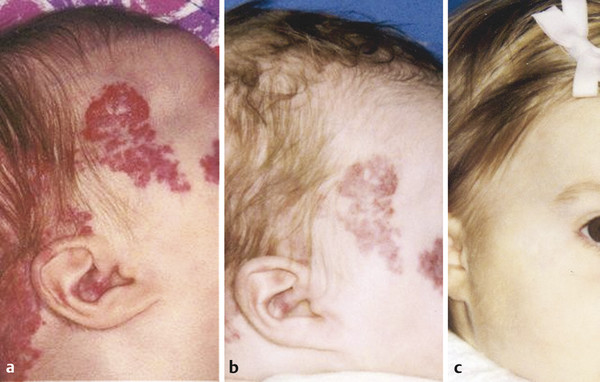
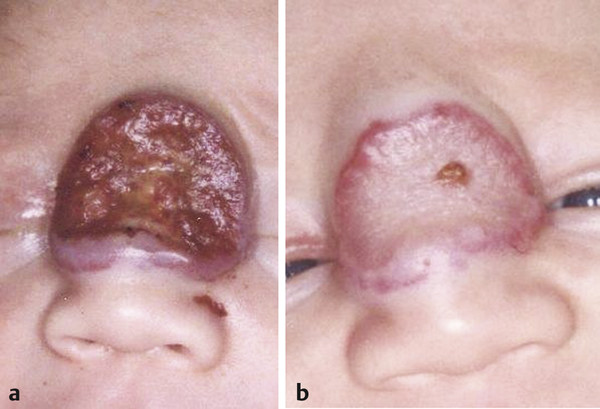
The concept of selective photothermolysis by laser energy is detailed throughout this book and applies to treatment of vascular lesions as well. The target chromophore in the vascular lesion is oxyhemoglobin, with absorption peaks at 18, 542, and 577 nm. The thermal relaxation time is the cooling time of oxyhemoglobin and is proportional to the vessel diameter squared. By keeping the pulse duration equal to or less than the thermal relaxation time, thermal injury to the surrounding tissues is minimized. Devices with adjustable pulse durations allow for treatment of vessels of different sizes. Melanin has a broad absorption spectrum (250–1,200 nm) that unfortunately overlaps the peaks of oxyhemoglobin. This makes it difficult to treat vascular lesions in dark-skinned or tan individuals and needs to be taken into account in the parameters used. In addition, in order to see continued improvement in some anomalies, it is often necessary to employ high energy levels that exceed the calculation of the thermal relaxation time for blood vessels. In order to address this problem and the problem of heat accumulation by the energy absorption of melanin, cooling mechanisms have been added to the laser devices. By simultaneously cooling the skin before, during, and after the laser pulse, the unwanted heat accumulation is minimized and, additionally, patient comfort is increased. Laser spot size is another determinant of laser depth penetration. Larger spot sizes allow for greater penetration of larger fluences (energy per unit area, J/cm2). Thus devices with adjustable spot sizes allow for treatment of vessels at different depths. The dynamic cooling devices increase the safety of using larger spot sizes. The introduction of the pulsed dye laser (PDL) in 1989 revolutionized the treatment of vascular lesions and anomalies and has since been the gold standard. The first-generation PDL emitted laser light at 577 nm, coinciding with the last peak of oxyhemoglobin. Currently available PDLs emit a wavelength of 585 or 595 nm with longer pulse durations. The longer wavelengths and pulse durations allow for greater depth penetration but require higher fluences to compensate for lower absorption beyond 585 nm. Again, the dynamic cooling devices allow for safe-guarding the epidermis under these conditions. Despite being a major advancement, the PDL is still limited in the size of vessels it can coagulate and the depth of penetration of the beam. The therapeutically effective depth of penetration is estimated to be 0.07 mm from the epidermal-dermal junction with poor coagulation beyond 1.16 mm. The vessel size and depth of vessels may be an explanation for the resistance of port-wine stains (PWS, capillary malformations) to treatment and/or incomplete clearance despite multiple PDL procedures. The same can be said for decreased effectiveness in treating proliferating superficial infantile hemangiomas or the superficial component of compound hemangiomas greater than 3 mm in thickness. Thus it is common for several devices to be used during an extended treatment protocol to address the heterogeneity in vessel size and depth within the vascular lesion. Therapy is first initiated with shorter wavelengths and pulses to target the typical small-diameter (30–50 µm) vessels. Thereafter, longer wavelengths and pulses can be used to target the larger and deeper blood vessels. Laser systems with longer wavelengths currently used for treatment of vascular lesions are the neodymium:yttrium aluminum garnet (Nd:YAG) (1,064 nm) and long-pulsed alexandrite (755 nm). Although not a longer wavelength, the frequency-doubled, potassium titanyl phosphate (KTP) (532 nm) can also be used. The Nd:YAG, a continuous wave infrared laser (1,064 nm), is not ideal for treating cutaneous vascular lesions due to deep penetration (4–6 mm) and preferential damage to arteries rather than veins. Thermal injury of these deeper vessels may lead to dermal necrosis with increased risk of scarring. This higher risk is thought to be due to partial conversion of oxyhemoglobin to methemoglobin causing a very steep fluenceresponse curve leading to rapid skin temperature and purpuric changes. The Nd:YAG laser induces shrinkage of vascular lesions by nonspecific thermal damage so it is used primarily for deeper (not cutaneous) lesions such as venous malformations. Delivery of the wavelength transmucosally or interstitially through a bare quartz fiber via a puncture, however, are useful techniques. The long-pulsed alexandrite has selective absorption of deoxyhemoglobin and 50 to 75% deeper tissue penetration than PDL. The 755-nm wavelength may be used alone or in combination with PDL for improved efficacy of treatment-resistant PWS or hypertrophic lesions without an increase in complications. Permanent hair reduction is a potential side effect of which patients must be warned. The 532-nm KTP laser emits green light near the 542-nm hemoglobin absorption peak but is absorbed by melanin more than the PDL, which may lead to higher rates of scarring and dyspigmentation. However, at low fluences and longer pulses of 10 to 50 ms, superficial facial vessels respond very well with little morbidity. Infantile hemangiomas (IHs) are the most common benign tumors of infancy. They have a peculiar, extensively reviewed2,3 natural history characterized by rapid postnatal proliferation of the tumor followed by variable involution. IHs are classified by degree of involvement of the dermis, with superficial IHs involving the upper layers, deep IHs the lower dermis, and compound IHs (▶ Fig. 12.1) having both a superficial and deep component. Multimodality therapy is the norm and involves combinations of observation, laser treatment, medical therapy, and/or surgery. The role of laser therapy can be to effect total resolution of the macular proliferative lesion, retard the proliferation, and/or treat the superficial residuum of involution. Given the excellent safety profile and selectivity of its wavelength, the PDL is the treatment of choice for the superficial component of proliferating and involuting IHs in these children. As discussed, depth of penetration of the 585-nm wavelength is limited; therefore, it is most effective in treating the superficial component that is < 3 mm in thickness. It has been shown to achieve > 95% reduction in proliferating thin lesions after four treatments (7 mm spot size, 1.5–3 ms pulse duration, and up to 10 J/cm2) spaced 1 month apart versus 85% reduction in color with little change in thickness with the same parameters in those > 3mm in thickness. So, the PDL has more of a chance of penetrating the entirety of the lesion leading to photocoagulation, cell death, and clearance―the thinner the superficial component. Treatment of thicker lesions leads to reduction in the color but not necessarily in the volume. The PDL, or any interstitial delivery of laser energy, has no proven role in the treatment of the deep component of focal, deep, or compound IHs.4 Fig. 12.1 Compound proliferating infantile hemangioma (IH) (a) before, (b) during, and (c) after treatment of the superficial component with the pulsed dye laser (PDL). Approximately 10% of proliferating IHs ulcerate, most commonly involving segmental IHs of the perineal area and focal lesions of the lip. The open wounds are painful and, in the diaper area, compounded by soiling and constant need for cleaning. Treatment of ulcerated IHs (▶ Fig. 12.2) involves local wound care, pain management, and laser therapy. The PDL is extremely effective in healing the ulcers in as few as one to two treatments spaced 7 to 10 days apart. A 7 or 10 mm spot size is used with a short pulse duration (1.5 ms–3 ms) and high fluence (10 J/cm2).5 Propranolol, a beta-antagonist, has become the first line of medical therapy for IH and is useful in treatment of complicated IHs. The mechanism of action is thought to be by inhibition of vasodilation thus causing vasoconstriction of the IH capillaries, reduction in angiogenesis by downregulation of vascular endothelial factor A, and induction of apoptosis. It is useful in both the proliferative and involution phases of the IH natural course.6 Fig. 12.2 Ulcerated proliferating infantile hemangioma (IH) (a) before and (b) after two treatments with the pulsed dye laser (PDL). Once the ulceration is healed, the stage is set for more definitive multimodality procedures to achieve a final result.
12.2 Treatment of Specific Vascular Lesions
12.2.1 Infantile Hemangiomas
Lasers for Vascular Anomalies
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








