Immediate Tissue Expander
Eric G. Halvorson
Joseph J. Disa
DEFINITION
Immediate tissue expander placement is performed following skin-sparing or nipple-sparing mastectomy as a prelude to either two-stage implant reconstruction or “delayedimmediate” autologous reconstruction.
The advantages of expander placement (compared to immediate autologous reconstruction) include shorter operation, lack of donor site, shorter hospital stay, shorter recovery, ability to adjust final volume, and a “perkier” result.
The disadvantages of expander placement include multiple postoperative office visits for expansions, discomfort associated with the expansion process, a second (albeit outpatient) surgery if proceeding with two-stage implant reconstruction, and the permanent risks of implants (capsular contracture, rupture, rotation, rippling, infection, malposition, and exposure).
PATIENT HISTORY AND PHYSICAL FINDINGS
It is beneficial for the initial consultation to occur separate from multidisciplinary clinic visits focused on cancer care. Patients presenting to the plastic surgeon after such visits are often overloaded with information and overwhelmed by all the options and information related to reconstruction.
It is critical to determine the patient’s goals for reconstruction and to ascertain their preferences with respect to breast size, breast shape, willingness to accept surgical risk, willingness to accept donor-site morbidity, operative length, hospital stay, recovery process, postoperative follow-up protocol, secondary surgeries, and long-term complications.
Having a physician extender well versed in reconstructive options to meet with patients and show them patient photographs is an incredibly helpful prelude to the physicianpatient consultation.
Physical examination of the breasts is performed to evaluate any masses and whether or not skin involvement or peau d’orange is present. The overall size and degree of ptosis are noted.
Patients with skin involvement or significant ptosis will typically require skin excision. If performed as an inverted “T” or Wise pattern, the risk of mastectomy flap necrosis is increased.
Alternatively, one can perform a generous horizontal, oblique, or vertical ellipse or two-stage Wise pattern excision with the vertical closure first and a horizontal excision at the inframammary fold (IMF) 3 to 6 months later.
The breast width, height, and projection are measured in centimeters. These measurements are used for selecting a tissue expander (as described in the following text).
SURGICAL MANAGEMENT
Ideal candidates for expander placement are thin nonsmokers undergoing bilateral mastectomy who have not, and will not, receive radiotherapy.
Smokers are prone to mastectomy flap necrosis and infection.
Radiotherapy increases the risk of infection, implant exposure, and capsular contracture.
Previously radiated skin will not expand well.
Although obesity increases the risk of complication for any type of reconstruction, heavier patients tend to have better cosmetic results with autologous reconstruction than with implants, as it can be difficult to match the opposite breast after a unilateral mastectomy or give adequate volume/ptosis after a bilateral mastectomy.
Patients with very large breasts who require skin removal during mastectomy are at risk for mastectomy flap necrosis and tend to require secondary procedures to address residual excess skin. These patients often have ample donor sites for autologous reconstruction, which may be a better option.
Patients with small breasts who want them to be larger can achieve that goal through expansion.
Patients who have minimal ptosis and want their breasts to be slightly smaller are candidates for single-stage implant reconstruction.
Using a tissue expander as a bridge to autologous reconstruction, so-called delayed-immediate reconstruction, is considered when the patient is likely to receive postoperative radiation therapy, as radiating autologous flaps can result in fat necrosis, firmness, and shrinkage.
A minority of surgeons prefer to accept the risks of radiating an autologous flap when compared to the risks of performing delayed reconstruction in a radiated field.
Other reasons to consider delayed-immediate reconstruction are to gain control of the skin envelope, to expedite surgery and adjuvant therapy, and to modify risk factors (smoking, obesity) and when patients are undecided.
Preoperative Planning and Implant Selection
Good communication with the breast surgeon is important to ensure oncologic goals are maintained and that reconstruction is appropriately staged.
Patients with advanced disease, requirement for immediate postoperative adjuvant therapy, unstable social environment, and/or uncertainty regarding goals for reconstruction may be better served by delayed reconstruction.
Prior to mastectomy, the patient must be marked in the standing position. The IMF is marked on each side, and the midline is drawn between the sternal notch and xiphoid process. The overall outline of the breasts is marked.
Although a transverse ellipse around the nipple-areolar complex (NAC) is commonly used for the mastectomy incision, the authors’ preference is an oblique ellipse parallel to the pectoralis major fibers (FIG 1). This renders the medial scar less visible in clothing, allows for better subincisional muscular coverage, and facilitates a stair-step approach during the exchange procedure (as described in the following chapter).
Tissue expanders are selected preoperatively based on the width of the patient’s breast. There are many different tissue expanders to choose from, but most are textured and anatomic, providing lower pole projection.
Some are taller than they are wide, some are wider than they are tall, and some are semicircular or crescentic and focus on lower pole expansion.
Some have tabs to secure the expander.
Most have integrated metal ports that are located with magnets, although a remote port is useful when placing the expander under a thick flap (such as a latissimus dorsi flap in an obese patient). In such patients, finding the port with a magnet can be difficult and a longer needle is required, placing the expander at risk for rupture.
Positioning
Patients are placed in the supine position under a general anesthetic with arms padded circumferentially and abducted at 80 to 90 degrees.
Following mastectomy, the patient is positioned such that the sternum is parallel to the floor (via head elevation or reverse Trendelenburg).
TECHNIQUES
▪ Tissue Expander Placement
First Step—Wound Assessment
Following mastectomy, the wounds are irrigated and hemostasis is obtained.
The mastectomy flaps are evaluated by examining their thickness and assessing color and capillary refill.
Areas where dermis is exposed internally should be carefully evaluated externally.
Areas where the external skin is pale without capillary refill should be excised.
Laser-assisted indocyanine green fluoroscopy has been promoted to assess mastectomy flap perfusion; however, guidelines for its use and interpretation have not been firmly established.1
Use of tumescent solution by the extirpative surgeon makes assessment of mastectomy flaps difficult and has been shown in some studies to be associated with a higher rate of mastectomy flap necrosis.2,3,4
When there is significant concern for mastectomy flap necrosis, or if debridement of questionable tissue will lead to closure under tension or an open wound, then aborting reconstruction is strongly advised.
If necessary, the IMF can be recreated with interrupted suture; however, the position of the inferior edge of the expander will ultimately determine the IMF, which can be adjusted further during an exchange procedure if desired.
Some surgeons try to establish the native IMF during this initial procedure (which may make the exchange procedure simpler), whereas others intentionally place the expander lower than the IMF to increase lower pole expansion and projection (which requires recreation of the IMF with suture during the exchange procedure).
The author’s preference is to preserve the native IMF when performing single-stage implant reconstruction, when placing a significant initial fill volume in the expander, or when the IMF is already low.
When performing delayed two-stage implant reconstruction or when placing minimal initial fill volume in the expander, placing the implant below the IMF will preferentially expand the lower pole and permit the surgeon to create minimal ptosis at the exchange procedure (as described in the following chapter).
Another reason to consider placing the expander lower than the native IMF is when adjuvant radiotherapy is expected. Radiotherapy almost always causes fibrosis and contracture of the pectoralis major and soft tissue surrounding the implant, with superior migration of the expander.
Second Step—Creation of Implant Pocket
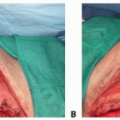
The tissue expander cannot be covered by the mastectomy flaps alone, which are thin and offer poor soft tissue coverage. Ideally, the surgeon should provide complete musculofascial coverage with the pectoralis major and serratus anterior muscles (TECH FIG 1A) or use an acellular dermal allograft (ADM) or other product in addition to the pectoralis major muscle.
An emerging technique is to use complete acellular dermal matrix (ADM) coverage with adjuvant fat grafting at the time of implant exchange, which is beyond the scope of this chapter.
The lateral edge of the pectoralis major muscle is pinched between the surgeon’s index finger and thumb and pulled away from the chest, revealing a loose areolar plane between the pectoralis major and minor muscles. Dissection in this plane commences with Bovie cautery, but once the
subpectoral space is entered, much of the superior and medial implant pocket can be created via blunt digital dissection before using lighted retractors for direct visualization.
A lighted retractor is quite helpful to finish medial dissection, as great care must be taken to ligate or cauterize the intercostal perforators (TECH FIG 1B,C).
The medial boundary is defined externally by the preoperative markings that define the patient’s native breast form. Internally, it is quite common to release the medial and inferomedial origins of the pectoralis major muscle. It is important not to release this area excessively, as symmastia can result and is difficult to correct.
After the subpectoral plane is developed, the inferior insertion of the pectoralis major muscle is examined (TECH FIG 1D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree