8.2 Inferior pedicle breast reduction
Synopsis
 The inferior pedicle procedure remains one of the most common techniques employed for breast reduction surgery.
The inferior pedicle procedure remains one of the most common techniques employed for breast reduction surgery.
 Key to a successful outcome with the inferior pedicle procedure is proper shaping of the pedicle.
Key to a successful outcome with the inferior pedicle procedure is proper shaping of the pedicle.
 One of the benefits of the inverted T procedure is reducing the amount of skin between the bottom of the areola and the inframammary fold.
One of the benefits of the inverted T procedure is reducing the amount of skin between the bottom of the areola and the inframammary fold.
 Patients that may benefit from this operation are those with wide, boxy breasts.
Patients that may benefit from this operation are those with wide, boxy breasts.
 Key to the procedure is not carrying the transverse scar close to the midline or laterally beyond the anterior axillary fold.
Key to the procedure is not carrying the transverse scar close to the midline or laterally beyond the anterior axillary fold.
 Although modifications are performed intraoperatively, the majority of the procedure is based on the preoperative patient’s markings.
Although modifications are performed intraoperatively, the majority of the procedure is based on the preoperative patient’s markings.
 Key steps include leaving the bulk of tissue underneath the nipple-areolar complex, limiting the amount of breast tissue in the lower portion of the pedicle, keeping a thick superior flap.
Key steps include leaving the bulk of tissue underneath the nipple-areolar complex, limiting the amount of breast tissue in the lower portion of the pedicle, keeping a thick superior flap.
Evolution of the technique
Breast reduction remains one of the most common procedures related to breast surgery, second only to augmentation mammoplasty. Numerous procedures have been developed specifically for breast reduction surgery, and the inferior pedicle technique has been performed for over three decades.1–4 Many procedures have been developed to reduce scar length and enhance breast shape. With the development of several short scar breast reduction techniques, some surgeons either no longer employ or limit the patients in whom they perform inferior pedicle procedures.
The inferior pedicle procedure is associated with an inverted T incision and still remains one of the most common techniques employed for breast reduction surgery.5–8 The length of the horizontal incision can frequently be kept short, and, in the past, this was considered one of the primary negative aspects of this procedure. Key to a successful outcome with the inferior pedicle procedure is proper shaping of the pedicle to minimize recurrent ptosis and bottoming out. With proper patient selection and proper design, the length of that horizontal incision frequently can be kept short. This technique is particularly suited for very large breasts when there is a large discrepancy between skin envelope volume and breast tissue.
One important aspect is modifying the shape of the pedicle itself, so that the bulk of the tissue is centrally located under the nipple-areolar complex with minimal tissue along the lower border of the inferior pedicle. Hester was one of the first to suggest this concept.9 By keeping the bulk of the tissue centrally and minimizing the tissue along the inferior aspect, secondary problems of bottoming out can be reduced.10,11
Details of planning and marking
Details of planning
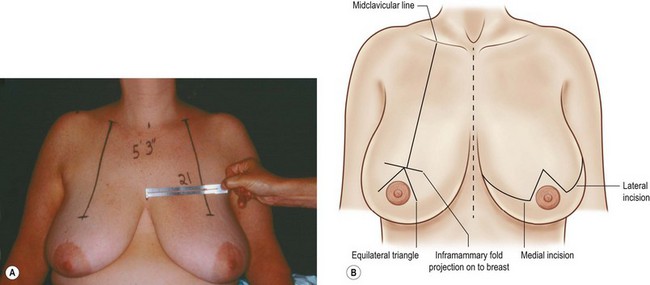
As with any surgical procedure, the two most important components are proper patient selection and proper planning of the procedure. With this technique, although modifications are performed intraoperatively, the majority of the procedure is based on the preoperative patient’s markings. With the patient in the upright position, the initial marking consists of creating a line along the midclavicular plane starting from the clavicle down to a projection point through the inframammary fold where the new nipple-areolar complex will be located. Since in many patients, the nipple-areolar complex does not sit in the midclavicular plane, it is important to create this line, ignoring the actual nipple location if it is too lateral or too medial. After creating the midclavicular lines on both sides, another mark is made in the midline to make sure that these lines are symmetrically placed an equidistance from the midline (Fig. 8.2.1A).
Creating an equilateral triangle
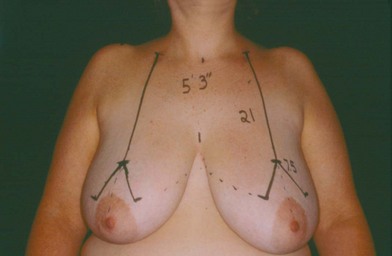
Beginning at the lower extension of the midclavicular line at the point where the nipple projection was created based upon the inframammary fold, an equilateral triangle is created. In smaller patients, it may be in the 7 cm range, while in relatively large patients, frequently it can be anywhere from 8–9 cm in length (Fig. 8.2.1B). In patients with a very wide, boxy breast the base of the triangle should be made slightly longer than either side to help narrow and cone the breast and reduce the boxy appearance. Once these equilateral triangles have been created the next step will be creating the transverse incision lines extending from the lower limbs of the triangle (Fig. 8.2.2).
Visualizing or examining the asymmetric patient
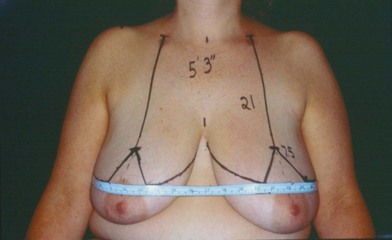
One trick is to take a tape measure and have the patient hold it under their arms against their chest wall and place it transversely along the base of each triangle. As demonstrated in Figure 8.2.3, it is obvious that the patient’s left breast is not only larger but the nipple-areolar complex is lower. Having a transverse tape measure helps one visualize any asymmetry (Fig. 8.2.3).
Detailed description of technical procedure
With the patient in the operating room, there are several important aspects in patient positioning. The arms are on arm boards but should not be at an extreme right angle, since this can distort the breast shape at the time of closure. The arms are well-secured with slight elevation. The patient is prepped and draped in a manner where all the markings are readily visible. A dilute solution of saline/epinephrine is injected, avoiding injection into the site of the inferior pedicle. The first step consists of marking the nipple-areolar complex (Fig. 8.2.4). With this technique, no traction is applied to the nipple-areolar complex as the cookie cutter is applied to the skin. One problem with applying to much tension at the time of marking is that it could lead to a very tight closure with potential healing problems. Also, having the areola being tight and smooth can result in an artificial appearance. After the marking is made, with the areolar tissue at rest, symmetry is compared and proper location of the cookie cutter incision is evaluated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree