Introduction646
INTRODUCTION
TREMATODE INFESTATIONS
SCHISTOSOMIASIS
Histopathology
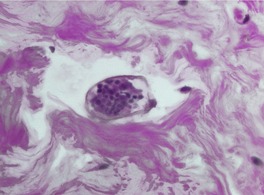
Fig. 29.1
OTHER TREMATODES
CESTODE INFESTATIONS
CYSTICERCOSIS

Fig. 29.2
Histopathology

Fig. 29.3

Fig. 29.4
SPARGANOSIS
Histopathology
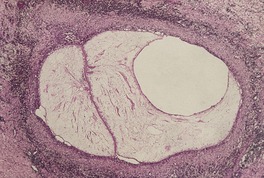
Fig. 29.5
ECHINOCOCCOSIS
NEMATODE INFESTATIONS
ONCHOCERCIASIS
Histopathology65.66. and 67.
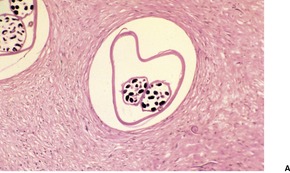
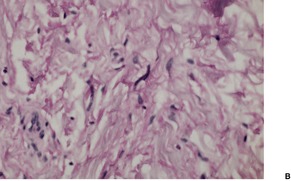
Fig. 29.6
GNATHOSTOMIASIS
Histopathology80
DIROFILARIASIS
Histopathology
LARVA MIGRANS
Histopathology
OTHER NEMATODES
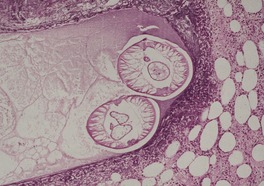
Fig. 29.7
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Helminth infestations
Helminthic parasites are responsible for a number of important diseases of tropical countries. These include schistosomiasis, caused by the trematode flukes; cysticercosis and sparganosis, resulting from the larvae of certain tapeworms (cestodes); and onchocerciasis, dirofilariasis, and larva migrans occurring as a consequence of nematode infestations. 1 The most common helminth infection in the United States and Western Europe, enterobiasis (pinworm), produces no primary cutaneous pathology, although changes in the perianal region, secondary to scratching, may occur. 2
It has been estimated that 200 million people are infested with one or other of the three major species of schistosome fluke. 3Schistosoma haematobium (found in most of Africa and in the Near East) has a predilection for the bladder, S. japonicum (common in parts of the Far East) for the gut, and S. mansoni (found in Africa and parts of the Caribbean region and the northeast part of South America) for the portal circulation.4. and 5. Four types of skin lesions have been described:6.7.8.9.10.11.12.13.14. and 15.
1. a pruritic, erythematous and urticarial papular rash (cercarial dermatitis, ‘swimmer’s itch’) associated with the penetration of the cercariae through the skin en route to the various venous plexuses to mature16
2. urticarial lesions associated with the dissemination of the cercariae or the laying of eggs by the adult flukes
Urticarial lesions are more common with S. japonicum, 8 and perineal lesions with S. haematobium,9. and 21. whereas extragenital cutaneous manifestations are usually a complication of S. japonicum and S. haematobium, but are quite rare with S. mansoni. 22 The term ‘bilharziasis’ is used for the ectopic deposition of ova within the dermis. 23 The late development of squamous cell carcinoma has been reported in the verrucous genital lesions. 10
Cercarial dermatitis may also be seen, rarely, as a result of penetration of the skin by cercariae of species of schistosome that are unable to develop further in humans, being destroyed before they reach the venous plexus.10. and 24. Cercarial dermatitis can also be produced by cercariae of the closely related genus Trichobilharzia. 25
ELISA methods have been developed to assist in the laboratory diagnosis of schistosomiasis. 26
The cercarial dermatitis shows intraepidermal spongiosis with exocytosis of eosinophils and neutrophils, sometimes forming microabscesses. 8 Cercariae are not usually seen. The dermal reaction is mild, with edema, vascular dilatation, and a mild perivascular inflammatory cell infiltrate and some interstitial eosinophils.
Genital and perineal lesions show hyperkeratosis and acanthosis. There may be prominent pseudoepitheliomatous hyperplasia, and at times focal ulceration or draining sinuses with accompanying acute inflammation.7. and 13. The dermis contains numerous ova, some associated with a granulomatous reaction, including foreign-body giant cells. Other eggs are in microabscesses, often containing numerous eosinophils. Flukes may be seen in cutaneous vessels.
Extragenital lesions show numerous ova in the superficial dermis associated with necrobiosis and palisading granulomas.11.12. and 15. Eosinophils, neutrophils, and foreign-body giant cells are found in most lesions, whereas in later lesions there may be degenerating or calcified ova, plasma cells and fibroblasts, with variable fibrosis (Fig. 29.1). Identification of ova in late fibrous lesions may be difficult. 22
An ovum of Schistosoma in an area of fibrosis. No reaction is present. (H & E)
The ova of the three major species have characteristic features. The ova of S. haematobium have an apical spine, those of S. mansoni a lateral spine, and those of S. japonicum have no spine. 8 The ova of S. mansoni and S. japonicum may be acid fast.
A larval trematode, identified as a mesocercaria of an undescribed species belonging to the subfamily Alariinae, has been removed from an intradermal swelling. 27 The lung fluke Paragonimus westermani rarely produces a cutaneous inflammatory lesion; it often extends into the subcutis. The lesions may include an abscess containing many eosinophils.28. and 29. An egg of the parasite may be present in the abscess. 30
The larval phase of Taenia solium, the pork tapeworm, may infect humans as an accidental intermediate host, with the formation of one or more asymptomatic subcutaneous nodules 1–3 cm in diameter.31.32.33.34.35.36.37.38. and 39. The larvae have a predilection for the chest wall, upper arms, and thighs. 40 The nodules are composed of a white cystic structure with an outer membrane containing clear fluid and a cysticercus larva attached to one edge (Fig. 29.2). Surrounding the gelatinous cyst is a host response of fibrous tissue.
Cysticercosis. Subcutaneous lumps removed from the thighs.
The diagnosis is made by the characteristic appearance of the scolex of the cysticercus larva (Fig. 29.3). The fibrous tissue reaction in the subcutaneous tissue contains a moderate chronic inflammatory cell infiltrate which includes variable numbers of eosinophils (Fig. 29.4). A few scattered giant cells are sometimes present.
Cysticercus larva removed from a subcutaneous ‘cyst’ of the skin. (H & E)
Cysticercosis. The cyst wall is composed of inflamed fibrous tissue and many eosinophils. (H & E)
Sparganosis is a rare infestation caused by the larval form of a tapeworm of the genus Spirometra.41.42. and 43. It occurs in many parts of the world, mainly in the tropics. Humans are a second intermediate host. Infestation may result in a subcutaneous nodule which slowly migrates. Bisection of the nodule after excision will reveal a white thread-like worm about 1 mm in width and from a few centimeters to 50 cm in length.44. and 45.
There is a subcutaneous, partly granulomatous, inflammatory mass composed of lymphocytes, plasma cells, neutrophils, and variable numbers of eosinophils. 46 Portions of worm are usually seen within the mass, 41 or there may be a cavity where the larva has been (Fig. 29.5). The larva has a flattened structure with both longitudinal and horizontal muscle bundles, giving a ‘checkerboard’ appearance. A longitudinal excretory canal is also present, and basophilic calcareous corpuscles, a characteristic feature of cestodes, may also be seen scattered in varying numbers throughout the matrix. 42
Sparganosis. Portions of worm are present in a subcutaneous cavity. There is an inflammatory reaction in the surrounding tissue and some fibrosis. (H & E) (Photograph kindly supplied by Professor Robin Cooke)
Echinococcosis is one of the most widespread parasitic diseases globally with an estimated 2–3 million cases, one-third of whom are children. The global burden for human (cystic) echinococcosis due to Echinococcus multilocularis was recently estimated to be more than that for onchocerciasis, although incidence figures do not seem to reflect this (see below), and similar to that due to African trypanosomiasis (see p. 635). 47 It is endemic in parts of Asia, including northwest China. 47
Cutaneous lesions have been reported on the abdomen in two patients with alveolar echinococcosis, an uncommon parasitic disease of the liver caused by the larvae of E. multilocularis. 48 A subcutaneous mass composed of multiple cysts diagnosed as echinococcosis developed in the scapular region of a woman without demonstrable visceral disease. 49 This cestode is closely related to E. granulosus, which causes hydatid disease of the liver and other sites. Subcutaneous lesions are rare with this latter species. 50 Anaphylactic shock, with cutaneous urticarial features, has been reported with hepatic hydatid disease. 51
Onchocerciasis, which is common in tropical Africa, the Yemen, and Central and South America, is caused by the nematode Onchocerca volvulus.52.53.54. and 55. It has been estimated that 18 million people worldwide are infested with this nematode, 56 despite massive intervention campaigns. 57 The larvae are transmitted by several species of flies of the genus Simulium. 58 Onchocerciasis mainly affects people living close to fast-flowing rivers, where the flies breed. 55 The larvae mature into adult worms in the subcutaneous tissue, where they form non-tender subcutaneous nodules 2.5–10 cm in diameter. The nodules, which may occur anywhere on the body, are either isolated or grouped in large conglomerations. Bilateral swellings in the inguinal region (hanging groin) may develop. 59 They may contain one or several tightly coiled worms, which may live for many years.
The adult worms produce microfilariae, which are found in the neighboring lymphatics. The microfilariae may migrate to the dermis and eye. Visual impairment and blindness (river blindness) is an important complication of onchocerciasis. 60 Onchocercal dermatitis, which results from infiltration of the skin by these microfilariae, is a pruritic papular rash with altered pigmentation.53. and 61. The dermatitis is typically generalized, but an eruption localized to one limb, usually a leg, is found in the northern Sudan and also in the Yemen, where it is known as sowda. 62 Pruritic urticarial plaques may also form. 63 Serodiagnosis can be made by a recombinant hybrid protein based ELISA method. 64
It has long been noted that residents of endemic areas show striking differences in infection intensity, which cannot be explained by differences in exposure alone. 57 Some remain free of infection. Genetic resistance to infection with this parasite appears to be linked to chromosome 2p. 57
Ivermectin, an anthelmintic, is used to treat the disease. Unfortunately it is not available because of cost, in some endemic areas. 58
The subcutaneous nodules have an outer wall of dense fibrous tissue which usually extends between the worms (Fig. 29.6). Centrally, there is granulation tissue and a mixed inflammatory cell infiltrate in early lesions, although in long-standing lesions in which the worms are dead there is only dense fibrous tissue, with some calcification and foreign-body giant cells and a chronic inflammatory cell infiltrate.59. and 68. Eosinophils are usually present at all stages. Microfilariae may be seen in lymphatics in this region.
(A) Onchocerciasis. (B) Several fine coiled microfilariae are present in the fibrous tissue that surrounds the worm. (H & E)
In onchocercal dermatitis there is a light superficial and deep infiltrate of chronic inflammatory cells and eosinophils in the dermis. Sometimes the infiltrate is heavy. 69 Microfilariae may be seen in slits between collagen bundles in the upper dermis.66. and 70. Eosinophils and eosinophil major basic protein are usually present around degenerating microfilariae.62. and 65. There is progressive fibrosis of the dermis. The epidermis shows acanthosis and hyperkeratosis. The highest numbers of microfilariae are usually found in the depigmented areas. 56
Gnathostoma spinigerum is endemic in southeast Asia and Japan. Other species of Gnathostoma are rarely implicated.71.72. and 73. Until recently, it has been rare in other countries, including the Americas. 74 Hundreds of cases of gnathostomiasis have been reported recently from Mexico, where it is becoming a public health problem. 75 Human infestation results from eating uncooked, infested meat from the second intermediate host, such as pigs, chickens, and freshwater fish of the genus Ophicephalus. 76 In the cases reported from Mexico the suspected source of infection is the raw fish in the popular dish ‘ceviche’. 75 The nematode may produce migratory cutaneous swellings with localized erythema (nodular migratory panniculitis) which is common in the cases from Mexico, or a true creeping eruption and pseudofurunculosis, which is seen at the site of exit of the worm through the skin.76.77.78.79. and 80. Excoriation of a pruritic patch may reveal the worm, which measures up to 3 cm in length.
In one large series, in which skin biopsies from 66 patients were reviewed, all biopsies showed a heavy inflammatory infiltrate involving the dermis and subcutis. The infiltrates were composed mostly of eosinophils with some admixed lymphocytes and a few neutrophils. Plasma cells were present in a few cases. Flame figures were rare and six cases showed an eosinophilic vasculitis. Focal spongiosis was present in some cases and edema of the papillary dermis was observed in 36 of the 66 biopsies. Larvae were found in 15 cases and, in 12 cases, the worm was retrieved during the biopsy procedure.
Human infection with Dirofilaria spp. is uncommon except in endemic areas, notably the Mediterranean region.81.82.83.84.85.86. and 87. The usual species found in this region is Dirofilaria repens, which may cause subcutaneous nodules. 88 In the case of Dirofilaria immitis (the dog heartworm) pulmonary lesions, which are usually asymptomatic, can also occur. 89 Skin lesions are usually solitary, erythematous, and tender subcutaneous nodules.90.91. and 92. Sometimes there is a sensation of ‘movement’ under the skin. 93
The center of the nodule contains a degenerating filaria with a thick laminated cuticle, distinct longitudinal ridges and large lateral chords, as well as typical musculature. 94 There is an intense surrounding inflammatory reaction of lymphocytes, plasma cells, histiocytes, eosinophils, and sometimes giant cells. There is usually central suppuration, and neutrophils may extend out into the adjacent inflammatory zone. 94 The diagnostic histological features of various zoonotic filariae in tissue sections have been reviewed by Gutierrez. 83
Cutaneous larva migrans commonly occurs in tropical and subtropical countries; most cases seen in the United States and Great Britain have been acquired during travel abroad, but cases contracted in these countries have been reported.95.96.97.98. and 99. It is a self-limiting eruption caused by the intracutaneous wanderings of hookworm and certain other nematode larvae.100.101.102. and 103. The creeping eruption caused by fly larvae is usually considered separately. It is known as migratory myiasis and is not due to a nematode. 104 In larva migrans there are pruritic papules that form serpiginous tunnels, which are at first erythematous but soon become elevated and vesicular. There is a predilection for the feet and other exposed sites, although in one study from an urban slum in Brazil in which 3.1% of the inhabitants examined had this infestation, no case involving the feet was found. 105 Lesions are usually localized, but widespread disease, acquired from sitting on the sand in tropical beach resorts, has been reported. 106 Bullae may rarely form.107. and 108. Folliculitis, usually on the buttocks, is another manifestation of the disease. It presents as follicular papules and pustules. 109 The linear burrows may be in the same area or in a different area to the folliculitis.110. and 111. The lesion may extend several millimeters per day. Older parts of the track may become crusted. The disease has a limited duration as the larvae are unable to complete their life cycle in the human body and usually die within weeks to months.112. and 113.
Epiluminescence microscopy has been used, with mixed success, in the attempted clinical diagnosis of this condition. 114
Larva migrans is most commonly caused by larvae of Ancylostoma braziliense, a hookworm of dogs and cats, but Necator americanus may give a creeping eruption of shorter duration. 1 Other hookworms that may produce cutaneous larva migrans include Ancylostoma caninum, Uncinaria stenocephala, and Bunostomum phlebotomum.
A deep subcutaneous form of larva migrans may be seen with Gnathostoma spinigerum.76.77. and 115. Infection with Toxocara sp. may cause visceral and ocular larva migrans, but not the cutaneous form. Urticaria and prurigo are cutaneous manifestations associated with toxocariasis. 116
The larvae of Strongyloides stercoralis, a soil-transmitted helminth, usually provoke little reaction as they migrate through the skin to reach vessels for their passage to the lung. In some individuals with strongyloidiasis, a variant of larva migrans is found with a rapidly progressing linear urticarial lesion, which may extend at up to 10 cm per hour.117. and 118. The term larva currens (racing larva) has been used for these cases.118.119.120. and 121. There is still a high incidence of Strongyloides stercoralis infestation in former prisoners of war interned many years ago in southeast Asia.122.123. and 124. In one series, almost one-third had suffered episodes of larva currens. 125 Infestation is now being seen in personnel sent to the Solomon Islands for security duties. 126 Another cutaneous manifestation of strongyloidiasis is the presence of widespread petechiae and purpura. 127 These features are seen in immunosuppressed patients with disseminated infections.118.128.129.130.131. and 132. This Strongyloides hyperinfection syndrome, as it is known, is an emerging health problem with a high mortality rate. 133 Prurigo nodularis and lichen simplex chronicus are further manifestations of infection with this parasite.134.135. and 136.
Recently, a creeping eruption caused by larvae of the suborder Spirurina has been reported from Japan.137. and 138. The eating of raw squid has been implicated in these patients.
An ELISA method can be used for its serodiagnosis. A single dose of ivermectin usually cures this disease. 109 Albendazole, another anthelmintic, can also be used. 126
In larva migrans there are small cavities in the epidermis corresponding to the track of the larva, although the parasite itself is uncommonly seen in section. There may be a diffuse spongiotic dermatitis, with intraepidermal vesicles containing some eosinophils. 139 There is usually no inflammatory reaction around the larva (when it can be found), whereas there is a mixed inflammatory reaction behind the migrating larva with a superficial dermal infiltrate of neutrophils, lymphocytes, plasma cells, and usually abundant eosinophils. 139 An eosinophilic folliculitis has been recorded.111.140. and 141.
Reports of larva currens have mentioned a perivascular round-cell infiltrate with interstitial eosinophils, a picture common to many parasitic infestations. 142 In disseminated strongyloidiasis there are numerous larvae, 9–15 µm in diameter, in the dermal collagen and rarely in the lumina of small blood vessels.118. and 128.
Various other nematodes are sometimes of dermatopathological interest. 1Mansonella streptocerca is found in West Africa. The adult worm lives in the dermis, and microfilariae may also be seen. It usually presents with hypopigmented macules and itching. The adult worms of Loa loa, which is endemic in the rainforests of West and Central Africa, live in the subcutaneous tissue and migrate, producing fugitive swellings and temporary inflammation. 143 The elevated outline of the subcutaneous worms may be visible on the skin surface. 144 There is high eosinophilia. Liberation of the microfilariae may produce urticarial lesions. 145Wuchereria bancrofti (Fig. 29.7) and Brugia malayi produce lymphangitis and lymphadenopathy, with the later development of elephantiasis. 146 North American Brugia species rarely cause zoonotic infections in humans. Humans acquire the disease through a mosquito bite. 92 The worm matures to an adult without reproducing. There are no circulating microfilariae. No treatment, other than surgical excision of the lesion is required. 92 A deep cutaneous granulomatous and eosinophilic reaction with fibrosis is found surrounding the parasite. 92 Filarial lymphedema affects an estimated 15 million persons worldwide. 147 Its course is complicated by periodic episodes of acute dermatolymphangioadenitis (ADLA) which may also lead to disease progression. 147 Further discussion is beyond the scope of this chapter.
Sections of the nematode Wuchereria bancrofti are present in a cavity in the subcutaneous fat. There are numerous eosinophils in the adjacent fat. (H & E)
Dracunculus medinensis may produce a blistering lesion due to the migration of the worm, which will eventually be extruded through rupture of the bleb. The female worm measures 70–120 cm in length and is coiled through the subcutaneous tissues. The anterior end is surrounded by granulation tissue containing a mixed inflammatory infiltrate, and there is fibrosis and some inflammation in the deeper parts.






