Latissimus Flap
Peter Henderson
Joseph J. Disa
DEFINITION
The principal reason to undergo a latissimus dorsi (LD) myocutaneous flap for breast reconstruction is to recruit healthy skin to replace lost breast skin. The volume of subcutaneous tissue is often insufficient to adequately replace the breast mound. In this case, the most common approach is to place tissue expanders (TEs) at the time of the LD flap, followed by expansion and ultimately exchange for permanent implants at a later date (but in the appropriately selected patient, breast reconstruction can be performed in a single stage, with the permanent implants placed at the time of the LD flap).1
LD flap breast reconstruction without placement of any sort of prosthetic device (TEs or permanent implants) would be done in one of three scenarios:
First, if the patient’s build is so thin that minimal breast mound is needed in order to provide the desired breast projection
Second, if the patient is obese and has a large amount of fat in the four fat compartments of the back, as described for the low transverse extended LD flap concept by Bailey et al. (parascapular fold, lumbothoracic fold, lumbar fold, or suprailiac ford).
Third, if the decision has been made that there will be no attempt to recreate any appreciable breast mound at the current time (if the patient’s preferences change in the future change, a prosthetic device could be placed at a subsequent operation). In the case of this reason, the LD flap would be best thought of as a means of providing soft tissue coverage for chest wounds and not of actual “breast reconstruction,” per se.
ANATOMY
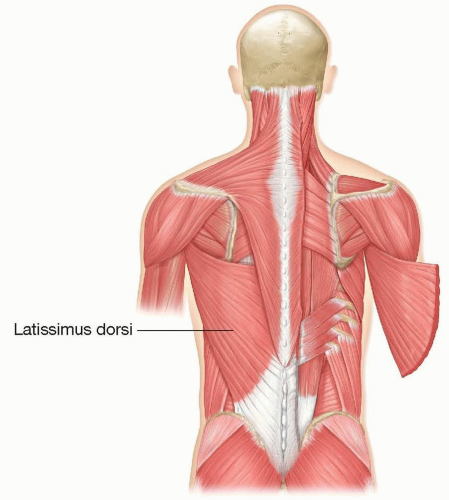
The LD is a Mathes-Nahai type V muscle. The dominant pedicle is the thoracodorsal artery and vein (off the subscapular artery and vein), and multiple secondary pedicles arise from the lumbar vessels (FIG 1).
The origins of the muscle are the spinous processes of T7-T12, the thoracolumbar fascia, the iliac crest, the inferior angle of the scapula, and ribs 9 to 12.
The insertion is the floor of the intertubercular or bicipital groove of the humerus.
The innervation is the thoracodorsal nerve (off the posterior cord of the brachial plexus).
The function of the LD is to adduct, extend, and internally rotate the ipsilateral arm.
PATHOGENESIS
The indication for the LD myocutaneous flap is most commonly breast skin loss due to ischemia (particularly following skin-sparing or nipple-sparing mastectomy) and/or radiation-induced injury.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient’s breast history (prior procedures as well as adjuvant or neoadjuvant therapy) should be elicited to understand the timing and expected progression of the sequelae.
If TEs are in place, it is important to understand if tissue expansion is complete or if it is still under way.
Physical examination should focus on assessing the surface area of skin needed, and the volume of breast mound needed.
The back should be examined for thickness/volume of the skin and subcutaneous tissue, as well as any prior incisions.
IMAGING
No imaging is necessary for preoperative planning.
If necessary, appropriate surveillance for breast disease (mammography, MRI, etc.) should be performed.
NONOPERATIVE MANAGEMENT
If TE is in place and skin necrosis has occurred in the absence of infection or exposure of the TE, one approach is to continue expansion—in fact overexpansion—in order to excise and perform primary closure at the time of exchange, which obviates the need for recruitment of additional skin.
SURGICAL MANAGEMENT
Preoperative Planning
If breast TE will be used, it is chosen based on base diameter and then desired projection.
If permanent implants are to be used, they must be chosen prior to the procedure. Important variables are fill substance, size, shape, and texture. This should be a joint decision-making process between the patient and the reconstructive surgeon.
The fill substance can be either saline or silicone (the outer shell is made of silicone in both cases). Saline has a less “natural” feel, but no surveillance is recommended; if rupture were to occur, it would be readily apparent, and saline is assuredly medically inert. Silicone has a more “natural” feel, though it is recommended to have a regular MRI surveillance imaging to evaluate for the possibility of rupture.
The most important variable in choosing the size of the implant is the base diameter (there is a decreasing emphasis on the volume, as it is a variable that can change based on the shape of the device).
The shape can be either round or anatomic (“form stable” or “gummy bear”). Anatomic implants were designed, in theory, to give more of a natural appearance. Round implants have greater upper pole projection and may not look as “natural” and instead have an “augmented” look, which may be desirable to some patients.
Positioning
Positioning is one of the greatest challenges of performing the LD flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree