Ligament Injuries of the Hand and Wrist
Karim Bakri
Brian T. Carlsen
Steven L. Moran
INTRODUCTION
Ligament injuries to the hand and wrist are common. In many cases, these injuries occur in the absence of concomitant fractures or gross radiographic abnormalities and therefore diagnosis is delayed. In addition to performing a history and physical examination, the plastic surgeon must have sufficient knowledge of joint anatomy and pathology to expediently make the correct diagnosis. In this chapter, the spectrum of major ligamentous injuries to the hand and wrist are reviewed with attention to pertinent anatomy, pathology, and treatment options.
PROXIMAL INTERPHALANGEAL JOINT
Ligament injuries around the proximal interphalangeal (PIP) joint are common. Immobility and improper splinting of the PIP joint can lead to permanent stiffness and contracture in as early as 2 weeks. It is imperative that these injuries be diagnosed and treated early. The most common injury patterns include ligament avulsions, dislocations, and fracture dislocations.
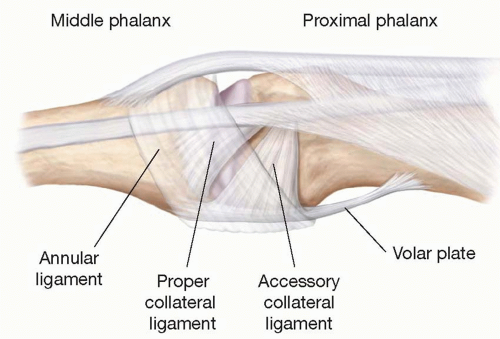
The PIP joint is a bicondylar hinge joint with 110° arc of motion in a single plane and has been called the functional locus of the hand because it produces 85% of intrinsic digital flexion and contributes 20% to the overall arc of finger motion. PIP joint stability is due to congruity of the articular surfaces and ligamentous anatomy including the proper and accessory collateral ligaments laterally and volar plate palmarly (Figure 81.1).
PIP dislocations occur in four major patterns: 1) dorsal dislocations, 2) fracture dislocations, 3) volar dislocations, and 4) lateral subluxation or dislocations. The extensor mechanism provides little support for the joint dorsally, and the bulk of dislocations occur dorsally as the middle phalanx is driven dorsally and proximally. Dislocations occurring laterally or volarly are less common and require a greater force for dislocation; these dislocation patterns often require operative intervention for successful management. A general treatment algorithm for all forms of PIP dislocation is 1) joint reduction, 2) verify the congruency of the joint surfaces throughout a normal arc of motion, 3) assess joint stability after reduction, and 4) institute early hand therapy to minimize stiffness. As a general rule, stable joints, following reduction, are treated nonoperatively, whereas unstable joints often require operative management to restore joint stability.
General Evaluation
A history is obtained to determine the mechanism of injury. Radiographs are obtained to assess concomitant fractures or evidence of ligament avulsion, which may present radiographically as small bone fragments near the site of ligament insertion. In partial injuries, with subluxation only, palpation over the volar plate and collateral ligaments can identify areas of injury. Dislocations are reduced with the aid of a digital block. If joint reduction does not occur easily, then further joint reduction maneuvers can be attempted with the aid of a portable fluoro-scanner. Multiple attempts at closed joint reduction should be avoided due to potential damage to the joint cartilage. In cases of irreducible dislocations, soft tissue interposition is usually preventing reduction and an open reduction in the operating room is indicated.
If the joint is amenable to closed reduction, the finger can then be assessed for tendon function and joint stability. Stability of the joint can be assessed passively by 1) laterally stressing the joint, 2) applying translational stress in a volar-dorsal direction, and 3) with active motion. Signs of subluxation or joint surface incongruity while the patient actively moves can be assessed in a fluoro-scanner. Joints that are stable throughout the full range of active motion are splinted or buddy taped for comfort for a few days, but can and should be mobilized early to prevent stiffness. Recurrent subluxation or dislocation with active motion necessitates splinting the joint in a position of stability to allow for ligament healing prior to mobilization.
Dorsal PIP Joint Dislocations
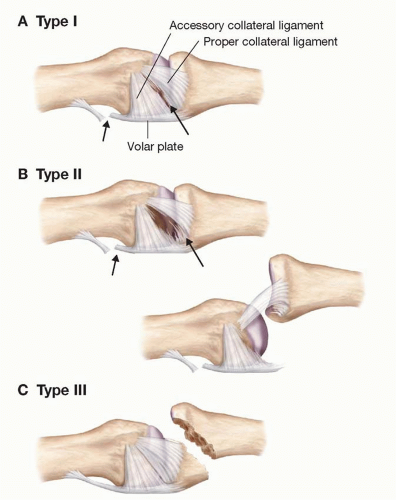
Dorsal dislocation or subluxation of the base of the middle phalanx is the most common PIP joint injury. The injury occurs as a result of hyperextension of the joint with axial loading. Dorsal PIP dislocations are classified into three types (Figure 81.2).1,2
Type 1(Hyperextension) injuries represent a hyperextension injury with an associated avulsion of the volar plate from the proximal phalanx. Although the degree of hyperextension may be dramatic, the articular surface of the middle phalanx remains in contact with the dorsal third of the proximal phalanx’s articular surface (Figure 81.2A).
Type 2 (Dorsal dislocation) injuries produce a complete longitudinal splitting of the collateral and accessory collateral ligaments and result in dorsal dislocation with incongruent joint surfaces and parallel phalanges in a bayonet configuration (Figure 81.2B).
Type 3 (Fracture dislocation) injuries result in an impaction fracture at the volar base of the middle phalanx, the fracture fragment remains attached to the volar plate, while the middle phalanx displaces dorsally. In acute injuries, deformity, swelling, and tenderness are frequently obvious; however, dedicated A-P and true lateral X-rays of the involved finger are essential and allow for the evaluation of subtle fractures or avulsed bone fragments. Fracture dislocations may either be stable or unstable based on the size and comminution of the fracture fragment. Stable fractures usually involve less than 30% to 40% of the volar articular surface of the middle phalanx. In cases of stable fracture dislocations, a portion of the proper collateral ligament remains attached to the middle phalanx, providing stability once the fracture is reduced. Unstable fractures usually involve more than 40% of volar articular surface of the middle phalanx. In these cases, the majority of the proper collateral ligament remains with the fracture fragment; thus, the middle phalanx has no remaining ligamentous support. Congruent reduction in such cases is unlikely and some means of fixation is required (Figure 81.2C).3
Treatment. Dorsal dislocations of the PIP joint are usually amenable to closed reduction by axial finger traction
under digital block anesthesia. Hyperextension of the PIP and gentle pressure applied to the dorsal base of the middle phalanx facilitate reduction. Difficulty reducing a dorsal dislocation should always raise the suspicion of soft tissue interposition between the joint surfaces and may necessitate open reduction. The volar plate is most commonly interposed, although interposition of the profundus tendon or a portion of the extensor mechanism is also possible. After reduction, the joint should be assessed for stability, and X-rays should be obtained to confirm the reduction and further assess for fractures.
under digital block anesthesia. Hyperextension of the PIP and gentle pressure applied to the dorsal base of the middle phalanx facilitate reduction. Difficulty reducing a dorsal dislocation should always raise the suspicion of soft tissue interposition between the joint surfaces and may necessitate open reduction. The volar plate is most commonly interposed, although interposition of the profundus tendon or a portion of the extensor mechanism is also possible. After reduction, the joint should be assessed for stability, and X-rays should be obtained to confirm the reduction and further assess for fractures.
Stable Joints
The majority of type 1 and type 2 injuries are stable after reduction and are treated nonoperatively with buddy-taping or extension block splinting. Simple hyperextension injuries, which are stable following reduction and without evidence of subluxation, can be splinted for comfort for 2 to 3 days and then patients may be started on active motion therapy protocols. Stable joints that have sustained more severe injuries (including congruent fracture dislocations that involve less than 40% of the articular surface of the middle phalanx) are placed in an extension block splint with the joint in 20° to 30° of flexion, which improves joint stability.2,4 Fluoroscopy is helpful in determining the angle to splint the joint to assure joint congruity in cases of fracture dislocations. The joint is allowed to flex within the splint. The splint is refashioned weekly to allow for gradual extension as the soft tissues heal. Alternatives to extension block splinting include extension block pinning which involves passing a K-wire into the head of the proximal phalanx to mechanically block PIP extension and prevent dorsal translation of the middle phalanx.5 Downsides of extension block pinning include the possibility of infection and the inability to gradually increase the amount of extension without removal of the pin. For stable dislocations, stiffness and swelling may persist for several months but long-term functional deficits are uncommon.
Unstable Joints and Fracture Dislocations
Intra-articular fractures and fracture dislocations that involve more than 30% to 40% of the articular surface leave little collateral ligament attached to the middle phalanx and are frequently unstable. These joints are much more prone to developing debilitating stiffness, contracture, and patient dissatisfaction. This type of injury is difficult to treat and complications may occur despite an optimally executed treatment regimen. The goals of treatment are to restore congruity at the articular surface and allow early active motion of the joint. There are several treatment options for unstable fracture dislocations and these include:
Dynamic skeletal traction—Longitudinal digital traction tightens the soft tissue envelope holding the bone fragments reduced (ligamentotaxis), and early range of motion can be initiated (Figure 81.3A-E).6
ORIF—Open reduction internal fixation using a lag screw can be performed through a volar approach if there is a single large volar fragment.
Trans-articular K-wire fixation—A single K-wire is passed proximally across the fracture site and into the head of the proximal phalanx with the joint in approximately 20° of flexion. The K-wire is removed after 3 weeks and the finger is mobilized,
4. Extension block splinting—Unstable PIP fracture dislocations tend to become more stable with an increasing degree of flexion. A dorsal splint can be used to block extension beyond the point of instability but allow for ongoing active flexion. The splint can be modified weekly to progressively decrease the degree of extension blocking. Extension blockade in greater than 30° of flexion for more than 3 weeks should be avoided, to minimize the risk of long-term PIP flexion contracture.4,7
Volar plate arthroplasty—When the articular surface of the middle phalanx is severely comminuted, restoration of stable congruent bone surfaces is difficult. Soft-tissue interposition arthroplasty using the volar plate to resurface the base of the middle phalanx can be used to restore joint function.8
Hemihamate osteochondral arthroplasty—For severe comminution of the middle phalanx, reconstruction of the volar portion of the middle phalanx is possible with the use of an osteochondral graft from the hamate. This procedure can be useful when there is >50% bone loss with instability. The dorsal central ridge of the hamate lies between the ring and small finger metacarpals and correlates nicely to the central ridge at the base of the middle phalanx. The graft is centered on this ridge and harvested slightly larger than the measured defect to allow for final contouring before inset. A volar approach to the PIP joint is used and the graft is secured with two or three bicortical screws. Early motion is begun at 1 week.9
Volar PIP Dislocation
Volar dislocation of the base of the middle phalanx is a rare injury and is usually associated with either 1) rupture of the central slip of the extensor tendon with or without an avulsion fracture of the base of the middle phalanx or 2) a torsional force causing rotatory subluxation of the middle phalanx volarly. Pure volar dislocations cause injuries to the collateral ligaments, volar plate, and extensor mechanism; however, the joint is easily reducible with longitudinal traction and extension of the middle phalanx. Rotatory volar dislocations usually result in disruption of only one of the collateral ligaments. As the associated side of the base of the middle phalanx subluxes in a volar direction, the corresponding proximal phalangeal condyle may buttonhole in the interval between the central slip and the lateral band, making reduction challenging. In such a situation, attempting reduction by longitudinal traction tightens the lateral band further entrapping the condyle. For these dislocations, reduction should be performed by placing the joint in full flexion, which relaxes the volarly displaced lateral band, and gentle rotation of the base of the middle phalanx. Radiographs are obtained to confirm success, and active extension is tested to assess the central slip stability. Failure to achieve full extension requires splinting in extension for 6 weeks; otherwise, the joint can be mobilized after 2 weeks. Inability to achieve closed reduction necessitates open exploration to reduce the entrapped condyle and repair the extensor mechanism. Small dorsal avulsion fractures can be immobilized in extension for 6 weeks. Larger, intra-articular dorsal fragments that are not comminuted are rare; however, ORIF should be considered if there is significant displacement.10
PIP Collateral Ligament Injuries
Forced lateral deviation of the PIP joint puts significant stress on the associated collateral ligament, which may rupture at its proximal attachment causing lateral joint instability. With more severe injury, the volar plate is also avulsed causing disruption of two sides of the ligamentous “box”; the middle phalanx dislocates laterally and should be reduced by longitudinal traction. Joint stability can be assessed by stressing the injured collateral ligament following reduction. Isolated collateral ligament injuries usually heal after a course of protection and immobilization in extension for 7 to 10 days, followed by controlled active motion. Buddy taping can be used to allow motion while protecting from further lateral stress injuries. Operative collateral ligament repair may be appropriate if the joint is irreducible or persistently unstable. In these circumstances, the ligament should be reattached through a midaxial approach using suture anchors.11,12,13
Outcomes and Complications.
Outcomes are predicated on appropriate reduction and early postoperative therapy. Type I injuries usually heal with few complications. Complete dorsal dislocations and fracture dislocations represent complete disruption of the volar plate and collateral ligaments and are associated with poorer outcomes. Collateral ligament fibrosis following dislocation is the most common complication, resulting in late joint stiffness and flexion contracture. For such cases, early therapy is the first-line treatment. If therapy fails to improve the stiff joint, consideration can be given to joint release, which can include total collateral ligament excision and volar plate release.
Other complications can include persistent volar plate laxity, which can lead to a hyperextension deformity (swan-neck) or early degenerative arthritis. In volar dislocations, extension lag can be troublesome even after repair of the central slip. Failure to identify central slip injuries in these patients will lead to chronic joint subluxation or a chronic boutonniere deformity.
DISTAL INTERPHALANGEAL JOINT
The distal interphalangeal (DIP) joint is also a uniaxial hinge joint and has an anatomic ligamentous structure similar to the PIP joint; however, additional volar support is provided by the profundus tendon insertion at the base of the distal phalanx. The checkrein ligaments are shorter and more laterally situated in comparison to the PIP joint which allows the joint to passively hyperextend by about 15°. The normal active motion arc is 0° to 60°, and restricted motion or fusion of the DIP joint is well tolerated. Dislocation of this joint is rare, and most cases are associated with concomitant flexor or extensor injury, and these will be discussed in greater detail in the section on extensor and flexor tendon injuries.
Dorsal DIP Dislocation
This is the most common DIP joint injury. Closed dislocations can be reduced by longitudinal traction and splinted for 2 to 3 weeks, with protected motion beginning at 1 week. The lack of soft tissue laxity often results in a dorsal skin laceration and an open joint, which should be irrigated, closed, and splinted. Rarely, DIP or thumb interphalangeal (IP) dislocations are irreducible due to interposition of the volar plate, flexor digitorum profundus (FDP) tendon, or even sesamoid bones and require open reduction. Hyperextension of the DIP joint can result in fracture of the volar lip of the distal phalanx. Small fragments proximal to the FDP insertion are usually inconsequential; fragments involving a large portion of the articular surface or the FDP insertion require operative fixation.14
METACARPOPHALANGEAL JOINT
Ligamentous injuries about the finger metacarpophalangeal (MP) joints are rare due to the significant amount of soft tissue stabilization around the metacarpal head. The MP joints are diarthrodial joints and are stabilized by a volar plate, as well as proper and accessory collateral ligaments. The MP joint has a complex articular geometry and extrinsic stabilizing structures that allow for stability in a multiplanar arc of motion. The metacarpal head is offset volarly from the shaft, which causes the collateral ligaments to tighten with increasing flexion. As such, the joint is lax in extension allowing for abduction and adduction when the hand is open. In flexion, the collateral ligaments are taut and joint stability is gained at the expense of lateral mobility. The volar plate is robust and cartilaginous distally, but thin and membranous proximally lacking checkrein ligaments and allowing for some hyperextension. Extrinsic stabilizers include the flexor tendons, the extensor mechanism, and the sagittal bands.15,16,17 Dislocations of the finger MP joints are usually dorsal or ulnar and occur most commonly in the index and small fingers. Volar dislocations and isolated collateral ligament injuries are rare.18
Dorsal MP Dislocation
Dorsal dislocation usually occurs as a result of forced MP hyperextension. Patients present with pain, deformity, and, usually, MP joint hyperextension. The diagnosis is confirmed radiographically. When the proximal phalanx is forced into hyperextension, the volar plate is torn proximally at its membranous portion. In a simple dorsal subluxation, there is often a marked hyperextension deformity of the finger; however by definition, the base of the proximal phalanx remains in contact with the metacarpal head; these injuries may be treated with closed reduction. In contrast, a complex dorsal dislocation occurs when the torn volar plate, which remains attached to the base of the proximal phalanx, becomes interposed in the joint. The finger assumes a bayonet position lying dorsally on the metacarpal head, and the deformity may be less impressive in appearance than a simple subluxation. The metacarpal head is forced into the palm and “buttonholes” between the
lumbrical radially, and the FDP tendon ulnarly. The flexor tendon is pulled dorsally by the intact A1 pulley and the structures form a noose around the narrow metacarpal neck. Attempts at closed reduction by hyperextension or traction tighten this noose, preventing relocation of the interposed volar plate and proximal phalanx.19 This mechanism should be considered even when attempting reduction of a simple dislocation, as digital traction causing excessive MP joint distraction can inadvertently draw the torn volar plate dorsally, thus converting a simple dislocation into a complex one requiring operative intervention. Closed reduction of a simple dislocation requires the wrist and PIP joints to be in flexion to relax the flexor tendons, and pressure is then directed over the base of the proximal phalanx volarly, sliding it over the metacarpal head, keeping the joint surfaces in contact to prevent inadvertent volar plate interposition.
lumbrical radially, and the FDP tendon ulnarly. The flexor tendon is pulled dorsally by the intact A1 pulley and the structures form a noose around the narrow metacarpal neck. Attempts at closed reduction by hyperextension or traction tighten this noose, preventing relocation of the interposed volar plate and proximal phalanx.19 This mechanism should be considered even when attempting reduction of a simple dislocation, as digital traction causing excessive MP joint distraction can inadvertently draw the torn volar plate dorsally, thus converting a simple dislocation into a complex one requiring operative intervention. Closed reduction of a simple dislocation requires the wrist and PIP joints to be in flexion to relax the flexor tendons, and pressure is then directed over the base of the proximal phalanx volarly, sliding it over the metacarpal head, keeping the joint surfaces in contact to prevent inadvertent volar plate interposition.
Complex, irreducible dislocations require open reduction. This can be approached through either a dorsal or volar incision.20 The dorsal approach carries a lower risk of injury to the neurovascular structures and allows direct visualization of the entrapped volar plate.21,22 The volar approach gives excellent access to the musculotendinous structures that entrap the metacarpal head, and reduction can be achieved by incising the A1 pulley, which allows the flexor tendon to return to its volar location by relaxing the noose around the metacarpal neck. In such cases, the neurovascular bundles will be placed on stretch and displaced superficially by the metacarpal head; the surgeon must be careful not to injure these structures during the skin incision and dissection to expose the joint.23 After reduction of simple or complex dislocations, a dorsal blocking splint should be applied to prevent recurrent hyperextension, and the reduction should be confirmed radiographically.
Volar MP Dislocation
Biomechanical studies in cadavers have shown that forced hyperflexion of the finger MP joints often results in a transverse proximal phalanx fracture rather than a volar MP dislocation; consequently, volar dislocation of the MP joint is an infrequent occurrence. Volar dislocations are usually irreducible due to interposition of the dorsal capsule, volar plate, juncturae tendinae, or collateral ligaments within the joint. Closed reduction may be attempted, but open reduction is usually required to remove the intervening structures prior to reduction.24
Isolated collateral ligament injuries at the MP joint are also rare, but may occur as a result of forced ulnar deviation at the MP joint and can be associated with a fracture of the base of the proximal phalanx. Injuries to the radial collateral ligament (RCL) of the index finger deserve special surgical consideration, as the integrity of this ligament is required to resist lateral deviation during pinch activities. If this injury is suspected, X-ray of the MP joint (Brewerton view) should be obtained to rule out avulsion fractures.25 Joint stability may be assessed by flexing the joint to 60° and placing a radial and ulnar lateral stress to the joint. Joints that are stable or have a firm endpoint on lateral stress testing can be splinted in 30° to 60° of flexion, and the patient may begin early active motion therapy. Such injuries may be expected to heal without surgical repair. Lack of a firm endpoint on lateral stress testing indicates a complete tear. Verification of such an injury can be performed with a magnetic resonance imaging (MRI). Unstable avulsion injuries are surgically repaired.26
LIGAMENT INJURIES OF THE THUMB
The thumb is capable of circumduction, opposition, flexion, extension, abduction, and adduction. The thumb contributes up to 40% of hand function, but due to its wide arc of motion, the thumb is at risk for hyperabduction and hyperextension injuries.27 The most common ligament injury occurring in the thumb is an acute tear of the MP ulnar collateral ligament (UCL), more commonly referred to as a “skier’s thumb.”
Thumb MP UCL Injury (Skier’s Thumb)
Acute tears of the UCL are 10 times more common than RCL injuries.28,29,30 The mechanism of injury is hyperabduction and forced radial deviation of the proximal phalanx during a fall. Patients will present with tenderness, swelling, and potentially bruising along the ulnar border of the thumb.
There are several important factors to determine when treating UCL injuries:
Is the injury a partial or complete ligamentous tear?
Is there a Stener lesion present?
Is there an associated fracture?
Is the injury acute or chronic?
Each of these factors will be discussed in greater detail below.
Physical Examination
The treatment of a UCL injury largely depends on whether the injury is a partial or complete ligament disruption. Partial tears (sprains) can be differentiated from complete tears on physical examination by assessing the degree of angulation on valgus stress testing, comparing this with the “normal” side, and evaluating for the presence of a “firm” endpoint. The differential attachment of the proper and accessory collateral ligaments normally allows the proper collateral ligaments to be taut in flexion and the accessory collateral ligaments to be taut in extension.
There is no consensus in the literature on how to clinically differentiate between partial and complete tears. However, if >35° of joint angulation is noted on valgus stress of the flexed MP joint, a complete tear of the proper collateral ligament is likely. In addition, if the degree of angulation with stress of the injured thumb exceeds that of the uninjured thumb by more than 15°, a complete tear is likely (Figure 81.4). Similarly, tears of the accessory collateral ligament can be identified when valgus stress testing of the extended MP joint results in more than 35° of radial deviation. Finally, the complete absence of resistance (“firm endpoint”) to lateral stress testing is also indicative of a complete UCL rupture. Pain and spasm of the injured adductor pollicis can confound the examination findings and a local anesthetic wrist block can be used to obtain a reliable examination. Partial tears are typically
stable and can be treated by immobilizing the MP joint for a minimum of 4 weeks in a thumb spica or hand-based splint, leaving the IP joint free.16,31,32,33
stable and can be treated by immobilizing the MP joint for a minimum of 4 weeks in a thumb spica or hand-based splint, leaving the IP joint free.16,31,32,33
Complete rupture of the UCL should be repaired to prevent long-term laxity and instability. The ligament usually tears at its distal attachment, although proximal and intra-substance tears have been reported. The surgical approach is through a lazy-S or chevron incision with the apex located at the volar, ulnar aspect of the MP joint. Mid-substance tears can be primarily repaired with nonabsorbable suture, and distal ligament avulsions should be securely fixed to the proximal phalanx using pullout sutures, bone anchors, or cerclage wire.34,35 In acute cases, the location of insertion on the proximal phalanx is apparent; however, in delayed cases, identifying the location of UCL attachment may be difficult. In these cases, the ligament should be reattached 3 mm distal to the articular surface and 3 mm dorsal to the volar cortex of the proximal phalanx to optimize MP range of motion.36
The Stener Lesion
Complete avulsion of the UCL from its distal attachment can result in interposition of the leading edge of the adductor aponeurosis between the ligament and its insertion (the Stener Lesion).28,37,38 Without operative reduction and fixation, soft tissue interposition will prevent the ligament from healing and the thumb will be chronically unstable. Occasionally, a small bone fragment is avulsed with the ligament and can be seen proximal to the adductor hood on radiograph. In the absence of a bone fragment, the diagnosis is largely a clinical one based on findings of a complete UCL tear with a palpable mass proximal to the MP joint. MRI or ultrasound can confirm the diagnosis.39,40
UCL Avulsion Fractures
X-rays are always obtained because avulsion fractures of the proximal phalanx are common. The majority of these fractures do not have a Stener lesion present, and primary bony healing is possible in minimally displaced fractures with immobilization. Combination injuries (avulsion fracture and ligament injury) can occur, though much less frequently.41 Due to the possibility of these combined injuries, MRI is recommended for open reduction and fixation to verify that the ligament is not injured. Indications for open reduction and internal fixation of avulsion fractures include:
Involvement of 20% or greater of the joint surface
Significant fracture displacement (>2 mm)
Significant instability with UCL testing
Presence of a bony Stener lesion
Combination injuries (avulsion fracture and ligament injury)
Minimally displaced fractures that are stable on stress testing can be immobilized in a thumb spica splint for 4 weeks, with a further 2 weeks of protected active motion.36
Chronic UCL Injuries (Gamekeeper’s Thumb)
The “gamekeeper’s thumb” refers to chronic symptomatic UCL laxity. It was originally described in a series of Scottish gamekeepers whose injury was a result of repetitively stressing the UCL as they fractured the necks of rabbits between the thumb and the index finger. This type of cyclical attenuation of the ligament can lead to symptomatic chronic UCL pain and laxity, although inadequate treatment of an acute tear or failure to recognize a Stener lesion are probably more common etiologies of chronic UCL symptoms.
Reconstruction of chronic UCL injuries can be achieved using either dynamic or static procedures. Dynamic procedures involve transferring the insertion of a musculotendinous unit (e.g., adductor pollicis or extensor pollicis brevis [EPB]) to the base of the proximal phalanx, stabilizing the MP joint by pulling the phalanx in an ulnar direction.42 Static procedures involve using free tendon grafts to reconstruct the proper and accessory collateral ligaments through bone tunnels.2,43 Satisfactory results have been reported with secondary ligament reconstruction; however, at the time of surgery the surgeon should still evaluate the mobility of the UCL because some surgeons have found that even after 2 years from the time of injury, the UCL can be dissected from the surrounding scar tissue and repaired to its original point of insertion.44 Contraindications to ligament repair or reconstruction includes evidence of MP joint arthritis, which can develop in cases of long-standing UCL instability. In such cases, MP fusion should be recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree