Keywords
Janus kinase, Tumor necrosis factor-α, Interleukin-17, Interleukin-23
Key points
- •
Investigational therapies aim to inhibit the specific immunologic mechanisms behind plaque psoriasis without widely affecting the normal immune system.
- •
Pathways targeted by investigational therapies include Janus kinase, tumor necrosis factor-α, interleukin-17, and interleukin-23.
- •
Phase II and phase III clinical trials have demonstrated strong safety and efficacy data for several agents, indicating an important future role in treating moderate-to-severe psoriasis.
Introduction
Enhanced insight into the immunogenetic mechanisms behind plaque psoriasis has led to the development of multiple new systemic therapies. These treatments include drugs targeting Janus kinase (JAK), tumor necrosis factor-α (TNF-α), interleukin (IL)-17, and IL-23 pathways ( Table 16.1 ). Clinical trials are currently underway to examine the safety and efficacy of these agents in moderate-to-severe patients. The treatments discussed have demonstrated promising results in phase II or phase III trials and may play an important role in future treatment algorithms.
| Primary Agent | Target | Source | Dosing | Comparisons | Study Length (wk) |
|---|---|---|---|---|---|
| Tofacitinib | JAK1/JAK3 | Papp et al, 2012 | Tofacitinib, 2–15 mg twice daily | Placebo | 12 |
| Bachelez et al, 2015 | Tofacitinib, 5–10 mg twice daily | Etanercept, 50 mg twice weekly or placebo | 12 | ||
| Certolizumab | TNF-α | Reich et al, 2012 | CZP, 400 mg at week 0, then 200–400 mg q 2 wk | Placebo | 12 |
| Mease et al, 2014 | CZP, 200 mg q 2 wk or 400 mg q 4 wk | Placebo | 24 | ||
| Brodalumab | IL-17R | Nakagawa et al, 2016 | Brodalumab, 70–210 mg Q2W | Placebo | 12 |
| Papp et al, 2014 | Brodalumab, 140–210 mg Q2W | None | 120 | ||
| Mease et al, 2014 | Brodalumab, 140–280 mg Q2W | Placebo | 12, then 40 wk open label extension with 280 mg q 2 wk | ||
| Lebwohl et al, 2015 | Brodalumab, 140–210 mg Q2W | Ustekinumab 45–90 mg (standard weight-based dosing) or placebo | 12, then extension with brodalumab 210 mg q 2 wk or 140 mg q 2 wk, q 4 wk, or q 8 wk, or ustekinumab (standard dosing) | ||
| Guselkumab | IL-23p19 | Sofen et al, 2014 | Guselkumab, single dose of 10–300 mg | Placebo | 24 |
| Gordon et al, 2015 | Guselkumab, 5 mg at weeks 0 and 4 and then q 12 wk, 15 mg q 8 wk, 50 mg at weeks 0 and 4 and then q 12 wk, 100 mg q 8 wk, or 200 mg at weeks 0 and 4 and then q 12 wk | Adalimumab (standard dosing) or placebo | 16, then extension through week 40 (placebo patients transitioned to guselkumab 200 mg Q8W) | ||
| Tildrakizumab | IL-23p19 | Papp et al, 2015 | Tildrakizumab 5–200 mg at weeks 0 and 4 and then q 12 wk | Placebo | 52, then 20 wk follow-up |
| Risankizumab | IL-23p19 | Krueger et al, 2015 | Risankizumab single dose of 0.01, 0.05, 0.25, 1, 3, or 5 mg/kg intravenously, 0.25 or 1 mg/kg subcutaneously | Placebo | 12 |
Tofacitinib
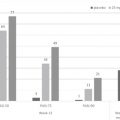
Tofacitinib is an oral JAK1/JAK3 inhibitor currently approved for rheumatoid arthritis at a dose of 5 mg twice daily. The current label includes a black box warning for serious infection and malignancy. It is under investigation for chronic plaque psoriasis. In a phase IIb, randomized, placebo-controlled trial, treatment outcomes were examined by Papp and colleagues using twice a day doses of 2 mg, 5 mg, or 15 mg. At week 12, the proportion of patients who experienced 75% or greater reduction in the Psoriasis Area and Severity Index (PASI-75) was compared with the placebo group. PASI-75 responses were achieved in 25.0% of patients receiving the 2-mg dose, 40.8% of those receiving the 4-mg dose, and 66.7% of those receiving the 15-mg dose, compared with 2.0% in patients with placebo ( P <.001 for each comparison to placebo). Infections were the most common adverse events, seen in 22.4% of the 2-mg dosing group, 20.4% of the 5-mg dosing group, 38.7% in the 15-mg dosing group, and 32% in the placebo group. Of note, 15-mg dosing was associated with statistically significant decreases in hemoglobin (−0.52 g/dL vs −0.14 g/dL with placebo; P <.05), hematocrit, and red blood cell counts as well as transient decreases in neutrophil count.
Rapid and significant improvements in itch severity have been demonstrated with tofacitinib. In patient-reported surveys using 5-mg and 10-mg twice a day dosing, reductions in the itch severity index (ISI) were evident as early as 2 or 3 days after treatment initiation. Among patients with a baseline ISI 1 or greater (indicating the presence of itch), treatment with tofacitinib provided a statistically significant reduction in pruritus ( P <.05) by day 6 and through all 12 weeks of treatment.
A phase III, noninferiority trial between tofacitinib and high-dose etanercept was conducted by Bachelez and colleagues. After 12 weeks, PASI-75 responses were achieved in 39.5% (130/329) of patients receiving 5 mg of tofacitinib twice a day and 63.6% (210/330) of patients receiving tofacitinib 10 mg twice a day, compared with 58.8% (197/335) of those receiving etanercept 50 mg twice weekly, and 5.6% (6/107) of those receiving placebo. Thus, relative to etanercept 50 mg twice weekly, noninferiority was demonstrated with 10-mg dosing of tofacitinib, but not with 5-mg dosing. The rate of adverse events was similar across all groups.
Certolizumab Pegol
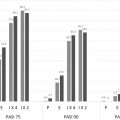
Certolizumab pegol (CZP) is a PEGylated monoclonal antibody to TNF-α approved for the treatment of Crohn disease, rheumatoid arthritis, and psoriatic arthritis. In a phase II trial conducted by Reich and colleagues, subcutaneous doses of CZP 200 mg and CZP 400 mg were compared with placebo. PASI-75 responses were achieved in 75% (44/59) of patients in the CZP 200-mg group ( P <.001 vs placebo), 83% (48/58) of patients in the CZP 400-mg group ( P <.001 vs placebo), and 7% (4/59) of patients in the placebo group. The Physician’s Global Assessment (PGA) score was measured as clear or almost clear in 53% of patients receiving 200 mg and 72% of patients receiving 400 mg, relative to 2% in controls ( P <.001 for each treatment group compared with placebo). Adverse events occurred at comparable rates across the 3 groups.
The efficacy of CZP has also been demonstrated in treating psoriatic arthritis. In a phase III, placebo-controlled trial of 409 patients, Mease and colleagues examined American College of Rheumatology 20% (ACR20) responses for doses of 200 mg every 2 weeks or 400 mg every 4 weeks. After 12 weeks of treatment, ACR20 responses were significantly greater in patients treated with CZP 200 mg (58.0%) or 400 mg (51.9%) relative to placebo (24.3%; P <.001 for each treatment group vs placebo).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree