Chapter 11
Leg Ulcers
OVERVIEW
- The underlying cause of most ulcers is inadequate blood perfusion of the skin.
- The majority of leg ulcers arise due to oedema and raised pressure in the intercellular space, preventing capillary perfusion and causing back pressure in the venules.
- Risk factors for venous ulceration include increasing age, immobility, obesity, lower leg trauma, oedema, varicose veins and thrombosis.
- Risk factors for arterial ulcers include hypertension, atherosclerosis, peripheral vascular disease, polycythaemia, cryoglobulinaemia, vasculitis and connective tissue disease.
- Clinical features of venous ulcers: most commonly over medial malleolus; pitting oedema, dilated tortuous veins; ulcers have a well-defined, sloping edge and central slough.
- Clinical features of arterial ulcers: most commonly over shins, dorsal foot; painful, pale hairless legs, poor peripheral pulses, ulcers sharply defined with ‘punched-out’ edge.
- Management: correction of underlying cause if possible, clean ulcers, application of non-adherent dressings and appropriate compression bandages.
Introduction
The prevalence of leg ulceration is estimated to be between 0.3% and 1.0% of the general population, rising to 2% of those over the age of 80 years; however, with rising rates of obesity the incidence is expected to rise. Leg ulcers cause significant morbidity for those affected and the cost to the National Health Service in the UK is estimated to be £400 million per annum. Many patients have recurrent ulceration requiring repeated courses of bandages and dressings; 80% of patients are treated in the community. If the underlying cause of ulceration cannot be relieved by an operation or medical intervention, then the key worker will often be the specialist nurse who has considerable experience in assessing and facilitating the healing of difficult chronic ulcers.
Assessment of any ulcer should include consideration of the following parameters: site, size, edge, base, surrounding skin, leg shape, duration, symptoms, underlying systemic/cutaneous diseases, peripheral pulses/sensation, medication, and current and past ulcer treatments. Investigations may include ankle: brachial pressure indices (ABPI), venous and/or arterial duplex scanning, microbiology swabs, ulcer biopsy (usually through the edge) and patch testing.
A basic understanding of the underlying principles of ulceration is essential in reaching a clinical diagnosis and appreciating the different approaches to management. Most (95%) of ulcers are ‘venous’ (stasis) in nature (Figure 11.1) and therefore these are considered first in some detail.

Figure 11.1 Venous leg ulcer.
Venous ulcers
Pathology
The skin
Ulcers arise because the skin (epidermis and dermis) dies from inadequate provision of nutrients and oxygen. This occurs as a consequence of (a) oedema in the subcutaneous tissues with poor lymphatic and capillary drainage and (b) the extravascular accumulation of fibrinous material that has leaked from the blood vessels. The result is a rigid cuff around the capillaries, which prevents diffusion of oxygen and nutrients through the vessel wall into the surrounding tissues with consequent fibrosis.
The blood vessels
Arterial perfusion of the leg is usually normal or increased, but stasis occurs in the venules. The lack of venous drainage is a consequence of incompetent valves between the superficial veins and the deeper large veins on which the calf muscle ‘pump’ acts. In the normal leg, there is a superficial low-pressure venous system and deep high-pressure veins (Figures 11.2 and 11.3). If the blood flow from superficial to deep veins is reversed, then the pressure in the superficial veins may increase to a level that prevents venous drainage (Figure 11.4). The resulting back pressure leads to varicose veins with stasis and oedema; consequently, there is diminished blood flow to the skin, causing ulceration. Chronic venous insufficiency and the resulting venous hypertension cause venous ulcers.
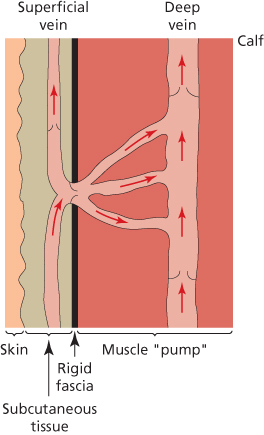
Figure 11.2 Healthy valves in legs.
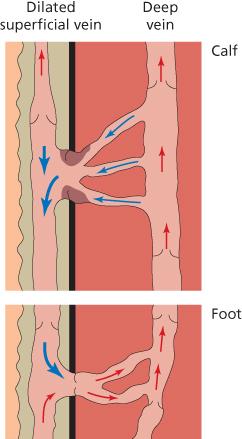
Figure 11.3 Incompetent valves in legs.

Figure 11.4 Varicose veins.
Incompetent valves
Incompetent valves leading to gravitational ulcers may be preceded by:
- Deep vein thrombosis (DVT) associated with pregnancy, injury, immobilisation or infarction.
- Primary long saphenous vein insufficiency.
- Familial venous valve incompetence that presents at an earlier age (approximately 50% of patients).
- Deep venous obstruction.
Risk factors for venous ulceration
Women are more at risk than men. Other risk factors are a family history of venous disease, increasing age, immobility, obesity, lower leg trauma, peripheral oedema, DVT, varicose veins and a previous history of venous leg ulceration. Patients may develop severe venous eczema prior to ulceration (Figure 11.5), which, if treated early and effectively, can prevent ulceration.

Figure 11.5 Varicose eczema.
Clinical features
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree