Hand Tumors
Benjamin Levi
Kevin C. Chung
In this chapter, we will address the management of tumors of the upper extremity, including those of the soft tissues.
GENERAL TUMORS
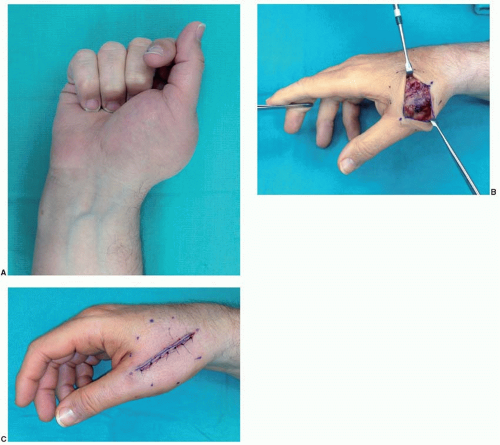
Surgical biopsy incisions should be oriented longitudinally, along the long axis of the limb (Figure 86.1A-C), facilitating subsequent extirpation if required. Incisions should not be oriented transversely (Figure 86.1D). Historic teachings recommend against exsanguination of the arm before tourniquet inflation to avoid spread of the tumor cells; however, no studies have confirmed that this actually occurs.
All tissue that is removed should be sent for pathologic evaluation. The biopsy should ideally include a portion of the tumor as well as some surrounding normal tissue, although this is not always practical. After the diagnosis has been established, the surgeon plans for excision with appropriate margins in a one-stage or multistaged procedure. Most wounds from large tumor excisions can be closed temporarily with a skin graft or skin substitute while awaiting pathologic examination of the margins. If tendon or bone is exposed after deep resection, more complex tissue rearrangements or free tissue transfers may be required, after clear margins are confirmed.
BONY AND SOFT TISSUE TUMORS
General
Malignant tumors of the hand are rare, often leading to delayed treatment.1,2 If a malignant diagnosis is suspected, a tissue biopsy is obtained to establish the diagnosis, to assess the grade and clinical behavior, and to stage the tumor.
|
Histologic Grade and Surgical Staging
Unlike skin cancers, staging of bone tumors of the hand takes into account histologic grade (G) (Table 86.1). The most commonly used classification is as follows:
G0: Benign
G1: Low grade, few cells, much stroma, little necrosis, mature cells, fewer than five mitoses per high-power field
G2: High grade, many cells, little stroma, much necrosis, immature cells, more than 10 mitoses per high-power field
Benign Bony and Soft Tissue Tumors
General.
Benign bone tumors of the hand and forearm are frequently asymptomatic, slow growing, and require no surgical intervention. If these lesions enlarge, become symptomatic, or appear to have an aggressive subtype, however, a biopsy is required.
Ganglions and Mucous Cysts.
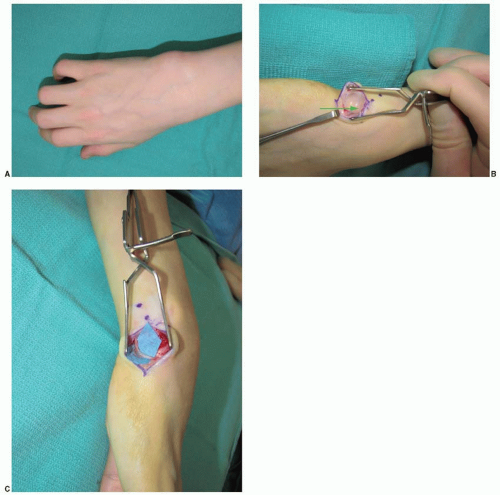
Ganglion cysts are the most common soft tissue masses in the upper extremity and are well-circumscribed, mucin-filled lesions that are attached to the underlying joint capsules or tendon sheaths. Ganglions are most commonly seen in patients 30 to 40 years old and are more common in women. A history of trauma is present in 10% of cases. The most common anatomic location is the dorsal wrist, which represents 60% to 70% of upper extremity ganglions. Sometimes referred to as retinacular cysts, these lesions are postulated to originate from the extensor retinaculum and are usually located over the scapholunate ligament between the second and fourth extensor compartments (Figure 86.2A-C). Dorsal ganglion cysts should be excised under tourniquet control. A transverse ellipse is excised around the tumor in an attempt to avoid its puncture. However, if the cyst is large, the cyst can be punctured when dissection becomes difficult to facilitate excision of the dorsal wrist capsule in continuity with the cyst stalk. During surgical excision of cysts, extensor tendons are visualized and retracted radially and ulnarly in order to avoid damaging them. Cysts over the radial border of the wrist should also be dissected with particular care to avoid the sensory branch of the radial nerve, which can course directly over the cyst (Figure 86.2C).
Ganglion cysts of the volar wrist are often located between the radial artery and the flexor carpi radialis, directly over the distal end of the radius or scaphoid tubercle. These cysts originate from the radiocarpal joint ligaments or scaphotrapezial joint. Radial and ulnar artery patency should be evaluated by an Allen test. The cyst will be attached intimately to the radial artery, which may be injured during dissection. The radial artery should be gently peeled off the cyst which can be punctured to facilitate removal. Volar ganglions are excised in a manner similar to dorsal ganglions; however, the incision is designed to allow for visualization of the neurovascular bundles. To prevent recurrence of all ganglions it is necessary to remove the stalk. Ganglions located in the distal interphalangeal (DIP) joint are called mucous cysts. Mucous cysts are usually seen in older patients and cause attenuation of the overlying skin or grooving in the nail from pressure exerted by the cyst (Figure 86.3A and B). Patients often say these lesions appeared suddenly or over the course of several months. The cysts may also subside or enlarge with activity and rupture. Osteoarthritis is always seen in the underlying joint in these patients. Aspiration may alleviate symptoms; however, this rarely provides a long-term solution.5 The cysts can be excised through a V-shaped incision centered over the lateral DIP joint with skin excision or rotation-advancement flaps.6 More recent studies have demonstrated similar outcomes with a transverse incision centered over the DIP joint. Osteophytes and affected portions of the joint capsule are excised to prevent recurrence.7
Giant Cell Tumor of Tendon Sheath.
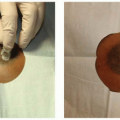
Giant cell tumors of the tendon sheath or benign fibrohistiocytomas represent the second most common soft tissue mass of the hand. These lesions are thought to represent a reactive process and thus do not have single cell type of origin.8 Clinically, giant cell tumors of the tendon sheath present as firm, painless nodules close or adherent to the tendon sheath. These benign tumors can also be found within the tendon sheath and can cause triggering. The most common locations for these lesions are the middle finger, index finger, and thumb, and these lesions grossly appear yellowish or tan (Figure 86.4A and B). Histologically, a large number of histiocytes with no mitotic figures are seen. Surgical excision of the tumor and its stalk is the recommended treatment. When present in phalanges, adequate exposure and visualization of the digital nerves is necessary. Despite complete excision, recurrence of these tumors has been shown to be 13% at 3 years.9
Epidermal Inclusion Cyst.
Epidermal inclusion cysts are the third most common tumor of the hand. The palm and fingertips are the most commonly affected regions, and these masses are more common in individuals with occupations susceptible to common penetrating hand injuries. These lesions are thought to form after penetrating trauma causes implantation of epidermal cells in the dermis. Epidermal inclusion cysts are slow growing, firm, round, nontender masses attached to the overlying skin that are filled with protein, cholesterol, and fat. Complete excision is necessary to prevent recurrence.
Glomus Tumor.
The glomus body is an arteriovenous anastomosis within the dermis that regulates vascular flow for temperature control at the fingertip. Glomus tumors are a benign proliferation of this glomus body.10 Patients present with painful subcutaneous and subungual nodules that are
hypersensitive to cold.11 Glomus tumors can also appear as a subungual bluish discoloration with or without overlying nail plate changes. Radiologic diagnosis can be made by magnetic resonance imaging (MRI) on which the T2-weighted images are characteristic. Treatment of choice for glomus tumors is currently surgical excision through a transungual approach, which has been shown to provide a low recurrence rate and rare nail deformities.12,13,14
hypersensitive to cold.11 Glomus tumors can also appear as a subungual bluish discoloration with or without overlying nail plate changes. Radiologic diagnosis can be made by magnetic resonance imaging (MRI) on which the T2-weighted images are characteristic. Treatment of choice for glomus tumors is currently surgical excision through a transungual approach, which has been shown to provide a low recurrence rate and rare nail deformities.12,13,14
Osteoid Osteoma.
Osteoid osteoma is a benign bone tumor found in the fingers, wrist, or distal radius. The classic presentation is nighttime pain, swelling, and tenderness that are relieved by aspirin. A small radiolucent lesion with a sclerotic margin is present on plain radiographs. If untreated, this tumor may resolve, though it can take several years. If nonsurgical management is employed, aspirin is prescribed for pain. Recently, radiofrequency ablation has become popular for osteoid osteomas proximal to the wrist. Due to the proximity of these tumors to neurovascular structures in the hand, radiofrequency ablation is not recommended distal to the wrist.15 Surgical treatment includes marginal resection, or curettage and bone grafting. Clinical history differentiates this tumor from an osteoblastoma which is histologically identical. Furthermore, osteoid osteomas are more commonly cortical, medullary, or subperiosteal, whereas osteoblastomas are usually medullary in origin.
Osteochondroma.
Although a common tumor of the general skeleton, osteochondromas are rare within the upper extremity. Osteochondromas originate in the physis or regions of tendon insertion.16,17,18 Though rare in the hand, they are most commonly seen in the distal aspect of the proximal phalanx in the second to third decade of life.19 Clinically, osteochondromas cause the overlying skin to protrude and may mechanically inhibit range of motion, as well as cause tendon
snapping, irritation, and rupture.20,21 Radiographically, they appear as bony exostoses, and histologically they demonstrate a benign cartilage cap similar to that seen in the epiphysis. These lesions can be left undisturbed, but resection is recommended and curative if functionally debilitating. Though the potential for malignant transformation exists in the general skeleton, such degeneration has not been reported in the hand.
snapping, irritation, and rupture.20,21 Radiographically, they appear as bony exostoses, and histologically they demonstrate a benign cartilage cap similar to that seen in the epiphysis. These lesions can be left undisturbed, but resection is recommended and curative if functionally debilitating. Though the potential for malignant transformation exists in the general skeleton, such degeneration has not been reported in the hand.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree