Keratoacanthoma: Introduction
|
Keratoacanthoma is a common epithelial tumor of the skin characterized by rapid growth, histopathologic features similar to those of cutaneous squamous cell carcinoma, and a certain tendency toward spontaneous regression. The exact nosology and classification of keratoacanthoma are still a matter of debate. Some authors regard keratoacanthoma as a benign cutaneous tumor that is the prototype of a “pseudomalignant” tumor of the skin, whereas others maintain that it is a malignant neoplasm and should be regarded as a variant of cutaneous squamous cell carcinoma.
 History
History
The first description of solitary keratoacanthoma was provided by Sir Jonathan Hutchinson in 1889, who called this tumor “crateriform ulcer of the face.”1 The term keratoacanthoma was officially first adopted in 1950 by Rook and Whimster.2 In addition to the solitary type of keratoacanthoma, a number of other variants have been described in the literature. Ferguson–Smith, in 1934, reported on a young patient presenting with multiple self-healing squamous cell carcinomas of the skin, a condition that later would be renamed as “multiple keratoacanthomas of the Ferguson–Smith type.”3 The occurrence of hundreds or even thousands of lesions in a single patient, today known as “multiple keratoacanthomas of the Grzybowski type,” was reported by Grzybowski in 1950.4 In 1961, Fisher published the first report on digital keratoacanthoma, pointing at the destructive features of the disease.5 Another rare variant, today described as “keratoacanthoma centrifugum marginatum,” a term that was coined in 1962 by Miedzinski and Kozakiewicz,6 was first described by Puente Duany in 1958.7
Epidemiology
The exact incidence of keratoacanthoma is unknown. The tumor is more frequent in light-skinned persons, and rarer in dark-skinned and Japanese persons. The relative frequency in comparison with squamous cell carcinoma of the skin is controversial, but most studies show a lower incidence of keratoacanthoma than of squamous cell carcinoma. Discordant results may be explained, at least in part, by differences in classification of these lesions.
Studies on gender distribution reveal that both sexes are affected equally, possibly with a slight predilection for men. Keratoacanthoma occurs mostly in adult life, with a peak between the ages of 55 and 65 years; it has been observed rarely in younger patients. The familial type of keratoacanthoma occurs often during adolescence, and a neonatal case has been reported.8 Although the incidence was thought to remain stable after a peak in the sixth decade, a study conducted in a defined population in Hawaii revealed that keratoacanthoma increases with age, in a fashion similar to that observed for cutaneous basal and squamous cell carcinomas.9
The authors of earlier reports considered keratoacanthoma to be a form of epithelial cancer of the skin, and named it accordingly. However, since the introduction of the concept of keratoacanthoma as a benign, self-healing neoplasm distinct from squamous cell carcinoma, the relationship between these two epithelial tumors has been the subject of debate. In their paper published in 1950, Rook and Whimster wrote, “This disease is evidently not cancerous or precancerous.”2 On the other hand, Kwittken, in 1975, stated, “I have come to the firm conclusion that all of these lesions are malignancies and that the formerly accepted concept of a self-healing squamous cell carcinoma of the skin is a correct one,”10 and in 1979, even Rook amended his initial concept by writing, “…transformation from keratoacanthoma to squamous cell carcinoma occurs frequently.”11 Cases of typical keratoacanthoma with metastases have been observed,12 and four possible explanations for this phenomenon have been suggested: an initial misdiagnosis of keratoacanthoma; the presence of both keratoacanthoma and squamous cell carcinoma in the same lesion; the malignant transformation of keratoacanthoma into squamous cell carcinoma; and, finally, the possibility that keratoacanthoma may be a peculiar variant of squamous cell carcinoma.13 The debate is not settled yet, and some authors still maintain that keratoacanthoma represents a benign epithelial tumor, distinct from squamous cell carcinoma,14 whereas others hold that it is a variant of squamous cell carcinoma with tendency to spontaneous regression, but with the potential for giving rise to lethal distant metastases.15 Two studies of large numbers of cases highlighted the impossibility of reliably differentiating keratoacanthoma from squamous cell carcinoma using histopathologic criteria alone.16,17 A patient under infliximab therapy developed multiple squamous cell carcinomas as well as keratoacanthomas, suggesting a common pathogenetic pathway on immunosuppression.18 In addition, multiple keratoacanthomas and multiple squamous cell carcinomas may be observed at the same skin site (“field cancerization”) (Fig. 117-1). Keratoacanthomas have a higher proliferation rate than squamous cell carcinomas.19 Other investigations pointed at similarities among squamous cell carcinoma and keratoacanthoma in the expression of oncogenetic and cell-cycle-regulating proteins as well as regarding the presence of trisomy 7 in a subset of tumors in both groups, thus suggesting a close relationship between these two entities.20–25 On the other hand, studies on loss of heterozygosity, on expression of angiotensin type 1 receptor and of desmogleins 1 and 2, on adhesion molecules vascular cellular adhesion molecule and intercellular adhesion molecule, on telomerase activity, on apoptotic and cell adhesion markers, and on chromosomal aberrations assessed by comparative genomic hybridization showed differences among keratoacanthomas and squamous cell carcinomas.26–33 Using different molecular techniques, both similarities and differences between keratoacanthoma and squamous cell carcinoma have been recently demonstrated.34 In short, at present, and in spite of the great amount of clinical and experimental data collected over the decades, the exact nosology of keratoacanthoma is not clear, and the term abortive malignancy has been proposed.35
Etiology and Pathogenesis
Different etiologic factors are probably involved in the development of keratoacanthomas in different patients, and it seems likely that these different factors act synergistically to induce the onset of a lesion in a given patient. The role of chronic ultraviolet (UV) light exposure in the etiology of keratoacanthoma is well documented by the frequent occurrence on sun-exposed areas, as well as by the presence of keratoacanthomas in patients with xeroderma pigmentosum and after prolonged psoralen and UVA light (PUVA) treatment. In patients with multiple keratoacanthomas, PUVA treatment accelerates the development of the tumors,36 but the risk for keratoacanthoma after therapy with PUVA seems lower than that for squamous or basal cell carcinoma.37 An etiologic link to UV light has been confirmed also by experimental studies in mice.
The relationship of keratoacanthoma to chemical carcinogens has been well documented in humans and in several animals.38 In fact, the incidence of keratoacanthoma is higher in industrial towns, and among industrial workers coming in contact with pitch, mineral oils, and tar. Chemical carcinogens may act in conjunction with UV rays to induce the onset of keratoacanthomas. Smokers seem also to be more affected than nonsmokers.38
Keratoacanthomas have been reported at the site of injury. The association with trauma is also documented by the report of cases occurring after skin grafting, at both the donor and the recipient sites, and at the site of arterial puncture and vaccination.39–41 A recent report described the onset of keratoacanthoma at the site of tattoo, particularly with red ink.42 One of these patients had four keratoacanthomas arising within two separate tattoos. The role of human papillomavirus (HPV) remains controversial. Evidence of HPV infection has been documented by polymerase chain reaction technique,43,44 but other studies failed to detect viral material within lesions of keratoacanthoma.45 Some studies found an association with HPV-25, and HPV-19 and HPV-48 have been isolated in a lesion arising in a human immunodeficiency virus (HIV) patient.46,47 Several other types of HPV have been linked to keratoacanthoma, including types 6, 9, 14, 16, 19, 35, 37, 58, and 61.
Genetic factors probably play a major role in the familial type of keratoacanthoma. In the other variants of keratoacanthoma, it seems likely that genetic aspects interplay with other etiologic factors (i.e., UV rays, trauma, infections) by providing the genetic predisposition for the development of the tumor. Keratoacanthomas are commonly observed in patients with Muir–Torre syndrome, suggesting that the genetic defect(s) of this syndrome also plays a role in the development of keratoacanthoma.48–52 In addition, keratoacanthomas have been observed in patients affected by a variety of skin diseases including psoriasis, lupus erythematosus, lichen planus, atopic dermatitis, herpes zoster, acne conglobata, and pemphigus foliaceus, among others.39
Keratoacanthomas also have been observed in patients under immunosuppression as a result of bone marrow transplantation, cyclosporine treatment, or infection with HIV, thus suggesting that immunosuppression may play an etiologic role in some cases. In these patients, most lesions of keratoacanthoma tested for presence of HPV proved positive, suggesting that immunosuppression may contribute by decreasing the immune response against possible causative agents.53 Similarly, UV light may act not only by direct carcinogenesis, but also by virtue of the local immunosuppression caused by sun exposure.
Little is known about the pathogenesis of keratoacanthoma, and about the exact mechanisms of regression in the absence of any treatment. Studies on p53 oncoprotein expression and p53 gene mutations revealed expression of p53 oncoprotein in the great majority of tested cases, and association with a point mutation in the p53 gene in slightly more than 10% of these cases, suggesting a possible role of p53 gene in the development of some keratoacanthomas.21,25
Patients with incontinentia pigmenti may develop subungual keratoacanthomas. Incontinentia pigmenti is caused by genetic alterations of the NF-κB essential modifier (NEMO). There is evidence that loss of activity of NF-κB is related to development of skin cancer, but somatic mutations of NEMO have not been detected in keratoacanthomas not associated with incontinentia pigmenti.54
Multiple keratoacanthomas of the Ferguson–Smith type show a familial distribution and are transmitted in an autosomal dominant fashion. The gene responsible for this syndrome is localized to chromosome 9q. The majority of the cases have been described in some Scottish families, and in these patients, the syndrome is thought to be caused by a single genetic mutation that occurred before 1790.55
Clinical Findings
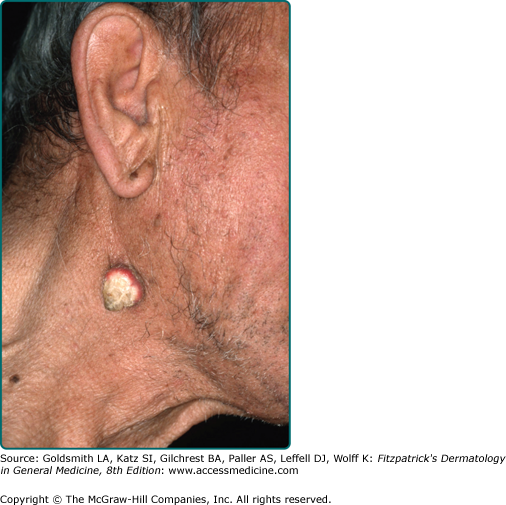
Keratoacanthomas occur mostly on sun-exposed skin of the face, forearms, and dorsal aspects of the hands (Figs. 117-1 and 117-2). Actinic damage is commonly found in the surrounding skin. In most instances, they are located on hairy skin, but lesions with similar clinicopathologic aspects have been described in the oral cavity, the subungual region, the genital mucosa, and the conjunctiva.
The stereotypic example of keratoacanthoma is represented by a solitary lesion growing rapidly within a few weeks, and subsequently showing a slow involution over a period of a few months. Three clinical stages have been described: proliferative, mature, and resolving.39 Lesions in the proliferative stage are rapidly enlarging erythematous papules that grow up to a dimension of 1–2 cm or more. In this stage, the lesions are symmetric and firm and show a smooth surface. In the mature stage there are symmetric, firm, erythematous or skin-colored nodules with a central keratotic core (Figs. 117-2 and 117-3). The central part can appear crateriform if the keratotic core is removed. Ghadially divided mature keratoacanthomas into three main morphologic types: type 1, or bud-shaped; type 2, or dome shaped; and type 3, or berry shaped.40 Regressing lesions are characterized by a keratotic, partly necrotic nodule that becomes progressively flat upon elimination of the keratotic plug, eventually leaving a hypopigmented scar (Fig. 117-4; Box 117-1).
Most Likely
|
Consider
|
Keratoacanthomas may be associated with multiple internal cancers in patients with Muir–Torre syndrome and the related hereditary nonpolyposis colorectal cancer syndrome. Patients with multiple keratoacanthomas should always be evaluated for the presence of typical traits of Muir–Torre syndrome, where cutaneous sebaceous tumors and low-grade visceral malignancies can be observed (most commonly carcinomas of the gastrointestinal tract, but also carcinomas of the lung and genitourinary system, and, occasionally, colonic polyps). It has been suggested that at least some of the patients with multiple keratoacanthomas of the Ferguson–Smith type may have an incomplete form of the Muir–Torre syndrome.
Keratoacanthomas may also occur in patients with xeroderma pigmentosum and, rarely, in patients with lymphomatoid papulosis. Subungual keratoacanthomas may be observed in patients with incontinentia pigmenti.
Several variants of keratoacanthoma have been described, and different morphologic types of keratoacanthoma have been observed in a single patient.56