Immediate Reconstruction After Skin-Sparing Mastectomy Through A Periareolar Approach
Joan E. Lipa
History
Skin-sparing mastectomy (SSM) became the mainstay of surgical treatment for breast cancer in the 1990s, limiting the amount of native breast skin removed in order to improve the aesthetics of immediate breast reconstruction. SSM by definition includes excision of the nipple-areolar complex and may also involve inclusion of previous biopsy or partial mastectomy scars with or without intervening breast skin, as well as excision of excess breast skin as in mastopexy techniques. It has been shown to be oncologically safe when compared with traditional non-SSM, with mastectomy flap necrosis rates at approximately 10% but comparable to non-SSM (1). The breast cancer recurrence rate following SSM ranges from 2% to 7% (1,2,3,4). Local recurrence does not frequently correlate with distant metastatic disease or decreased survival.
If the mastectomy incision is limited to the periareolar region, a patchlike effect from autogenous tissue reconstruction can be avoided, as the entire skin paddle will reconstruct the areola. Similarly, if an expander/implant reconstruction is carried out, scars are limited and can be at least partially camouflaged by tattooing for areolar reconstruction. Therefore, SSM through a periareolar approach has the potential to result in the ideal immediate breast reconstruction (5), regardless of which technique for reconstruction is employed.
Indications
SSM with immediate reconstruction through a periareolar approach was originally described for early-stage breast cancer, from ductal carcinoma in situ (DCIS) to early invasive (stage I or stage IIA) disease, but it was rapidly adapted for use in prophylactic mastectomy. It is now also used in the case of high-risk or locally advanced disease (stage IIB or III) and in cases of failed breast conservation treatment (6). In these cases, autogenous tissue immediate breast reconstruction techniques are preferable since radiation either will be or will have been administered as adjuvant therapy.
It is most favorably used for moderate-sized breasts without ptosis and without scars other than those preexisting in a circumareolar location. If ptosis is present, then the mastectomy skin can be adjusted using mastopexy techniques. Similarly, if scars are present, then they ideally will lie within a mastopexy pattern; otherwise they may require resection separate from the periareolar scar or in continuity with a bridge of skin between the scar and the periareolar incision, which then commits the patient once again to either a more extensive scar or skin paddle that will not be concealed by areolar reconstruction.
Contraindications
Conversely, SSM through a periareolar approach is contraindicated if there is involvement of skin with tumor, either with direct invasion or with inflammatory breast cancer, as skin resection will be required in order to achieve adequate anterior margins. Relative contraindications include multiple scars that compromise residual mastectomy skin and pendulous breasts that require a large skin reduction. Smokers are not ideal candidates because there is a higher risk of mastectomy flap necrosis. If there appears to be intraoperative mastectomy flap compromise with areas that do not appear to be viable, these areas should be resected. In addition, a plan for immediate implant reconstruction may have to be adjusted to staged tissue expander reconstruction, or, in the case of autogenous reconstruction, a larger patch of skin may be left of inset in a delayed fashion several days after the mastectomy skin flaps have been demarcated. Finally, immediate breast reconstruction may be not desirable if postoperative radiotherapy is planned, because of the potential effects of radiotherapy on the reconstruction.
Preoperative Planning and Marking
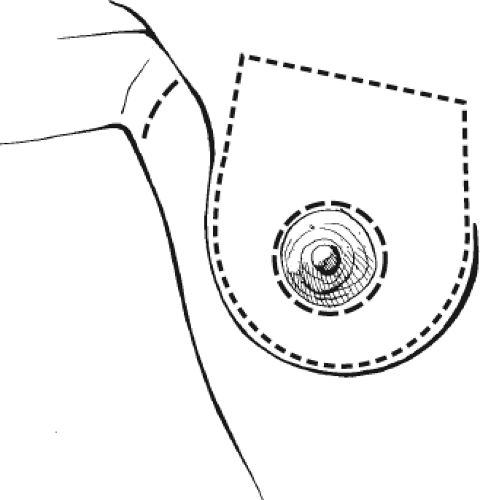
The incision is marked, which is approximately 5 mm outside of the limits of the areolar pigmentation (Fig. 56.1). Ideally the access for the mastectomy should be at least 5 cm in diameter (4), and this diameter can be recorded to help decide, in the case of an autogenous reconstruction, the size of the skin paddle that should be left at the conclusion of the reconstruction. The limits of the dissection are also marked—the inframammary fold, anterior axillary line, parasternal region, and clavicle—in order to visualize the borders of the resection and improve the reconstructive outcome. In the case of unilateral mastectomy, the normal, unoperated breast landmarks should also be marked, as these serve as an intraoperative reference for the breast reconstruction. If a sentinel node biopsy is planned, it may be necessary to access this through a separate axillary incision, as this will provide a direct approach for visualization of vital blue dye and can also be marked to inform the patient preoperatively of where scars will be.
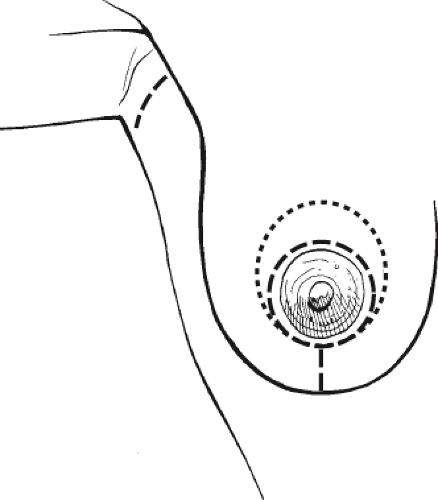
If there is ptosis and/or it is anticipated that there will be skin excess following the mastectomy, the appropriate markings for mastopexy incisions should also be outlined (Fig. 56.2). However, the new position of the areolar opening should be positioned conservatively, at least 1 cm lower than that predicted in standard reduction/mastopexy techniques (7). Although mastopexy markings can be used by the breast surgeon to improve access, my preference is to only cut the mastopexy incisions after evaluating the overall integrity of the
mastectomy skin flaps. However, an incision that extends vertically inferiorly from the areola can be planned within this pattern and be available for use by the breast surgeon (8).
mastectomy skin flaps. However, an incision that extends vertically inferiorly from the areola can be planned within this pattern and be available for use by the breast surgeon (8).
The appropriate expander should be immediately available, and preferably a range of implants and sizers should be ordered if an attempt at immediate one-stage reconstruction is made. Of note, this can only be accomplished if the patient is willing to go smaller in size, because once the periareolar incision is closed, the skin envelope will be reduced and will not be able to accommodate an implant of the size of the breast that was removed. The exception is if the areolar defect is going to be replaced with a latissimus dorsi skin paddle, in which case an implant of comparable size to the weight of the removed breast tissue can be used. If an autogenous flap reconstruction is planned, the landmarks and outline of the skin paddle are also marked preoperatively, preferably in the standing position. Some people outline the proposed skin paddle on the flap that will recreate the areolar defect. My preference, however, is to wait until the flap is within the mastectomy pocket to determine the exact location of the skin paddle and only at that time to commit to incising it.
Operative Technique
Skin-Sparing Mastectomy
The patient is positioned supine under general anesthesia and should have deep vein thrombosis prophylaxis, usually with sequential compression devices, as well as antibiotic prophylaxis. Even for unilateral mastectomy, both breasts should be prepped and draped.
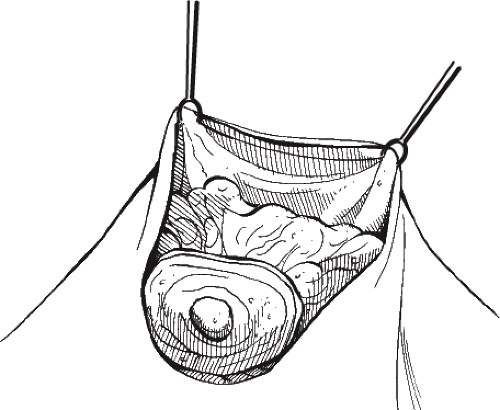
Some surgeons carry out infiltration with dilute adrenaline solution with or without local anesthetic around the incision and in the plane of the resection between the subcutaneous tissue and the breast. This is particularly useful if sharp scalpel dissection is used in a sweeping fashion to carry out the breast excision after periareolar incision is made. However, if diathermy cautery is used for the dissection, then infiltrating fluid hampers the effectiveness of the cautery. In either case, the periareolar incision should be made with a scalpel. If cautery is being used, the skin flaps are gently retracted straight up with either skin hooks or Lahey clamps placed on the deep subcutaneous tissue and deep dermis if necessary, as opposed to on the skin edge (Fig. 56.3). Countertraction on the breast gland is helpful in developing the plane. Dissection proceeds sequentially, medially, inferiorly, superiorly, and laterally. A headlight is helpful. Once the breast has been separated from the subcutaneous tissue, narrow retractors are used to displace the mastectomy skin away from the medial reflection of the breast tissue, and the breast tissue is removed from the pectoralis fascia and eventually delivered from the mastectomy pocket (Fig. 56.4). The axillary dissection, if necessary is carried out en bloc, prior to delivery of the entire specimen in continuity. If sentinel node biopsy is performed, it may be done through the periareolar incision if the skin is distensible; otherwise a separate axillary incision is used.
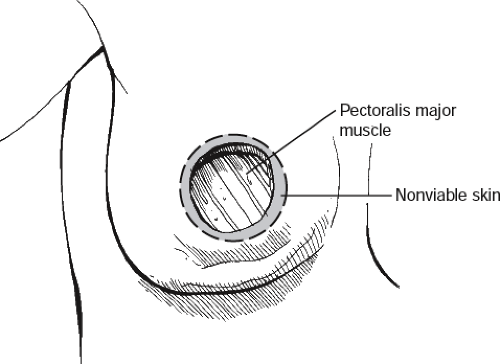
The edges of the incision should be evaluated, and if they are damaged or nonviable, they should be excised (Fig. 56.5). Mastectomy skin in general should also be evaluated. If it appears nonvascularized, it should be excised. If the flaps appear compromised but still viable, then this has to be taken into
account for either volume of fluid instilled in a tissue expander or consideration made not to proceed with immediate implant reconstruction if that was the original plan, and if mastopexy incisions were planned, it may be better to delay this until a second stage. Furthermore, evaluation of the extent of dissection of the mastectomy pocket is made, and the natural landmarks for the inframammary fold and remaining breast limits are reconstituted prior to proceeding with the breast mound reconstruction. My preference is for internal sutures of 2-0 Vicryl or PDS, attaching deep dermis corresponding to the level of the fold to the chest wall soft tissues. Hemostasis should be meticulously obtained.
account for either volume of fluid instilled in a tissue expander or consideration made not to proceed with immediate implant reconstruction if that was the original plan, and if mastopexy incisions were planned, it may be better to delay this until a second stage. Furthermore, evaluation of the extent of dissection of the mastectomy pocket is made, and the natural landmarks for the inframammary fold and remaining breast limits are reconstituted prior to proceeding with the breast mound reconstruction. My preference is for internal sutures of 2-0 Vicryl or PDS, attaching deep dermis corresponding to the level of the fold to the chest wall soft tissues. Hemostasis should be meticulously obtained.
Immediate Reconstruction
For the complete details of the techniques of tissue expander and/or implant placement or specific flap elevation, the reader is directed to the appropriate chapters in this book. However, some features of these reconstructive techniques as they relate specifically to immediate breast reconstruction following SSM through the limited periareolar approach are highlighted here.
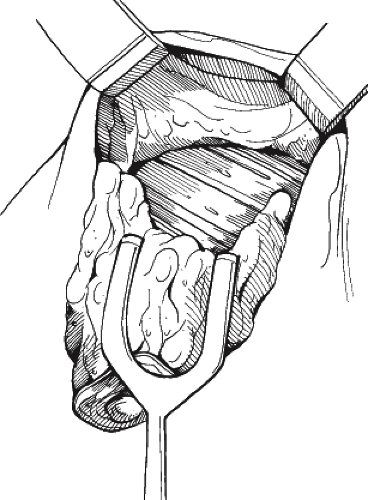
If a tissue expander reconstruction is carried out with the aid of a regenerative tissue matrix such as AlloDerm (LifeCell Corp., Somerville, NJ), a fiberoptic-lighted right-angle breast retractor is necessary, often with gentle retraction of the opposite mastectomy skin with a shallow retractor to hold the tissue away and improve visibility. First, the inferior edge of the pectoralis major muscle is identified and lifted superiorly, and the pectoralis muscle flap is mobilized (Fig. 56.6). Next, the tissue matrix is placed along the inframammary fold, using 2-0 PDS suture to secure it first at its most medial-superior point along the fold, or one may also start laterally (Fig. 56.7). The integrated-port expander can now be placed under the pectoralis major muscle superiorly and the tissue matrix inferiorly (Fig. 56.8), and then these two tissues are reapproximated with PDS to complete coverage of the expander. Intravenous saline fluid can be placed in the expander under direct vision prior to reapproximation of the pectoralis–tissue matrix junction, and further infiltration can be carried out after coverage. Drains are placed; my preference is for two flat drains, one in the subcutaneous pocket
inferiorly and the other in the subpectoral pocket. The closure for the incision is ideally placed so that it lies superficial to the muscle. It either can be closed in a purse-string fashion (Fig. 56.9) or skin at 3 and 9 o’clock can be excised (Fig. 56.10) to allow for a transverse linear closure (Fig. 56.11). If small dog ears remain, these usually flatten out during the expansion process. Alternatively, the excess can be taken vertically (Figs. 56.12 and 56.13), although this will place the incision over the tissue matrix as opposed to over the muscle, but this may lead to a more symmetric scar location if a balancing contralateral vertical-pattern mastopexy is planned. Skin closure is carried out with 3-0 Monocryl deep dermal sutures followed by a 4-0 Monocryl running intracuticular suture. Following closure, it is important to observe the mastectomy skin flaps once again for vascular compromise; if this is the case, then saline can be withdrawn from the expander until the skin flaps once again appear to have good color and capillary refill.
inferiorly and the other in the subpectoral pocket. The closure for the incision is ideally placed so that it lies superficial to the muscle. It either can be closed in a purse-string fashion (Fig. 56.9) or skin at 3 and 9 o’clock can be excised (Fig. 56.10) to allow for a transverse linear closure (Fig. 56.11). If small dog ears remain, these usually flatten out during the expansion process. Alternatively, the excess can be taken vertically (Figs. 56.12 and 56.13), although this will place the incision over the tissue matrix as opposed to over the muscle, but this may lead to a more symmetric scar location if a balancing contralateral vertical-pattern mastopexy is planned. Skin closure is carried out with 3-0 Monocryl deep dermal sutures followed by a 4-0 Monocryl running intracuticular suture. Following closure, it is important to observe the mastectomy skin flaps once again for vascular compromise; if this is the case, then saline can be withdrawn from the expander until the skin flaps once again appear to have good color and capillary refill.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree