Linear Immunoglobulin A Dermatosis and Chronic Bullous Disease of Childhood: Introduction
|
|
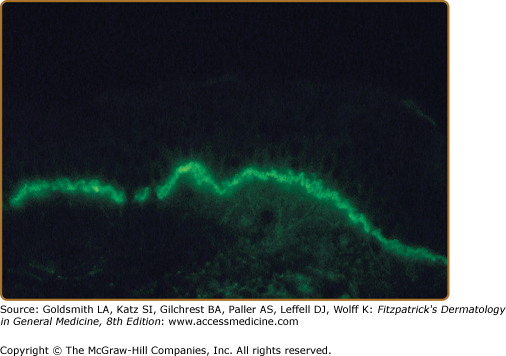
Linear immunoglobulin A (IgA) dermatosis is a rare immune-mediated blistering skin disease that is defined by the presence of homogeneous linear deposits of IgA at the cutaneous basement membrane (Fig. 58-1). Although in the original description of patients with linear IgA dermatosis it was considered to be a manifestation of dermatitis herpetiformis (DH), it has now been clearly separated from DH on the basis of its immunopathology, immunogenetics, and lack of consistent association with a gluten-sensitive enteropathy.1–4 Patients with linear IgA dermatosis can present with lesions suggestive of epidermolysis bullosa acquisita (EBA), DH, bullous pemphigoid (BP), lichen planus, prurigo nodularis, or cicatricial pemphigoid.1–6
Drug-induced linear IgA was initially described in association with vancomycin and has subsequently been associated with a wide variety of drugs.7–11 Drug-induced linear IgA has been found to differ somewhat from classic linear IgA in clinical presentation with a wider variety of clinical presentations including morbilliform, erythema multiforme like, and toxic epidermal necrolysis like.7–14
Chronic bullous disease of childhood (CBDC) is a rare blistering disease that occurs predominantly in children younger than 5 years of age and has an identical pattern of homogeneous linear IgA deposits at the epidermal basement membrane.15,16 Recent studies have demonstrated that in some patients CBDC and linear IgA dermatosis represent different presentations of the same disease process.17,18
Epidemiology
Linear IgA dermatosis occurs most often after puberty, with most patients presenting after the fourth decade of life.2,4,19 A slight predominance of females has been noted in several studies.2,4,20 In contrast, CBDC presents most often before the age of 5 years.20 As in patients with linear IgA dermatosis, there is a slight female predominance in patients with CBDC.16,20
Evaluation of the HLA association in patients with linear IgA dermatosis and CBDC has yielded conflicting results. Some investigators have found an increased frequency of the human histocompatibility antigen HLA-B8 in patients with linear IgA dermatosis, whereas others have found no increased frequency.21–23 In CBDC, an increased frequency of HLA-B8 has been noted, with up to 76% of patients expressing HLA-B8.20 Collier et al demonstrated an increased frequency of HLA-B8, -DR3, and -DQ2 in CBDC that was not seen in adults with linear IgA dermatosis.21 These authors suggested that these haplotypes may have a role in earlier disease presentation. In addition, the TNF2 allele was found with increased frequency in both adults and children with linear IgA disease when compared with unaffected subjects. There was, however, no increase seen in either adults or children when compared with HLA-DR3+ controls.
Etiology and Pathogenesis: Immunopathology
Linear IgA dermatosis and CBDC are defined by the presence of a homogeneous linear band of IgA at the dermal–epidermal basement membrane zone. A minority of patients in both groups have additional deposits of other immunoreactants, most often IgG and occasionally the third component of complement (C3).20 Because IgA is the predominant Ig of the secretory immune system, numerous investigators have attempted to determine if the IgA present in the skin of these patients is of mucosal origin. Characterization of the IgA subclass in the skin has revealed almost exclusively IgA1 and not the subclass most often associated with mucosa, IgA2.19,24,25 In addition, neither secretory piece nor J chain, both of which are present in secretory IgA, have been found in the IgA present in the skin of patients with linear IgA deposits.26 Although these data have led to suggestions that the IgA is not of mucosal origin, the true origin of the IgA deposits in the skin of these patients is not known.
Initially it was thought that patients with linear IgA dermatosis and CBDC rarely had circulating IgA antibodies against the epidermal basement membrane. Indirect immunofluorescence, using 1 M NaCl-split normal human skin as a substrate, demonstrates that the majority of patients with CBDC have low-titer circulating antibodies against the epidermal side of the split skin.19 Circulating low-titer IgA antibodies directed against the epidermal basement membrane also have been found in adults with linear IgA dermatosis.20,27 Others have reported binding of IgA antibodies from some patients to the dermal side of normal human split skin, suggesting that more than one antigen may be the target for the IgA antibasement membrane antibodies.27–29 Immunoelectron microscopic studies have been performed to determine the exact location of the IgA in the skin of patients with both linear IgA dermatosis and CBDC. Immunoelectron microscopy of the skin of patients with linear IgA deposits has revealed three distinct patterns of immunoreactants. In some patients with linear IgA dermatosis, the IgA deposits are found in the lamina lucida region of the basement membrane zone, similar to the location of immunoreactants present in the skin of patients with BP.28,29 A second pattern of IgA deposition has been detected in which the IgA deposits are present at and below the lamina densa in a pattern similar to that seen in EBA.28–30 Prost et al have described a third pattern of immunoreactants in some patients with linear IgA dermatosis in which the IgA deposits are found both above and below the lamina densa.29 In a similar manner, immunoelectron microscopic studies of skin of patients with CBDC have shown the IgA immunoreactants to be in either the lamina lucida or a sublamina densa location.17,30 These findings further support the probability that multiple antigens may be involved as the targets in both adults and children with linear IgA deposits in the skin. Horiguchi et al reviewed 213 cases of linear IgA in Japan and found a strong association between older age of onset and both IgG/IgA type and dermal binding. IgG was found in approximately 9% of patients with the infantile (CBDC) type whereas in adults (>16 years) IgG was found in 24% of patients. Interestingly, when comparing the different groups based on patterns of antigen binding (e.g., dermal vs. epidermal and IgA vs. IgG/A) no significant clinical differences were found.31
Although the relatively low titer of IgA antibodies against the basement membrane present in the sera of patients with both linear IgA dermatosis and CBDC has complicated the search for specific antigenic targets for the IgA, several investigators have made significant observations regarding the antigenic targets in these diseases. Zone et al studied sera from patients who had circulating IgA antibodies that bound to the epidermal side of 1 M NaCl-split normal human skin, as shown by indirect immunofluorescence.32 They found that serum IgA from patients with either CBDC or linear IgA dermatosis bound to a 97-kDa protein. Immunoelectron microscopy revealed that the 97-kDa antigen is present in the lamina lucida, below the hemidesmosome of normal human skin, in a location similar to where the IgA is localized in patients with CBDC and linear IgA dermatosis.33 Subsequently, Zone et al determined that the 97-kDa linear IgA bullous disease antigen is identical to a portion of the extracellular domain of the 180-kDa BP antigen (BPAG2 or collagen XVII), which is essential in anchoring basal keratinocytes to the epidermal basement membrane.34 The BP antigen (BPAG2) consists of a 180-kDa transmembrane protein and 120-kDa portion that corresponds to the collagenous ectodomain. Roh et al and Schumann et al have reported that autoantibodies in patients with linear IgA dermatosis recognize the soluble 120-kDa ectodomain of type XVII collagen35,36 The 120-kDa antigen target is not unique to linear IgA dermatosis because it is also the antigen targeted by autoantibodies in some patients with cicatricial pemphigoid and BP.35,36 Furthermore, IgA antibodies and T cells from patients with linear IgA bullous dermatosis have been found to be directed against the NC-16A region of collagen type XVII, which is the same region against which the IgG and T cells from patients with BP are directed.37,38 This may explain in part the overlap in clinical and histologic features of these conditions. Wojnarowska et al have identified another possible target antigen in patients with linear IgA dermatosis and CBDC using sera from patients in whom the IgA bound to the epidermal side of 1 M NaCl-split skin on routine indirect immunofluorescence. They found that IgA in the sera of some patients with these diseases bound to a 285-kDa protein (LAD 285) that was not the 230-kDa BP antigen or type VII collagen, the EBA antigen.39 Allen and Wojnarowska have analyzed the sera of over 70 patients with both linear IgA dermatosis and CBDC and found that the predominant antigenic target in these patients is the BP180 antigen (collagen XVII), but that some patients react with multiple antigens including the BP230, LAD 285, and other yet to be identified proteins.40 Ishtii et al described a patient with Linear IgA who had antibodies directed at the NC16a domain of BP180 without evidence of antibody formation to 120-kDa LAD 1.41 In many patients, IgA appears to bind to several different antigenic targets, suggesting the possibility that there is epitope spreading. The clinical significance of these findings however, has not been established.40
Clinical Findings
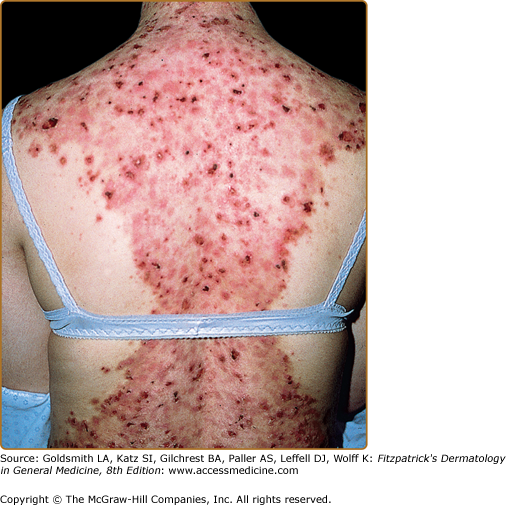
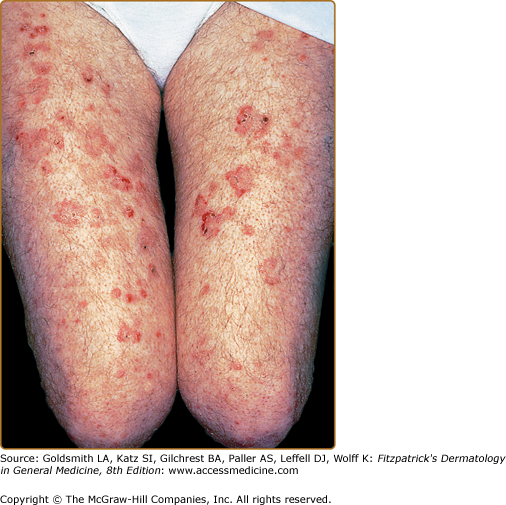
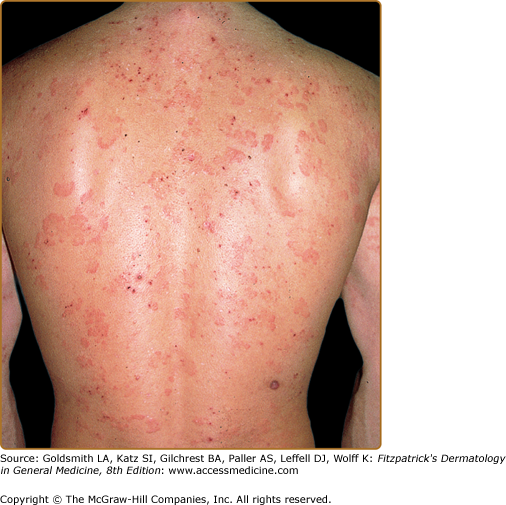
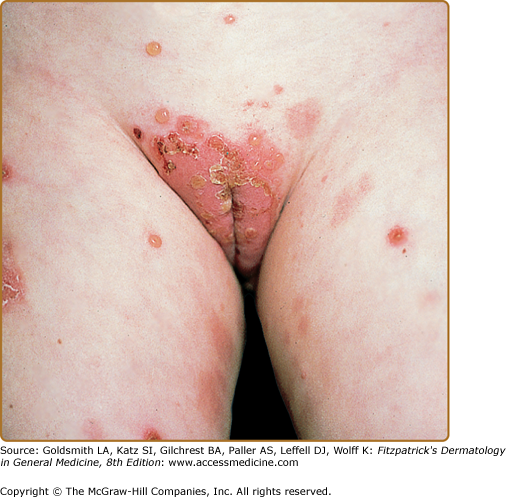
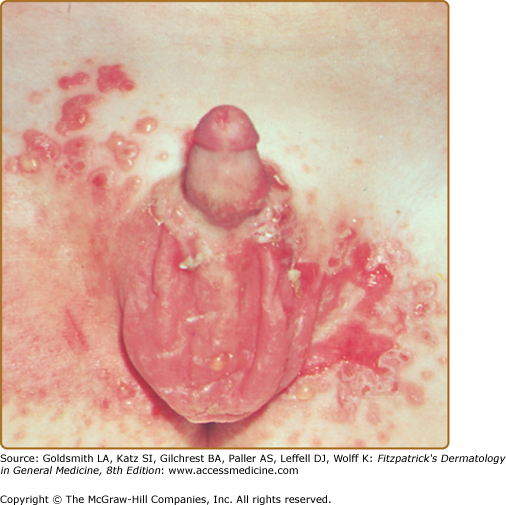
The clinical manifestations of linear IgA dermatosis are heterogeneous and often indistinguishable from those seen in patients with DH.2,4,20,42 Patients may present with combinations of annular or grouped papules, vesicles, and bullae (Figs. 58-2 and 58-3). Typically, these lesions are distributed symmetrically on extensor surfaces, including elbows, knees, and buttocks. Lesions most often are very pruritic, resulting in numerous crusted papules (Fig. 58-4). The clinical presentation can be difficult to distinguish from that seen in patients with DH. However, the degree of pruritus seen in patients with linear IgA dermatosis is variable and, in general, less severe than that seen in patients with DH. Some patients with linear IgA dermatosis present with larger bullae, in a pattern more consistent with that seen in patients with BP, or occasionally with cutaneous findings similar to those seen in patients with EBA.
Patients with drug-induced linear IgA bullous dermatosis have been reported with erythema multiforme-like findings and a toxic epidermal necrolysis-like presentation, with widespread bullae.7,11,13 Localized palmar and morbilliform variants have also been described.12,14 While vancomycin is most closely associated with the drug-induced linear IgA, a number of other medications have also been implicated including lithium, phenytoin, sulfamethoxazole/trimethoprim, furosemide, atorvastatin, captopril, and diclofenac.13 In addition, a localized linear IgA in the setting of an acute contact dermatitis has been reported.43 Recovery has been reported with discontinuation of the offending agent alone, but these patients may benefit from dapsone therapy (see Section “Treatment and Prognosis”).7,11,44
The clinical presentation of CBDC is characterized most often by the development of tense bullae, often on an inflammatory base.15 These lesions occur most frequently in the perineum and perioral region and often may occur in clusters, giving a “cluster of jewels” appearance (Figs. 58-5, 58-6, and 58-7). New lesions sometimes appear around the periphery of previous lesions, with a resulting “collarette” of blisters. Patients often report significant pruritus and/or a burning of the skin with the development of skin lesions. Patients with CBDC often present with the acute development of large numbers of tense blisters, which may rupture and become secondarily infected. CBDC differs from linear IgA bullous dermatosis of adults in its typical clinical appearance, relative paucity of serious mucosal involvement, and good prognosis.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree