitate efficient use of the operating room and staff, reduce the overall time the patient is under anesthesia, and optimize safety, and provide superior results.
Patient Positioning and Intraoperative Precautions
Patient positioning depends on the area or areas that need to be treated, other procedures the patient will be undergoing, the patient’s body habitus/BMI, and surgeon preference. If the patient is scheduled to undergo liposuction of the abdominal flap as well as the lumbar area, then both prone and supine positioning is usually recommended. Some surgeons prefer using the left and right lateral decubitus positions instead of a combination of prone and supine.
One caveat with regard to patient positioning is that it is better to have sufficient and efficient positioning and achieve the optimum aesthetic result during the initial surgery than to have to return to the operating room for revisions and correction of contour irregularities. With that said, we believe that the prone and supine positioning offers the best opportunity to achieve symmetry by simultaneously evaluating the left and right sides of all body areas, and reduces the need for revision. Certain areas, such as the lateral trunk, hips, and thighs, may be amenable to supine-only positioning, but we prefer to ensure symmetry and perform these procedures with the patient in both the prone and the supine positions, allowing better contouring of the areas from several access points and from different directions. It is import-ant to keep the patient well padded at all pressure points and safely positioned. In addition, placing lower extremity compression devices, keeping the patient warm, and placing a urinary catheter when appropriate should all be on the preoperative checklist before surgery can proceed.
Tumescent Infiltration ( Box 3.1 )
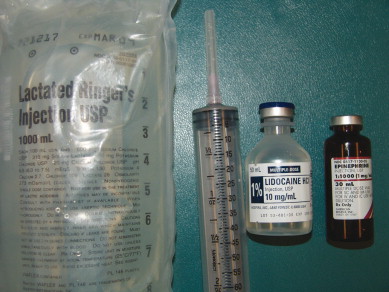
The use of infiltration fluid containing epinephrine has become obligatory when performing liposuction. The three types of infiltration methods – wet, superwet, and tumescent – differ largely according to the volume of fluid used and infiltration/aspiration ratios. All three methods involve infiltration of physiologic intravenous fluid (lactated Ringer’s solution is preferred) containing lidocaine and epinephrine. The wet infiltration method involves injecting 200–300 mL of solution per area to be treated; the superwet and tumescent techniques use larger volumes than the wet technique and have essentially become the methods of choice. The superwet technique involves injecting a volume of infiltrate that is roughly equal to the amount of aspirate that is proposed to be suctioned out. The ratio of infiltration to aspiration is approximately 1:1.5. The tumescent technique uses a larger amount of infiltrate than the anticipated amount of fat to be removed. The ratio of infiltration fluid to aspirate volume is roughly 1:1 for large-volume suctioning; for smaller procedures the ratios are higher. Small areas, such as touch-up liposuction, can have an infiltration-to-aspirate ratio of 10:1, i.e., 1000 mL of infiltrate to 100 mL of aspirate. The amount of blood loss per aspirate is comparable for both superwet and tumescent methods at approximately 1–2%.
- •
Tumescent solution should be at or slightly above bodytemperature to avoid heat loss.
- •
Epinephrine should be added to the solution just prior toinfiltration to reduce the time the epinephrine is exposed toheat and light which degrades it.
- •
The amount of lidocaine per kg patient weight shouldbe determined preoperatively. Large-volume liposuctionwill benefit from using a modified tumescent solution of12.5 mg lidocaine per liter in order to avoid surpassing thesafe maximum dose.
- •
The amount of solution needed should be judged byclinical examination, including tissue rigidity and thepresence of a fountain sign.
- •
Sufficient time should be allowed between infiltration andliposuction to achieve maximum vasoconstriction.
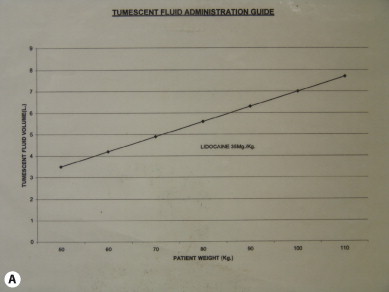
For efficient tumescent infiltration we use a pneumatic pressurized pump ( Fig. 3.1 ). This gives us continuous uninterrupted infiltration while the tumescent fluid bags are changed. This is the most efficient technique. The composition of the infiltration fluid depends on the amount of liposuction anticipated. The amount of epinephrine generally remains the same at one ampule (1 mL) per liter (1:1 000 000) of Lactated Ringer’s, and we modify the lidocaine concentration depending on the amount of proposed liposuction to keep the dosage below the accepted maximum of 55 mg/kg. We routinely keep the lidocaine dosage below 35 mg/kg, as this has an extremely good margin of safety ( Fig. 3.2 ). When large-volume liposuction is planned it is beneficial to use a modified, more dilute tumescent mixture in order to avoid exceeding the safe level of lidocaine ( Table 3.1 ).

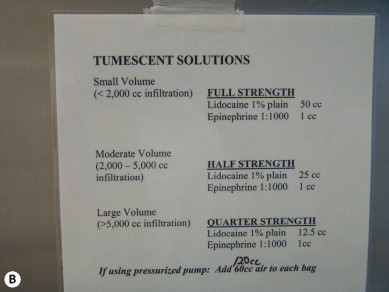
| Modified Hunstad Tumescent Fluid Solutions | ||
|---|---|---|
| Half-Strength Solution (Normal Mixture) | Quarter-Strength Solution (Large-Volume Mixture) | |
| Lactated Ringer’s solution | 1000 ml | 1000 ml |
| 1% Lidocaine plain | 25 ml | 12.5 ml |
| Epinephrine 1:1000 | 1 ml | 1 ml |
| Final concentrations (fluid warmed to 38°C) | Lidocaine: 0.05% Epinephrine 1:1,000,000 | Lidocaine: 0.0125% Epinephrine 1:1,000,000 |
Lactated Ringer’s is superior to normal saline for tumescent infiltration for many reasons. The pH is relatively neutral at 6.5, whereas normal saline is quite acidic at pH 5.0. Because of this neutral pH, it is not necessary to add sodium bicarbonate to Lactated Ringer’s-based tumescent fluid, as it is with normal saline-based fluid. Ringer’s Lactate is more physiologic than saline and is very useful for fat grafting. There is 3.5 mEq/L less sodium in Lactated Ringer’s than in normal saline. All of our liposuction solutions are kept at a temperature of 38°C or 100°F ( Fig. 3.3 ).

A few key points about infiltration fluid are worth emphasizing. The first is that although it is important for the fluid to be warm so as to help maintain the patient’s core body temperature, it must not be too hot. In addition to the physical trauma created by fluid that is too warm, one must remember that epinephrine is susceptible to degradation at elevated temperatures. Epinephrine has a recommended storage temperature of 15–25°C (59–77°F), and should be protected from light as well as from freezing. It is difficult to know at what temperature the clinical effects of degradation are noted. Our infiltration fluid is roughly body temperature at 38°C, and importantly, the epinephrine is added to the Lactated Ringer’s solution just before it is infiltrated ( Fig. 3.4 ). We have noticed a reduction in the effect of epinephrine due to prolonged fluid warming; and we have experienced poor vasoconstriction with the use of epinephrine from certain manufacturers. We cannot be sure why this occurred, but we believe that the epinephrine may have been exposed to prolonged elevated temperatures in transit from the supplier to our office. Epinephrine should be stored in a cool, dark location without direct sun exposure.
Infiltration is performed through the preoperatively designated assess sites. Entry into the access sites can be performed in a variety of ways. Using the Enter-Ease device reduces dermal bleeding from the skin puncture site ( Fig. 3.5 ). The desirable interval between infiltration and surgery corresponds to the time necessary for patient preparation and draping, approximately 20 minutes. This stepwise design is time efficient and allows the epinephrine to be maximally effective ( Fig. 3.6 ). Tumescent fluid is placed superficially first, and then at successively deeper levels ( Fig. 3.7 ). The amount of infiltration performed is determined intraoperatively. Several clinical signs can be relied on to verify that the appropriate amount of infiltration has been given, including tissue turgor, blanching of the overlying skin, and the ‘fountain sign’ ( Fig. 3.8 ).











