The immunobullous diseases are uncommon chronic skin disorders caused by autoantibodies directed against various cutaneous proteins. These disorders primarily occur in older adults and can cause significant discomfort in affected patients and can even be fatal in the case of pemphigus. Patients with immunobullous diseases often have significant quality of life issues in questions pertaining to physical, emotional, and mental health.1 Skin biopsies for routine histology and immunofluorescence are needed to confirm the diagnosis.
Bullous pemphigoid is an uncommon blistering eruption that primary affects elderly patients. The mean age of onset ranges from 68 to 82 years of age.
The incidence is estimated to be between 4.5 and 14 new cases per million per year. It is more common in women.2
Bullous pemphigoid is an autoimmune disease associated with the production of autoantibodies targeting the basement membrane. The basement membrane is important for the adhesion of the epidermis to the dermis, and so when targeted, leads to a separation (blister) in this space. The antigens themselves are parts of the hemidesmosomes of the basal cells. The targets are BP 180 and BP 230.3 BP 180 is a transmembrane protein in basal cells, which is the extracellular noncollagenous domain of type 17 collagen. BP 230 is a cytoplasmic plakin family protein of the hemidesmosome. There is evidence for the pathogenic roles of these autoantibodies in this disease, especially against BP 180.
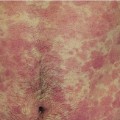
Despite being labeled a blistering disorder, many patients will present initially with prebullous pemphigoid which presents as a pruritic urticarial rash without blisters.4,5 The pruritus can be severe. When blisters develop, they are tense blisters because they are forming between the dermis and epidermis and do not easily rupture.
In the prebullous phase, the patient has pruritic urticarial plaques. In the bullous phase, the patient develops blisters. Most commonly the tense blisters are bilateral, symmetric, and on the trunk and proximal flexural extremities (Figure 22-1). The blisters may or may not have surrounding erythema. Mucosa can be involved, but usually in less than 20% of patients.
Histopathology of a skin biopsy from the edge of an intact bulla shows a subepidermal bulla with a dermal eosinophil inflammatory component (Figure 22-2).
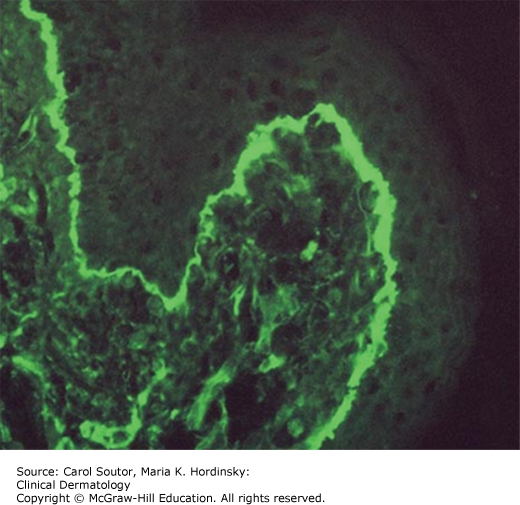
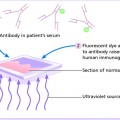
Direct immunofluorescence of a skin biopsy taken of normal skin near a bulla shows a linear deposition of C3 and IgG along the basement membrane zone (Figure 22-3).
Indirect immunofluorescence of the blood shows linear IgG along the blister roof on salt-split skin (Many patients do not have detectable circulating antibodies).
An enzyme-linked immunosorbant assay (ELISA) for BP 180 and BP 230 is available.
The key diagnostic features of pemphigoid are tense, pruritic vesicles and bullae.
In the prebullous phase
✓ Urticaria: The individual lesions of urticaria should last less than 24 hours.
✓ Drug rash: Usually truncal with macular papular erythema.
✓ Dermatitis: This eruption is usually eczematous.
✓ Other: primary pruritus.
In the bullous phase
✓ Other bullous disorders (Table 22-1).
✓ Other: epidermolysis bullosa acquisita, dermatitis herpetiformis, bullous drug reaction, bullous tinea, bullous diabeticorum, coma/pressure bullae, edema.
Clinical and laboratory findings in bullous diseases.
| Disease | History and Physical Examination | Routine Histology and Direct Immunofluorescence |
|---|---|---|
| Pemphigoid | Tense pruritic bullae that are bilateral and symmetric | Subepidermal blister with IgG and C3 at the basement membrane |
| Pemphigus | Flaccid bullae with positive Nikolsky sign | Blister within epidermis with intercellular IgG and C3 |
| Dermatitis herpetiformis | Pruritic crusts on extensor surfaces | Subepidermal blister with IgA in dermal papillae |
| Stevens–Johnson/TEN | Very ill patients with significant crusting of lips, nose, and eyes. Nikolsky sign is positive | Subepidermal blister with epidermal necrosis. Immunofluorescence is negative |
| Epidermolysis bullosa | Tense blisters in areas prone to trauma | Subepidermal blister with IgA at the basement membrane |
Skin biopsies for routine histopathology should be done from the edge of the blister and skin biopsies from perilesional skin should be sent for direct immunofluorescence. Blood could be sent for indirect immunofluorescence. Tense bullae can be drained with a sterile needle leaving the roof intact to act as a biologic dressing. White petrolatum can be used with nonstick dressings for any eroded areas. Bullous pemphigoid can be a chronic relapsing disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree