Chapter 48 Interference Screw Fixation in Bone–Patellar Tendon–Bone Anterior Cruciate Ligament Reconstruction
Introduction
Interference screw fixation on both the femoral and tibial sides remains an effective fixation scheme for bone–patellar tendon–bone (BPTB) anterior cruciate ligament reconstruction (ACLR). Interference screws achieve early stability with aperture fixation and a rigid fixation of graft to host bone. Interference screw fixation of BPTB ACLR provides strength greater than that needed during early rehabilitation.1–3 This chapter includes our ideas and techniques for maximizing the potential for early stability with interference screw fixation of BPTB ACLR.
Graft Preparation
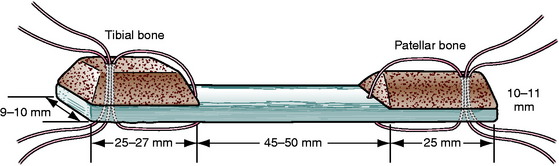
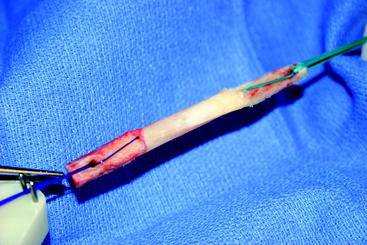
In order to visualize our fixation strategies, the reader should have an understanding of the shape of our graft. Through a slightly medial parapatellar incision, the peritenon of the patella tendon is elevated and the tendon is visualized from its medial to lateral border. We use a ruler not only to confirm the tendon to be 30 to 33 mm in width, but also to measure the distance between longitudinal cuts through the full thickness of the patella tendon 10 to 11 mm apart. We use a combination of an oscillating saw and osteotomes to harvest a trapezoidal-shaped bone block from the tibial tubercle, which is 25 to 27 mm long, and a triangular-shaped bone block from the patella, which is 25 mm long (Fig. 48-1). The bone blocks are trimmed with a rongeur to pass through either a 10- or 11-mm sizing sleeve. The overall length of the graft is usually 90 to 105 mm. Two stay sutures are passed through each bone block and tendon using #1 absorbable monofilament (PDS) for the femoral block and #5 nonabsorbable braided suture for the tibial end of the graft. The absorbable suture in the femoral bone block allows us to cut the suture flush with the skin if it will not pull out. The bone block with the better bone, which is usually the tibial tubercle block, is directed toward the femoral canal with the #1 sutures (PDS). The graft is stretched on a graft board with 20 pounds of tension for 10 to 15 minutes while covered by an antibiotic-soaked gauze (Fig. 48-2).
Screw Selection
A cannulated, round-headed, partially threaded screw is used for the femoral side to protect the graft from laceration at the bone plug–tendon interface. Any number of manufacturers produce round–headed, partially threaded screws.4 A fully threaded screw or a screw with a squared-off head may put the tendinous portion of the graft at risk. We use a fully threaded screw for fixation in the tibial tunnel. The extra threads provide additional fixation, and a round head is not needed distal to the screw and graft.
The literature has shown that the effect of screw diameter is interrelated to the tunnel diameter and the gap size between the graft bone plug and tunnel.5–7 We make our tunnels the same size as the sizers through which our graft bone plugs pass, usually 10 or 11 mm. In both the femoral and tibial tunnels, our first choice for screw diameter is 1 mm less than the tunnel diameter for metal screws, usually 9 or 10 mm, and the same as the tunnel diameter for bioabsorbable screws, usually 10 or 11 mm.
Length of interference screws has not been correlated to fixation strength with BPTB grafts.8–10 We try to match the length of the screw to the length of the graft bone plug. If the surgeon harvests a full 25 mm of bone plug and makes a tunnel deep enough to accommodate the whole plug, he or she should fix the full length of the plug within the tunnel. We frequently use 25-mm-long metal or 28-mm-long bioabsorbable screws in the femoral tunnel, and we use 25-mm-long metal or 28-mm-long bioabsorbable screws in the tibial tunnel.
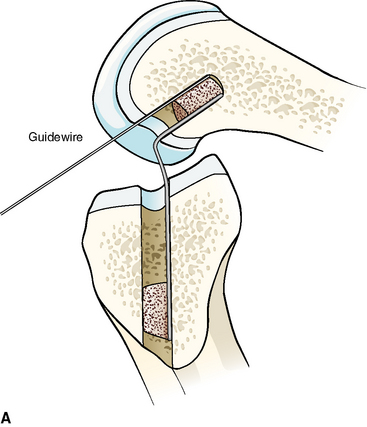
Metal interference screws have a proven track record for secure fixation of BPTB ACLR and are well tolerated by the human body. However, complications related to this hardware option include laceration of the graft on insertion and interference with postoperative magnetic resonance imaging (MRI) scans of the knee, as well as potentially blocking tunnels for revision ACLR. The influence on MRI has been lessened with the use of titanium screws compared with the stainless steel screws initially used. Graft laceration by the screw has not been a problem because we use a plastic sheath to protect both the ACL graft and native posterior cruciate ligament (PCL) when inserting both metal and bioabsorbable screws into the notch and femoral tunnel (Fig. 48-3, A and B).

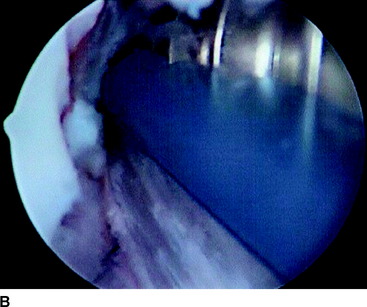
Fig. 48-3 A, Graft protector for screw insertion. B, The plastic sheath protects the graft from laceration.
Bioabsorbable screws were introduced as a device to provide secure mechanical fixation in the interval prior to biological fixation of the graft and then leave the body with no residual foreign material. They create less interference with MRI scans of the knee, cause less graft trauma, and allow easier revision by disappearing or by just drilling through any remnant. The disadvantages of these implants were reported to be breakage and soft tissue reaction due to poor biocompatibility. Poly-L-lactic acid (PLLA) screws are most commonly used today. Studies have shown screw breakage on insertion to be uncommon and, when it does occur, does not cause adverse effects.11,12 A handful of cases of late screw fragmentation have been reported, and soft tissue reactions to PLLA are rare.13,14 The low rate of soft tissue reactions to PLLA is due to the slow rate of degradation in vivo. Studies show persistence of these screws years after insertion.15,16
The tensile strength of cancellous and cortical bone is less than that for titanium or PLLA. For metal and bioabsorbable screws of the same size and shape in the same anatomical and biological scenario, the failure strength will be the same because the construct will fail at the weaker cancellous bone first.3 No significant difference was found when metal and bioabsorbable interference screws in BPTB ACLR were compared with regard to initial strength of fixation as tested with single load and cycle load to failure (LTF).1–3,17,18 Walton showed no difference during a period of interval healing when examining sheep specimens 4 to 52 weeks after interference screw fixation in BPTB ACLR.19 McGuire et al and Kaeding et al showed no significant difference of motion, laxity, or instability between metal and bioabsorbable interference screw fixation of BPTB ACLR as much as 2.4 years postoperatively.11,12
Bone Tunnel Preparation
Much has been written to describe proper tunnel placement in both the tibia and lateral femoral condyle. We use a targeting guide for the tibial tunnel with the goal of the guidewire exiting in the posterior portion of the native ACL footprint, just medial to the anterior horn of the lateral meniscus, centered medial to lateral between the tibial spines. The graft harvest incision is retracted medially to place the distal entry site halfway between the anterior cortical ridge and the medial border of the tibia. We use a guide set at 55 degrees to create a tibial tunnel 50 to 55 mm long. After placing the guidewire, we use intraoperative fluoroscopy to confirm the position of the guidewire within the tibia. On the initial flexed lateral image, the guidewire penetrates the proximal cortex of the tibia with approximately 20% to 40% of the anteroposterior length anterior to the guidewire. A second lateral fluoroscopic image is obtained with the knee fully extended. A line extended from the guidewire should be just posterior to Blumensaat’s line (Fig. 48-4). The guidewire is removed and repositioned if it does not meet the just-mentioned criteria. Once the guidewire is positioned appropriately and no impingement is confirmed, the first reamer, which is 2 mm smaller than the graft size and final tunnel diameter, is passed. Bone reamings are collected to use as autograft for the patella–bone plug defect at the conclusion of the case. The tibial tunnel is then expanded incrementally 2 mm up to the final diameter.
The femoral tunnel is placed on the medial aspect of the lateral femoral condyle with just 1 to 2 mm of cortical bone posterior to the tunnel.20–22 A 5-mm offset femoral guide is used transtibially for femoral tunnel placement (Fig. 48-5). The knee must be flexed to a position such that the guidewire is not directed posteriorly to exit the posterior portion of the femur. The guidewire is placed using the offset guide. The position just anterior to the posterior wall is confirmed on a true lateral fluoroscopic image of the distal femur. A small, 7- or 8-mm acorn reamer is passed to a depth of 35 to 40 mm after proper guidewire position is confirmed. The guidewire is repositioned in the anterior portion of the femoral tunnel and gently tapped into the depth of the tunnel to secure it in a slightly anterior eccentric position within the femoral tunnel. Progressively larger reamers or dilators are used to enlarge the tunnel to its final diameter and avoid posterior wall blowout. A motorized shaver is introduced through the anteromedial portal to remove all loose bone-reaming debris from the posterior joint space and notch. A rasp is placed through the tibial tunnel and up into to the femoral tunnel to confirm posterior wall by palpation and then to rasp smooth the anterior aperture of the femoral tunnel (Fig. 48-6). The arthroscope is then removed from the anterolateral portal and inserted through the tibial tunnel, across the knee joint, and into the femoral tunnel to visually check continuity of the posterior wall. The knee is hyperflexed, and a Beath pin is placed through both tunnels and the femoral cortex to exit the anterior thigh. The Beath pin then brings a passing suture loop across the knee, and the passing suture loop is used to bring the leading graft sutures through the knee to exit the anterior thigh. The graft is brought into the knee.
Relative Position of Screw and Graft within Tunnel
The femoral tunnel is placed on the medial aspect of the lateral femoral condyle with just 1 to 2 mm of cortical bone posterior to the tunnel.20–22 A 5-mm offset femoral guide is used transtibially for femoral tunnel placement. A small (8-mm) acorn reamer is used followed by progressively larger reamers to avoid posterior wall blowout. The tendinous portion of the graft does not fill the aperture of the femoral tunnel, so its relative position within the tunnel can be directed. A soft tissue grasper is inserted through the anteromedial portal and used to rotate the graft bone plug prior to its final entry within the femoral tunnel. We place the cortical side of the bone plug in the posterolateral aspect of the femoral tunnel, placing the tendinous portion of the graft at the posterolateral portion of the aperture. The guidewire and screw are placed opposite the graft in the anteromedial portion of the tunnel (Fig. 48-7, A and B). With regard to depth within the tunnel, the graft bone plug is usually recessed 1 to 2 mm within the femoral tunnel and the interference screw is placed with the head flush with the distal end of the graft bone plug, with no hardware overhanging the graft bone plug to abrade the tendon (Fig. 48-8, A and B). Prior to inserting the graft within the knee, we use a rasp to smooth the anterior lip of the femoral tunnel opening.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree