Fig. 32.1
Implant exposure in a previous irradiated breast treated with nipple-sparing mastectomy and immediate implant reconstruction and contralateral augmentation

Fig. 32.2
Immediate result 15 days after surgery

Fig. 32.3
Result 4 months after surgery

Fig. 32.4
Result 6 months from the time of the first lipofilling

Fig. 32.5
Result at 10 months when the second lipofilling is planned

Fig. 32.6
Result 2 months from the last lipofilling at the time of the third lipofilling and tattooing
This is not the normal practice but the use of well-vascularized tissue can improve the irradiated tissue itself [13].
32.4.2 Case 2: High-Grade Capsular Contraction in Very Thin Mastectomy Skin Flaps
This situation needs an urgent solution. The presence of both capsular contraction and very thin tissue will require a flap in order to offer the patient an immediate solution.
In this case a deep inferior epigastric perforator flap was offered to solve the problem with contralateral breast reduction at the same time (Figs. 32.7, 32.8, 32.9 and 32.10).

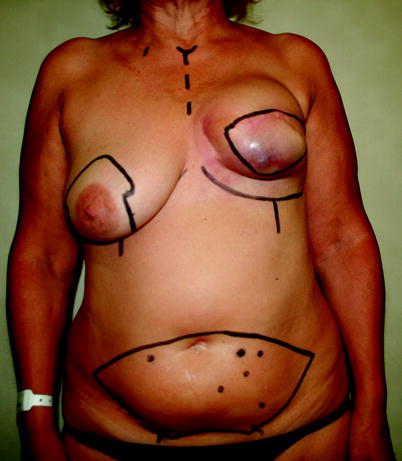
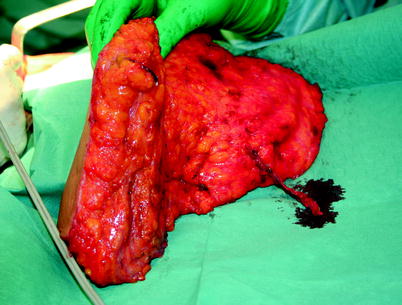


Fig. 32.7
Patient presents with high-grade capsular contraction
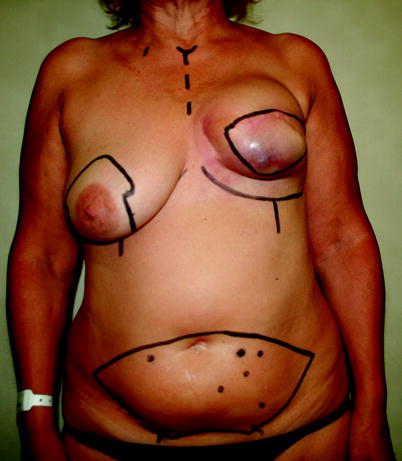
Fig. 32.8
Preoperative planning for deep inferior epigastric perforator (DIEP) flap reconstruction
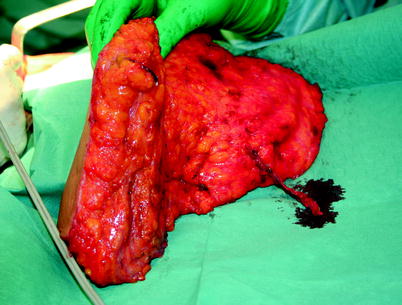
Fig. 32.9
Intraoperative assessment of the DIEP flap

Fig. 32.10
Final result
The final aesthetic outcome was acceptable, but there was a previous periprosthetic capsule remained at the parasternal part. So lipofilling was suggested as a possible improvement.
32.4.3 Case 3: Expander Decubitus
This is another case of a patient who originally underwent immediate reconstruction with an expander. The reason for using the expander was because of the presence of a very thin mastectomy skin flap; it can be considered an emergency reconstruction.
During the expansion there was a decubitus of the expander and the procedure was changed to autologous reconstruction with a deep inferior epigastric perforator flap (Fig. 32.11).
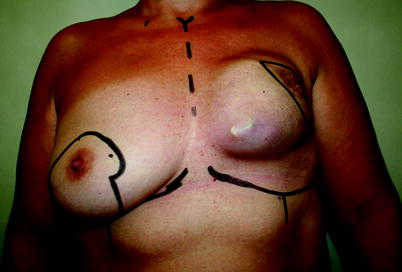
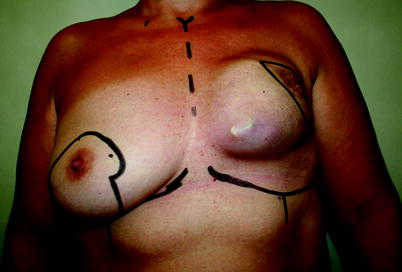
Fig. 32.11
Patient with a decubitus of the expander and planning for DIEP flap reconstruction
The final result at the time of nipple–areola reconstruction is shown in Fig. 32.12.


Fig. 32.12
Final result
32.5 Conclusion
The salvage of the infected and or exposed breast prosthesis remains a challenging but viable option for a subset of patients.
Keys to success include culture-directed antibiotics, capsulectomy, device exchange, and adequate soft tissue coverage. Relative contraindications to breast device salvage include atypical pathogens on wound culture, such as Gram-negative rods, methicillin-resistant Staphylococcus aureus, and Candida parapsilosis.
Patients with a prior device infection and exposure and a history of either radiotherapy or S. aureus on wound culture should be closely monitored for signs of recurrent breast prosthesis infection/exposure and managed cautiously in the setting of elective breast surgery.
References
1.
Handel N, Jensen JA, Black Q et al (1995) The fate of breast implants: a critical analysis of complications and outcomes. Plast Reconstr Surg 96:1521–1533PubMed




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








