CHAPTER 63 Lipoabdominoplasty: Advanced techniques and technologies
Introduction
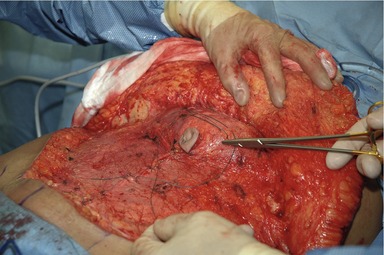
The conventional or “classic” abdominoplasty is a technique that is dependent on delamination of the abdominal skin and adjacent layers (lamina) from the deep abdominal wall (rectus abdominis muscle) fascia in order to accomplish maximum tightening of loose tissues. In most cases, this is a safe procedure, with acceptable risk of delayed healing and scarring. For some patients who have undergone massive weight loss, the conventional abdominoplasty is necessary. (Fig. 63.1).
Safety concerns over combining lipoplasty and excisional surgery
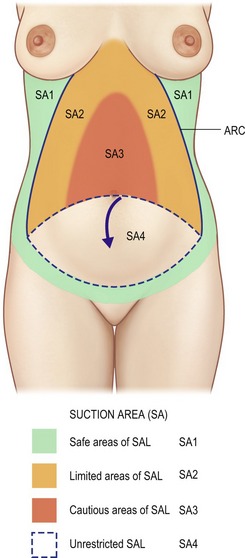
For years, the matter of combining lipoplasty and the “classic” excisional abdominoplasty was met with skepticism and safety concerns regarding the combined effect of raising a devascularized flap of abdominal tissue that had been first traumatized by a lipoplasty procedure. The “red zone” influence of the diagrams contained within articles written by Matarasso (1989, 1991, 2000)1–3 greatly influenced our thinking about the potential for central abdominal skin necrosis when conventional lipoplasty was combined with classic abdominoplasty (Fig. 63.2).
Innovations in abdominoplasty
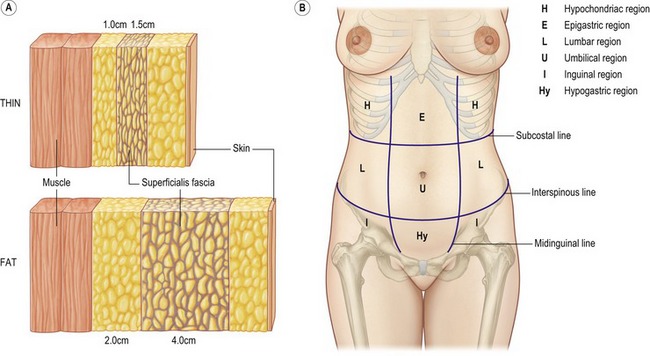
Progress on how to improve the quality of outcomes in abdominoplasty occurred when tension on the flaps was directed laterally to help shape the waist.4 Ted Lockwood in the early 1990s recognized the importance of the superficial fascia (Scarpa’s fascia) of the abdominal area to take tension off the skin closure.4,5 Avelar (1989) further refined the concept when he described a laminar approach to the abdominal wall, skin, subcutaneous fat, superficial fascia-fat matrix, and deeper fat layer6 (Fig. 63.3).
Other contributors to advanced concepts of abdominal contouring include Saldanha (2001), Shestak (1999) and Illouz (1992).7–10 The concept of safely combining lipoplasty with excisional surgery in order to improve the aesthetics of the entire abdominal region was demonstrated. Brazilian surgeons appear to have innovated the “lipoabdominoplasty”, although it is difficult to exactly credit one inventor, as several surgeons reported their own individual variations on the procedure. Matos and Ribeiro recently published an excellent review and classification of lipoabdominoplasty and its variants.11 Other surgeons, including Cardenas-Camarena and Brauman were some of the first to report lipoabdominoplasty in the American plastic surgery literature.12–13
VASER® ultrasonic lipoplasty combined with excision
When Dr Fodor, Dr Souza Pinto and I wrote the original VASER paper in 2002, I noted the capabilities of VASER® technology to deliver safe, effective, and precise outcomes that heretofore were not available with “conventional” lipoplasty or second-generation ultrasonic lipoplasty devices. The VASER® was able to safely treat all layers of tissue in areas such as the abdominal region and did not appear to inflict collateral damage to skin, vascular, lymphatics, or sensory nerves. It was possible to be selective for fat removal from the tissue matrix and still leave supporting structures largely intact, provided simple clinical guidelines were followed. The use of ultrasonic lipoplasty was initially reported by Abramson14,15 (Figs 63.4–63.6).
The effect of VASER® ultrasonic lipoplasty on the lamellae of the abdomen appears to go far beyond that of volume reduction, producing a “shrink wrap” effect on overlying tissue through a proposed tightening of the collagen rich mid-lamellar layer. Competing superficial technologies that utilize radiofrequency energy, infrared, or mechanical rollers lack a substantive effect at this depth. According to a prospective randomized study that compared conventional lipoplasty to the adjunct of laser energy delivered to the tissues done by Prado,16 there was not a substantive benefit noted.
Ultrasonic cutting devices
Additional innovation was made by Richter17 regarding how dissection above the superficial fascia could be performed to limit interruption of vascular and lymphatic structures where tissue excision is planned. Suture fixation of the superficial fascia to the deeper rectus fascia has been shown to stabilize the mons pubis and inguinal regions. Variations on this approach with resection of a midline strip of superficial fascia in the lower abdomen to access the deeper fascia for tightening have been reported by Jewell.18 Once the deeper tightening has been accomplished, the superficial fascia is closed with PDS suture (Ethicon Inc., Somerville, NJ USA). This approach works well with both procedures that require umbilical transposition or limited tissue excision from the lower abdominal region only.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree