I. OVERVIEW
A. Laser is an acronym for light amplification by stimulated emission of
B. All lasers have four essential parts
1. A medium (gas, liquid, or solid) that can be excited by stimulated emission.
2. Power supply or a source of energy to excite the medium
3. Mirrors for amplification
4. Delivery system to deliver light to target
C. Laser light has three unique properties
1. Monochromaticity: Emission of single wavelength or narrow band of wavelengths
2. Coherence: Light waves are in phase temporally and spatially.
3. Collimation: Light waves travel in parallel without spreading even over long distances.
D. Lasers can be delivered in three modes
1. Continuous mode: A constant, uninterrupted beam. (Example: Argon lasers)
2. Pulsed mode: Single or train of pulses
3. Q-switched mode: Very short pulses at high peak power.
E. There are four outcomes when laser light hits the skin
1. Reflection: No biological effect
2. Scattering: Incoming beam is spread in all directions.
3. Transmission: Light passes through tissue unaltered.
4. Absorption: Light hits appropriate target (chromophore). Light is transformed into heat by interaction with tissue.
F. Theory of selective photothermolysis.
1. Energy of a specific wavelength is absorbed by a chromophore in tissue. Major chromophores in the skin are melanin, hemoglobin, and water.
2. The time of laser exposure (pulse duration) is just shorter than the cooling time (thermal relaxation time) of the chromophore.
a. Thermal relaxation time is the time required for the heated tissue to lose half of its heat.
b. If a pulse duration is longer than the thermal relaxation time, heat is not confined to target structure and can damage the surrounding tissues.
G. Key parameters
1. Wavelength
a. Fixed and depends on the specific laser selected.
b. Lasers are selected based on the indication and target chromophore (e.g., pigment, water, melanin, hemoglobin).
i. Chromophores absorb the light, and heat is produced in order to create the clinical effect.
a) If no heat is produced, no clinical effect.
b) If excess heat is produced, scarring can result from thermal injury.
ii. Example: Darker skin has a greater amount of melanin and greater chromophore concentration. Therefore, it is more likely to generate heat and thermal damage with laser therapy compared with lighter skin tones.
______________
*Denotes common in-service examination topics
a. The amount of energy produced by the laser (J/cm2).
b. Selected by the practitioner
3. Pulse duration
a. How long the tissue is exposed to the laser.
b. Should be equal to or less than the thermal relaxation time.
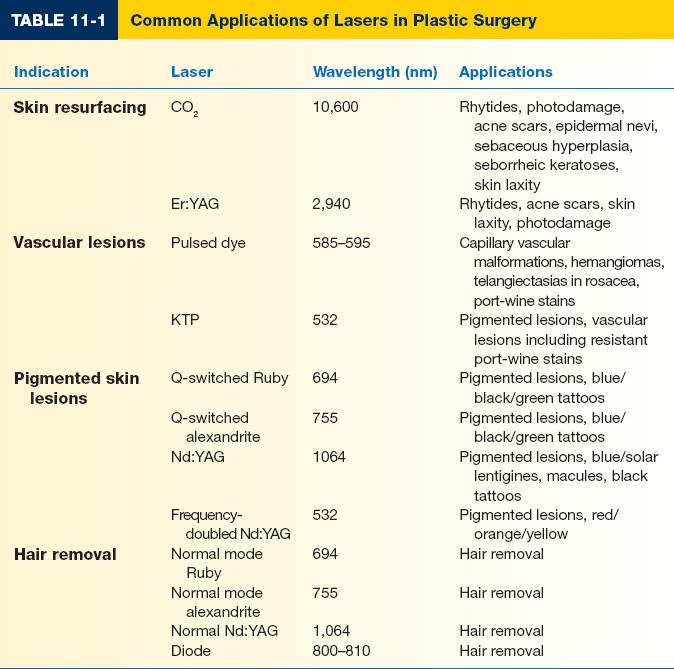
II. LASER APPLICATIONS (TABLE 11-1)
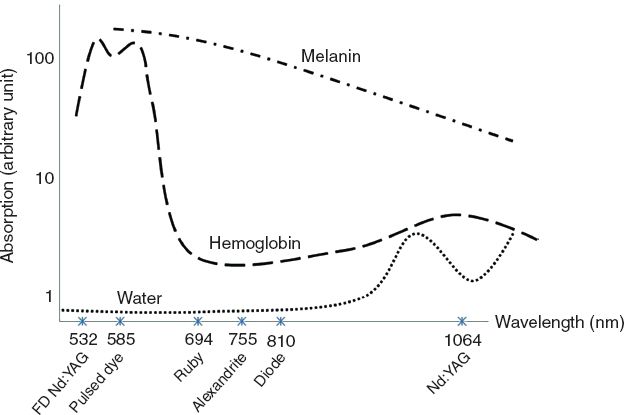
A. The three main chromophores of the skin are water, hemoglobin, and melanin, and laser therapy is directed toward these targets (Fig. 11-1).
B. Skin resurfacing
1. Can improve fine-to-medium wrinkles in patients with Fitzpatrick I or II skin (e.g., perioral rhytids) due to skin contraction from collagen contraction and increased deposition and reorganization of collagen and elastin.
a. Results in thermal injury to the skin with wound healing.
b. Reepithelialization occurs through proliferation of progenitor cells within hair follicles and sweat glands.
c. Increased dermal collagen synthesis for 3 to 6 months.
d. Reorganization of elastic fibers into a parallel and tight configuration.
2. Contraindications
a. Relative: Smoking, previous resurfacing, diabetes, prior skin irradiation, active acne, hypertrophic scarring, skin hypersensitivity, vitligo, and pigmentation disorders.
Figure 11-1. Wavelength depth of commonly used lasers. (Adapted from DiBernardo BE, Cacciarelli A. Cutaneous lasers. Clin Plast Surg. 2005;32:141–150.)
b. Absolute: Keloids, scleroderma, systemic lupus erythematosus, and isotretinoin use within the previous year.
3. Prophylaxis: *Valacyclovir or other similar antivirals for HSV prophylaxis for all patients.
4. CO2 laser: Ablative
a. Wavelength: 10,600 nm
b. Medium: Gas
c. Chromophore: Water
d. Pulsed or continuous wave modes
e. Water absorbs energy, converting light to heat which vaporizes or ablates tissue
f. Ablation threshold—the necessary amount of energy that achieves tissue vaporization. Ablation threshold for CO2 laser is 5 J/cm2.
g. Side effects
i. Long healing times
ii. Long period of erythema (weeks to months)
iii. Temporary hyperpigmentation
iv. Possible yeast, bacterial, viral infections
v. Contact dermatitis
vi. Risk of permanent hypopigmentation (infrequent)
vii. Risk of scarring (infrequent)
h. Indications: Photoaged skin, rhytids, acne scars, skin laxity, hypertrophic burn scars, some linear epidermal nevi, sebaceous hyperplasia, and seborrheic keratoses.
i. Relative contraindications: Vitiligo, scleroderma, darker skin, unrealistic expectations.
j. Best candidate: Fitzpatrick type I or II skin.
k. Effects are similar to a controlled partial-thickness burn.
l. Fractional setting decreases amount of thermal injury but still stimulates tissue regeneration.
5. Erbium:yttrium–aluminum–garnet (Er:YAG)
a. Compared with the CO2 laser, more passes are required for the same depth of penetration, but with less thermal damage.
c. Medium: Solid
d. Chromophore: Water
e. Ablation threshold for Er:YAG laser is 1.6 J/cm2.
f. Side effects
i. Long healing times
ii. Long period of erythema (weeks to months)
iii. Temporary hyperpigmentation
iv. Possible yeast, bacterial, viral infections
v. Contact dermatitis
vi. Risk of permanent hypopigmentation (infrequent)
vii. Risk of scarring (infrequent)
g. Indications: Rhytids, photodamage, acne scars, skin laxity
h. Best candidate: Fitzpatrick type I or II skin
C. Vascular lesions
1. Most commonly indicated for capillary malformations.
2. Selective photothermolysis targets hemoglobin and oxyhemoglobin molecules in order to shrink or eliminate blood vessels.
3. Argon laser
a. Wavelength: 418 and 514 nm
b. Medium: Gas
c. Chromophores: Oxyhemoglobin and melanin
d. Painful for patient
e. Very popular choice in the 1980s for treatment of capillary malformations but now rarely used due to side effects
f. Side effects
i. Weeping, crusting, blistering after treatment
ii. Textural changes
iii. Hypertrophic scarring
iv. Pigmentary changes
4. KTP (potassium–titanyl–phosphate) laser
a. This laser is a long-pulsed, frequency-doubled Nd:YAG laser
b. Wavelength: 532 nm
c. Medium: Solid
d. Chromophore: Hemoglobin and melanin
e. For thicker pigmented lesions and vascular lesions. May have a role in resistant port-wine stains.
f. Similar response rates as pulsed dye laser (PDL) for some indications but main advantage over PDL is that purpura rarely occurs—but scarring has been reported
g. Consider for resistant port-wine stain and large venous malformation
5. Flashlamp Pulsed Dye Laser
a. *Wavelength: 585 or 595 nm
b. Medium: Liquid (dye)
c. Chromophore: Oxyhemoglobin
d. Used to treat capillary vascular malformations, hemangiomas, telangiectases in rosacea, port-wine stains.
e. Side effects: Erythema/purpura for 7 to 14 days, hyperpigmentation, hypopigmentation.
f. Usually requires several treatments for lightening of vascular lesions.
g. Best results for port-wine stains depends on location and size.
i. Port-wine stains on the face and neck respond better than those on the leg and hand.
ii. On the face, port-wine stains on forehead and lateral face respond better than those on the middle of face.
iii. Chest, upper arm, and shoulder respond well
iv. Port-wine stain less than 20 cm2 at initial examination cleared more than those larger than 20 cm2.
D. Pigmented skin lesions
1. Common pigmented skin lesions amenable to laser treatment: lentigines, ephelides, café au lait macules, thin seborrheic keratoses, nevus of Ota, nevus of Ito, blue nevi.
2. May require multiple treatments, especially for lesions such as café au lait macules, nevus of Ota, nevus of Ito.
3. Treatment of melanocytic nevi is controversial and should be undertaken carefully because of concern for undiagnosed dysplasia and melanoma being inadvertently treated and slowing diagnosis. As a result, diagnosis should be ascertained prior to treatment.
4. Chromophore: Melanin
5. Although continuous wave lasers have been used in the past such as copper vapor or copper bromide, Q-switched lasers are now the treatment of choice for pigmented lesions.
a. Q-switched ruby laser: 694 nm
b. Q-switched alexandrite: 755 nm
c. Q-switched Nd:YAG: 1,064 nm; use for patients with darker skin because of decreased risk of dyspigmentation
6. Complications: Pigmentary changes (hypopigmentation or hyperpigmentation), partial removal, infection, bleeding, textural changes, scarring (< 5%)
E. Tattoo removal
1. Lasers in Q-switched mode are used for tattoo removal.
2. Chromophore: Tattoo pigment
3. Three types of lasers are currently used for tattoo removal.
a. Q-switched ruby: 694 nm
i. Useful for black, blue, and green pigments
ii. Can remove all colors except red and orange
b. Q-switched alexandrite: 755 nm
i. Useful for black, blue, and green pigment
ii. Can remove all colors except red and orange
c. *Q-switched Nd:YAG: 532 nm
i. Useful for red pigment
d. *Q-switched Nd:YAG: 1,064 nm
i. Useful for black and blue pigments
4. Absorption peak of pigment must match wavelength of laser, which heats the tattoo particles leading to fragmentation. Phagocytes remove fragments.
5. Multiple treatments are necessary with treatments separated by 5 to 10 weeks. Complete clearance may not be achieved.
6. Tattoos absorb in the following ranges
a. Red tattoos—505 to 560 nm
b. Green tattoos—630 to 730 nm
c. Blue green tattoos—400 to 450 nm and 505 to 560 nm
d. Yellow tattoos—410 to 510 nm
e. Purple tattoos—550 to 640 nm
f. Blue tattoos—620 to 730 nm
g. Orange tattoos—500 to 525 nm
h. Black and gray tattoos—600 to 800 nm
7. Practice care with cosmetic tattoos (e.g., tattooed lip liner) because oxidation of certain tattoo pigments (such as ferric oxide and titanium oxide) with laser therapy may lead to darkening instead of lightening.
8. Complications: Pigmentary changes (hypopigmentation or hyperpigmentation), partial removal, infection, bleeding, textural changes, tattoo ink darkening, scarring (< 5%)
1. Numerous lasers targeting unwanted hair include diode laser (800 to 810 nm), normal mode ruby (694 nm), alexandrite (755 nm), and normal Nd:YAG (1,320 nm).
2. *Chromophore: Melanin
3. Using lasers with longer pulse duration achieves two goals.
a. Epidermal melanosomes are not affected.
b. The light-absorbing melanized bulb and shaft diffuses heat to surrounding follicle.
4. Lasers with higher fluences have better results for hair removal but higher fluences lead to higher discomfort and complication risks.
5. Requires multiple treatments.
6. All lasers lead to hair reduction, not permanent hair removal.
7. Ideal patients have dark hair and fair skin. The treatment of light or white hairs remains a challenge.
G. Fractional photothermolysis
1. Only a portion of the epidermis and dermis is treated with columns of energy in order to create targeted areas of thermal damage (microthermal treatment zones [MTZs]).
2. The untreated areas are a reservoir of collagen and promote tissue regrowth.
3. Allows for greater penetration with decreased risk of scarring.
4. Pattern density
a. Number of MTZs within the treatment area.
b. Greater number of MTZs yields a greater surface of the skin treated at each pass.
5. Energy
a. Depth of MTZ penetration into the dermis.
6. Nonablative fractional devices
a. Erbium-doped laser (1,550 nm)
b. Skin resurfacing, acne, striae, scarring, melisma, burn scars
c. Can be performed under topical anesthetic
d. Mild erythema and swelling for 2 days is most common. Can also result in facial edema, dry skin, flaking, superficial scratches, pruritus, pigmentary changes, and an acneiform eruption.
e. Risk of herpes simplex virus and varicella zoster virus reactivation.
7. Ablative fractional devices
a. Ablative CO2 or erbium lasers
b. Fine rhytids, dyspigmentation, skin laxity
c. Can be performed under topical anesthetic with nerve block.
d. May result in prolonged erythema, hypopigmentation, and scarring, although the risks are less compared with fully ablative therapy.
III. LASER SAFETY
A. Signs
1. Signs on room door should have information about laser, its wavelength, and energy.
2. A pair of appropriate eyewear placed on the door outside the room.
B. Eye protection
1. CO2 and Er:YAG lasers can injure cornea.
2. PDL and ruby lasers can injure retina.
3. Special glasses that match the emission spectrum of a laser must be worn by laser operator and other personnel in the room.
4. Manufacturer of protective eyewear has the wavelengths of light for which protection is provided printed on goggles.
5. Patient can wear
a. Metal corneal eye shields if laser will be used around orbits.
b. Burnished stainless steel eye cups.
1. Prep solution should be nonflammable (avoid chlorhexidine or alcohol).
2. Surround the area to be treated with wet towels.
D. Laser plume
1. Ablative lasers create a plume.
2. Laser plume may contain bacteria and HPV.
3. Laser operator and personnel should wear surgical masks.
4. Use a smoke evacuator close to the site of procedure.
PEARLS
1. Vascular lesions are most effectively treated using PDLs (585 to 595 nm)
2. Tattoos can be effectively treated with Q-switched lasers, and the appropriate wavelength depends on the color and depth of the pigment
3. Fractional technologies are increasingly popular for skin rejuvenation and resurfacing, and only treat a portion of the skin surface. These techniques can potentially minimize patient side effects and complications.
QUESTIONS YOU WILL BE ASKED
1. What are the common complications of laser therapy?
Hypopigmentation, hyperpigmentation, HSV flare, and scarring.
2. What medication(s) should all patients undergoing cutaneous laser resurfacing receive as prophylaxis?
Valacyclovir
3. Which skin types are at greatest risk for side effects or complications following laser therapy?
Fitzpatrick IV and above
Recommended Readings
Alster TS, Lupton JR. Prevention and treatment of side effects and complications of cutaneous laser resurfacing. Plast Reconstr Surg. 2002;109(1):308–316. PMID: 11786830.
Chim H, Drolet B, Duffy K, Koshima I, Gosain AK. Vascular anomalies and lymphedema. Plast Reconstr Surg. 2010;126(2):55e–69e. PMID: 20679788.
DiBernardo BE, Cacciarelli A. Cutaneous lasers. Clin Plast Surg. 2005;32:141–150. PMID: 15814112.
Nelson AA, Lask GP. Principles and practice of cutaneous laser and light therapy. Clin Plast Surg. 2011;38:427–436. PMID: 21824540.
Wu EC, Wong BJ. Lasers and optical technologies in facial plastic surgery. Arch Facial Plast Surg. 2008;10(6):381–390. PMID: 19018058.
< div class='tao-gold-member'>