Lipomodeling of the Reconstructed Breast
Emmanuel Delay
Introduction
Surgical reconstruction of the breast is one of the most difficult enterprises in plastic surgery. Creating a breast of normal consistency and shape is a challenge that is still hard to meet. Defects after reconstruction are particularly marked in the medial and upper medial part of the breasts, in the décolleté area. However, this area is the most important one for the patients, as it is the most visible and plays a major role in the patient’s relationship with others in a social context (Fig. 77.1).
Until the advent of lipomodeling, there was no available technique that enhanced the décolleté or corrected the defaults of the cleavage area. Finding that fat transfer was effective in the face, we had the idea of using this technique in the mammary region in reconstructed breasts. We first began to use lipomodeling in breasts reconstructed using the autologous latissimus dorsi flap in 1998. Then, as we found the technique very effective, we decided to extend its indications to breast reconstructions with transverse rectus abdominis muscle (TRAM) flaps and to implant reconstructions. In 2001, we started breast reconstruction procedures using autologous fat transfer alone in selected cases.
The History of Fat Transfer
The idea of transferring fat from an area with an excess in adipose tissue to another where fat is lacking is not new. In 1893, Neuber was the first to describe autologous fat transfer (1). He excised deposits of adipose tissue from the arms and used them to fill a facial depression caused by mycobacterial osteitis.
In 1895, Czerny described the transfer of a lipoma to fill a breast depression after excision of a benign tumor (2). In 1910, in his paper “Freie Fettgewebstransplantation,” Lexer presented his experience with the transfer of fat deposits taken from the abdominal wall (3). Following these works, numerous authors published papers on fat transfer. In 1987, Ellenbogen recorded more than 200 authors who had used this technique (4).
A decisive advance in fat harvesting was the invention of liposuction by Illouz (5,6,7), who published his work in 1983. Fat extraction became less invasive and large quantities could be harvested by suction. Fournier refined the technique, which he called liposculpture, in 1985 (8). He modified the method of Illouz by using syringe harvesting and by carrying out microsuction and microinjections with a 13-gauge needle. More recently, Coleman combined the various improvements, introduced centrifugation, and developed a rigorous protocol, stressing the need for atraumatic fat harvesting and transfer (9,10). His preliminary work dealt mainly with the application of fat transfer in facial rejuvenation. Numerous authors have confirmed the value of fat transfer to the face, in particular in facelifts and lipodystrophy after antiprotease treatment.
The impressive results we obtained in aesthetic surgery and reconstructive surgery of the face gave us, in 1998, the idea of applying this technique to breast reconstruction. We first developed a protocol for fat transfer to the autologous latissimus dorsi flap, and we applied it during the second stage of reconstruction with nipple-areola complex reconstruction. Later, encouraged by the conclusive results, we used the lipomodeling protocol in other indications of breast reconstruction and other indications of breast plastic surgery (11,12,13,14).
Indications
Lipomodeling of the reconstructed breast is a technique that now has numerous indications. It can be used whenever there is a defect to be corrected in a small area. The décolleté (Fig. 77.1) is ideal for fat tissue transfer. In breasts reconstructed with flaps, the complementary fat transfer can add considerable volume and keep the reconstruction completely autologous while improving the size, shape, and projection of the breast.
In our department, we now consider that lipomodeling is a validated technique when it is carried out after total mastectomy. In cases in which the breast has been preserved (after lumpectomy and radiotherapy), there are ongoing studies on the correction of residual deformities of conservative treatment (15,16,17,18).
In these indications, this approach is being assessed with a strict protocol including mammography, ultrasound, and magnetic resonance imaging (MRI) evaluation before lipomodeling with long-term follow-up. Similarly, before any fat transfer is done for augmentation purposes in normal breasts, the patient is screened with mammography and ultrasound; this imaging is referred to a breast radiologist for clearance for the procedure.
Our department is carrying out mammography, ultrasound, and MRI studies on the effects of fat transfer in the normal breast to study breast imaging after lipomodeling and to avoid any coincidence with a previous breast cancer.
Contraindications
Contraindications to lipomodeling are rare and consist mainly of very thin patients with no potential donor sites. Sufficient fat deposits are in fact required to allow harvesting, bearing in mind the “twice 30%” rule: 30% of the volume harvested is lost during centrifugation and preparation, and 30% of the volume transferred is lost at a later stage because of resorption that occurs during the 4 months after the transfer.
In certain cases, the contraindication is a relative one and fat may be taken from a variety of areas, but this makes the harvesting procedure longer and more complex.
Operative Technique
Preoperative Planning
Patients are informed about the operative technique and its risks and potential complications and are given a specially designed fact sheet. It is important that the patient should be at ideal weight at the time of surgery because the fat that is transferred “remembers” its origins, and if the patient loses weight after the lipomodeling procedure, the benefit will be partially lost.
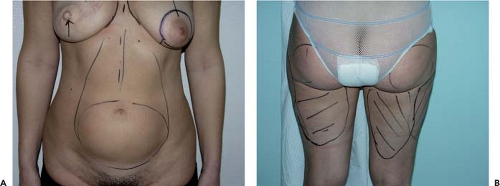
The areas of the breast that need to be treated are defined by meticulous clinical examination and marked out on the patient (Fig. 77.2). In our department, we now carry out a three-dimensional morphologic study, as well as the usual two-dimensional photographs, and this may be advantageous in assessing the quantity of fatty tissue to be transferred and the amount that will be resorbed.
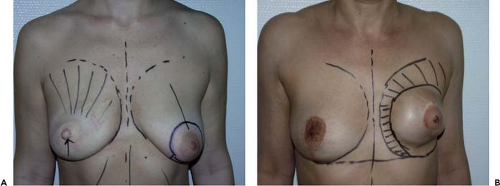 Figure 77.2. Outline of the areas to be treated. A: Lipomodeling of the autologous latissimus reconstructed breast. B: Lipomodeling of implant breast reconstruction. |
The various fatty areas of the body are examined to locate natural fat deposits. The abdominal deposit is generally used, as patients appreciate removal of fat from this area and it does not require a change in the operating position. The second site is the trochanter area (saddle bags), which may if necessary be completed by removal of fat from the buttocks in order to obtain an adequate quantity. The areas from which fat will be harvested are outlined with a skin marker (Fig. 77.3).
Harvesting Fat Without Damage
Authors who have studied adipocyte transfer have stressed the fragility of these cells (9,10,19). It has been shown that each stage of transfer can influence the percentage of resorption, as well as the long-term survival of the fat.
Recent studies have helped to standardize the techniques of fat harvesting and transfer in order to reduce the loss at each stage (19). Each stage needs to be carried out with meticulous care so that the fat will survive in the short, medium, and long term.
Use of the abdominal area for harvesting facilitates installation of the patient so that extraction and transfer will be carried out in a single operative field. If the quantity obtained is not sufficient, two lateral abdominal incisions can be made and fat can be obtained from the suprailiac areas. In some slim patients, fat from the trochanter area must be used as well as buttocks fat. In this case, the patient must be placed on a ventral decubitus, and a change of position is necessary to transfer the fat to the breast area with the patient in a half-sitting position.
General anesthesia is used because lipomodeling is usually combined with another procedure: liposuction of the inframammary fold, reconstruction of the nipple-areola complex, or a contralateral symmetry procedure. Classic preoperative antibiotherapy is usually given as with any plastic surgery. Lipomodeling does not require any specific antibiotic treatment. For less limited lipomodeling (second or third session), the procedure can be done under local anesthesia.
Before fat harvesting, we infiltrate the donor with saline plus epinephrine (1 mg of epinephrine for 500 mL of saline) to reduce blood loss and bruising.
The harvesting cannula is disposable, 15 cm long and 3 mm in diameter (Fig. 77.4). It has a blunt tip so that fat can be extracted as in classic liposuction without damaging the vessels or subcutaneous nerves. This cannula can be inserted through 4-mm incisions made with a no. 15 blade.
Fat is extracted with a syringe. The 10-mL Luer Lock syringe fits directly on to the cannula. Moderate suction is applied (Fig. 77.5) to reduce adipocyte trauma. Excessively vigorous mechanical aspiration could harm adipocyte survival. A sufficient quantity of fat must be harvested, taking into account the loss during centrifugation and the overcorrection necessary when the fat is transferred.
In order to optimize the shape of the donor sites where fat was harvested, a classic liposuction using a 4-mm cannula can be done. The skin incisions are closed using a fine, rapidly absorbed suture.
Preparing Fat
While the fat is being harvested, the assistant prepares the syringes for centrifugation. A screw cap is placed on the syringes (Fig. 77.6), and they are then centrifuged in batches of six (Fig. 77.7) for 1 minute at 3,200 rpm. The centrifugation machine has a sterilizable platter (Fig. 77.8) with a rack to hold the syringes in sterile conditions.
Centrifugation separates the fat into three layers (Fig. 77.9):
A top layer containing oil (an oily liquid rich in chylomicrons and triglycerides) from ruptured fat cells.
A bottom layer containing blood residues and serum, as well as infiltration fluid if the fat was harvested under local anesthesia.
A middle layer containing purified fat, which is the useful part. This is the layer that will be transferred, while the others are discarded: The bottom layer is drained off simply by removing the cap (Fig. 77.10), and the top layer is removed by decanting the oil that covers the middle layer (Fig. 77.11).
The team must be well organized so that the fat is prepared quickly and efficiently. Using a three-way tap, purified fat can be collected in 10-mL units by transferring it from one syringe to another (Fig. 77.12).
Transferring Fat
After preparation, a number of 10-mL syringes of purified fat are ready for use. This fat is transferred directly to the breast area using the syringes fitted with the special disposable cannulas, 2 mm in diameter. These are slightly longer and stronger (Fig. 77.13) than the cannulas used for transfer in the facial area, as the mechanical stresses are greater because the receiving tissue is firmer and more fibrous.
The incisions in the breast are made with a 17-gauge needle (Fig. 77.14), which gives sufficient access with a minimal punctiform scar. Several incisions are made, so that the area can be honeycombed with numerous microtunnels for the fat transfer.
Fine cylinders of fat (like “fat spaghettis”) are transferred in small quantities (Fig. 77.15). Microtunnels are created in many
directions. Fat is grafted from a deep toward a superficial plane (Fig. 77.16). Good spatial visualization is necessary, and a sort of three-dimensional honeycomb must be created to avoid accumulation of fat, which would lead to fat necrosis. Each microtunnel must be designed to be surrounded with well-vascularized tissue. The fat is transferred under gentle pressure while gradually withdrawing the cannula.
directions. Fat is grafted from a deep toward a superficial plane (Fig. 77.16). Good spatial visualization is necessary, and a sort of three-dimensional honeycomb must be created to avoid accumulation of fat, which would lead to fat necrosis. Each microtunnel must be designed to be surrounded with well-vascularized tissue. The fat is transferred under gentle pressure while gradually withdrawing the cannula.
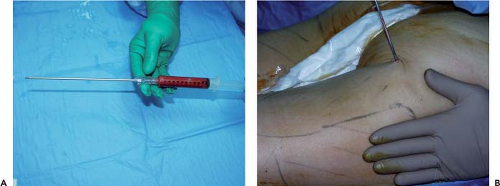 Figure 77.5. Fat extraction with a cannula fitted directly on the 10-mL Luer Lock syringe. A: cannula on the 10-mL Luer Lock syringe. B: Fat harvest with the cannula. |
 Figure 77.6. A screw cap is placed on the syringe.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|