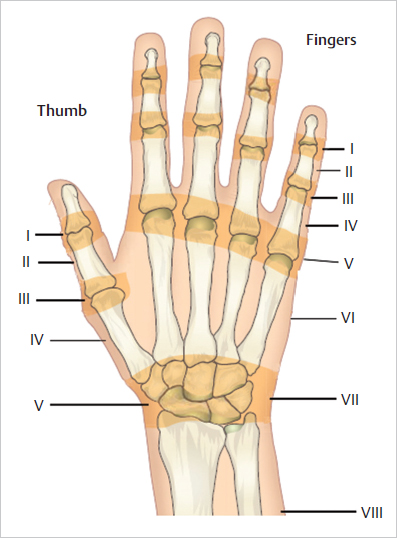
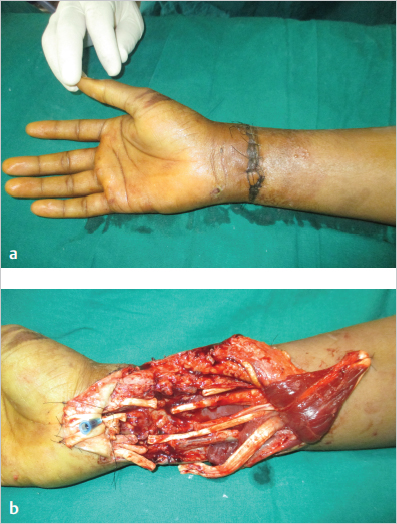
21 Hand Trauma Abstract Hand injuries are the most common injuries that occur in the workplace and often involve young people. Complications following even the “simple” injuries could lead to severe morbidity and lifelong disability to the individual. A systematic examination to assess injury to the tendons, nerves, bones, and blood vessels is important. All injured structures can be primarily repaired if the surgeon is confident of primary wound healing. Primary wound healing depends upon good debridement. When the injuries are associated with soft-tissue loss, skin cover with either grafts or flaps must be achieved as early as possible. In hand injury management, first time is the best time to get good results. Good management of hand injuries needs skilled surgeons experienced in the management of hand injuries, a supportive infrastructure, and supervised postoperative physiotherapy. If any of the required components of care are not available, it is better to refer the patient to the center where it would be available. With a better understanding of the healing of various structures of the hand and the advent of microsurgery, good outcomes are possible even in major injuries with loss of various tissue components. Microsurgery has made it possible to reattach even totally amputated hands and fingers. While amputated parts with no muscle like the fingers and thumb can stand long periods of ischemia, proximal amputations with large muscle component have to be revascularized within a few hours. Awareness of the possibility of replantation and indications will help surgeons to refer the patients to the replantation center. Accurate assessment of the injury, followed with appropriate care and physiotherapy can help get good functional outcomes even in major injuries. Keywords: mangled hand, amputation, tendon injury, fracture, osteosynthesis, replantation, rehabililtation Hand is a commonly injured part of the body. Almost 40% of all injuries that happen in the workplace are to the hands affecting people in the most productive years of life. While in most parts of the body, wound healing is the end point, in the hand, restoring function is the end point. Proper assessment of the injury, with appropriate management provided at the right time, could result in a good outcome. Most patients would also need to undergo supervised rehabilitation protocols. If any one component of care is missed, it could result in severe morbidity to the individual. It could also result in an economic disaster with loss of employment and productivity, which the individual and the society could ill afford. Uniquely, the ultimate outcome depends upon the decisions made by the first doctor who examines the patient. So familiarity with the examination of an injured hand and the principles of its management is a must for a trauma surgeon. Remember • Forty percent of all injuries at the workplace are to the hands. • Ultimate outcome depends upon the initial diagnosis and appropriate primary care. The structure and the capability of the hand distinguish the human being. In the hand, the second and the third rays act as stable rays, whereas the thumb and the ulnar two metacarpals possess movement. The position and mobility of the thumb are unique. The range of movement of carpometacarpal joint of the thumb is critical for hand function. Apart from the movement of the thumb, a length of at least up to the neck of the proximal phalanx is considered critical for function. Functional capability is drastically reduced with shorter thumb and a total loss of thumb equals 40% loss of function of the hand. Every structure in the hand is well adapted for function. The palmar skin is thick, whereas the dorsal skin is thin and is loosely attached. So edema of the hand is more pronounced in the dorsum and it can pull up the metacarpophalangeal (MCP) joints into a nonphysiological position of hyperextension. The fibrous septa in the hand and fingers hold the volar skin tight and help in gripping. The sensation of the fingertips can distinguish points with a gap of 3 to 4 mm. The neurovascular bundle in the fingers lies volar to the midlateral line, with the nerve lying volar to the artery. In the thumb, the digital nerves lie on either side of the flexor tendon ( Important surface landmarks are useful in examining the hand. On the volar side, the distal wrist crease corresponds to the proximal limit of the flexor retinaculum, which extends distally for another 3 cm. The flexor retinaculum is attached to the pisiform and the hook of the hamate, which are both palpable on the ulnar side and to the tubercle of the scaphoid (a palpable landmark on the radial side) and the ridge of the trapezium. The distal palmar crease corresponds to the level of the MCP joints of the fingers and the proximal palmar crease in the base of the hand indicates the position of the carpometacarpal joint of the thumb. Any plasters crossing these lines will restrict the movement of the joints. The hand is well supplied by radial and ulnar arteries, with the ulnar artery mainly contributing to the superficial palmar arch and the radial artery to the deep palmar arch. While the extensive anastomosis can compensate for injuries of a particular vessel, in major crush injuries it is advisable to repair blood vessels to get pulsatile blood flow into the hand, which helps in wound healing, improved survival of local flaps, and planning secondary reconstruction. The flexor tendons to the finger and the thumb reach the hand through the carpal tunnel. There is one flexor tendon for the thumb (flexor pollicis longus), whereas two for each finger (flexor digitorum profundus [FDP] and flexor digitorum superficialis [FDS]). The flexor tendons pass through an intricate system of fibro-osseous sheaths called pulleys. The FDS lies superficial to the FDP tendon up to the MCP joint level. At this level, the FDS tendon splits into two slips and through it the FDP becomes superficial to the FDS. The FDS is inserted at the middle phalanx and produces proximal interphalangeal (PIP) joint flexion. The FDP is inserted at the base of the distal phalanx and produces distal interphalangeal (DIP) joint flexion. Depending upon the relation of the flexor tendon to the pulley system and the surrounding anatomical structures, they are divided into five zones ( Fig. 21.1 Surface anatomy of the hand. (a) The line of digital nerves to the thumb. (b) The line of radial digital nerve to the index. (c) Dotted line shows the level of the metacarpophalangeal joints of the fingers. (d) Dotted line shows the carpometacarpal joint of the thumb. Plaster extending beyond these lines (c, d) blocks movement of the respective joints. Fig. 21.2 Zones of the flexor tendon I to V (thumb TI-TV) in relation to important structures. FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis. FDP traverse in the narrow space of the pulley system. Repair of these tendons in this zone is considered a challenge, and hence the name of “no man’s land.” One has to be very precise in surgical technique to get a good result of flexor tendon repair at this level. At zone 4, all the flexor tendons are packed in a small space (carpal tunnel) along with the median nerve. An injury at this zone typically involves multiple structures. The pulleys prevent bowstringing of the tendons. There are five annular pulleys and three cruciate pulleys. A2 and A4 pulleys are considered important for function ( Extensor tendon system is equally important. They are divided into nine zones. Odd numbers are used for regions overlying joints, whereas even numbers represent the regions between joints ( If the injured hand is not severely bleeding, the first few minutes of the patient examination must be spent on enquiring about the nature of the accident, the time of occurrence, handedness, occupation, and recreational demands of the individual. Comorbidities, if any, must be noted. Each factor has an important bearing on the management. If the hand has been injured in a roller injury or subjected to prolonged compression, the damage will be more than what is initially obvious. Time of occurrence of the injury will have a bearing on the decision to replant or revascularize the distal part. Surgical procedures are chosen depending on the work of the individual and the demands the hand will be put to. All major injured patients must go through the advanced trauma life support (ATLS) protocol so that an associated injury is not missed. Prophylactic antibiotics and tetanus prophylaxis must be administered. Hand injuries attract attention and if this protocol is not followed, it might lead to missed injuries and a poor outcome. Fig. 21.5 (a) In the event of complete division of a vessel, the muscular walls contract and occlude the bleeding. (b) In the event of a partial division, the same mechanism opens up the rent and maintains it open, resulting in severe bleeding. Fig. 21.6 Blind plunging of the artery forceps to control bleeding from the ulnar side wound can include the ulnar nerve as well. If the patient arrives with significant bleeding, the best way to control the bleeding is to apply a sterile dressing over the injured area and apply direct pressure over the bleeding surface with a compression dressing and elevate the injured part above the level of the heart. Bleeding will stop in most instances with this step in a few minutes. If significant bleeding persists, a partial injury to the vessel should be suspected. Whereas in a complete injury the contractile mechanism of the vessel wall helps control the bleeding, in a partially injured vessel it stretches the tear, making it wider ( Good outcomes in hand injury management are achieved when the wound heals primarily and the injured structures are primarily repaired. The hand is packed with functional tissues and therefore multiple structures may be damaged and it is quite easy to miss nerve or tendon injuries. The safe axiom is to consider all structures beneath the skin wound to be injured unless proved otherwise. Vascularity of the hand and fingers is assessed by feeling the pulse and checking the color of the fingertips as well as capillary refill, which should be less than 3 seconds. If the fingertip is pale or congested, a vascular injury must be suspected. If the pulses are not felt in the injured limb although it is present on the other side or when a pulse oximeter does not pick up signals, a vascular injury is suspected. The absent pulse must not be attributed to vascular spasm or shock. In closed injuries, a hand-held Doppler can be run along the course of the main vessels. An abrupt drop in signals denotes the possible site of vascular injury and merits early exploration. Rarely do we resort to angiograms in upper limb injury. Compartment syndrome is a situation of vascular compromise to tissues in a tight osseofibrous compartment. Bleeding inside a closed compartment, vascular injury, and muscle injury all could cause a reduction in the arteriovenous gradient preventing circulation in the muscles. Whenever the compartment pressure increases over 40 mm of Hg, circulation to the muscles is compromised. It may occur even in the presence of a palpable pulse in a major vessel. Whenever there is pain out of proportion to the injury accompanied by swelling and firmness over the compartment, compromised circulation should be thought of. Pain, pallor, paralysis, and pulselessness are the common findings, but the diagnosis of compartment syndrome should be done in the stage of pain itself. Pain and increased resistance on passive stretch of the fingers is the key to diagnose compartment syndrome. Because of the increased resistance component, this test could be used even in an unconscious patient. When present, it is an indication for careful frequent monitoring and if there is no improvement in a couple of hours, urgent decompression of the compartment should be done. Compartment pressures can be measured, but the person should be experienced in the technique to avoid false results. Time must not be wasted in doing an angiogram to diagnose compartment syndrome. The fingers have a normal resting cascade due to the tension of the musculotendinous units and any deviation from the norm in the presence of good joints could be due to tendon injury. On the flexor side, this is seen as inability of the fingers to maintain the cascade, whereas on the extensor side it is reflected by drop of the finger. When the extensor injury is close to the DIP joint, it causes mallet finger and at PIP joint it leads to boutonniere deformity. The patient is requested to actively go through the range of movements of the joints. While loss of movement occurs in complete injuries, even 10% of intact tendon will allow the patient to go through the full range of movement. Partial tendon injury should be suspected if there is pain on resisted movement of the fingers. In injuries in the palm and fingers, triggering of the finger could denote a partial injury with the injury site being caught at the rent in the pulley. In injuries to extensor tendons on the dorsum of the hand, finger extension might still be possible even with complete division of the tendon due to the presence of juncturae tendinae. The size of the wound has no bearing on the structures injured. Wounds due to knife or glass pieces are notorious for causing extensive injuries ( Missing nerve injuries is the commonest cause of litigation in hand injuries. The nerves are suturable structures to the level of the middle of the pulp of the fingertip and hence injured nerves should be repaired. In the acute stage, the patient may not be aware of the loss of sensation. To diagnose a nerve injury, we need to systematically examine the muscles supplied by the nerve and distal sensation. While testing sensation in the emergency room, instead of asking the patient whether the patient feels the stimulus, we need to compare it with the uninjured side and ask the patient whether there is a difference between the two sides. If there is a difference, a nerve injury is suspected and the wound should be explored. In proximal injuries, sensation in the area of autonomous zones is checked (
21.1 Introduction

21.2 Relevant Anatomy
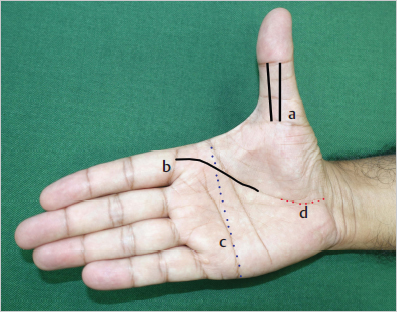
 Fig. 21.1). The position of the nerves has to be kept in mind when performing digital blocks or exploring wounds. Digital nerves are identifiable and suturable structures almost to the level of the middle of the distal phalanx and as such must be repaired in cases of injury. Unrepaired digital nerves, apart from loss of sensation, can cause painful neuromas.
Fig. 21.1). The position of the nerves has to be kept in mind when performing digital blocks or exploring wounds. Digital nerves are identifiable and suturable structures almost to the level of the middle of the distal phalanx and as such must be repaired in cases of injury. Unrepaired digital nerves, apart from loss of sensation, can cause painful neuromas.
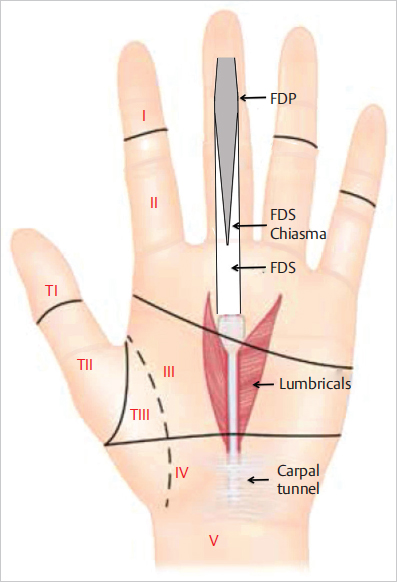
 Fig. 21.2). In zone 2, both the FDS and
Fig. 21.2). In zone 2, both the FDS and
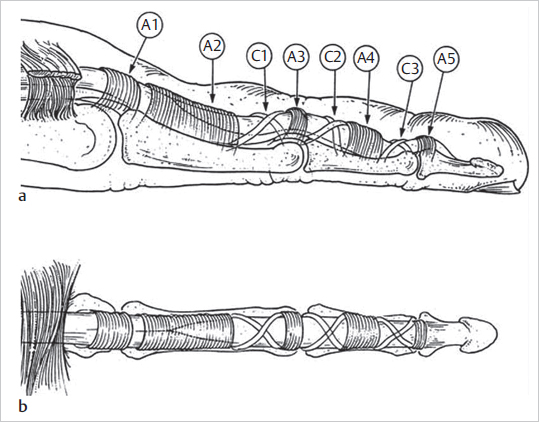
 Fig. 21.3).
Fig. 21.3).
 Fig. 21.4). Distal to the MCP joint (zones 1–5), the extensor tendon is very flat and thin. Repairs of the tendon at these levels cannot be very strong; hence, they always require protection after repair, mostly in the form of a wire across the joint that the tendon is acting on.
Fig. 21.4). Distal to the MCP joint (zones 1–5), the extensor tendon is very flat and thin. Repairs of the tendon at these levels cannot be very strong; hence, they always require protection after repair, mostly in the form of a wire across the joint that the tendon is acting on.
21.3 Assessment of an Injured Hand
21.3.1 The Primary Survey
21.3.2 Controlling Bleeding
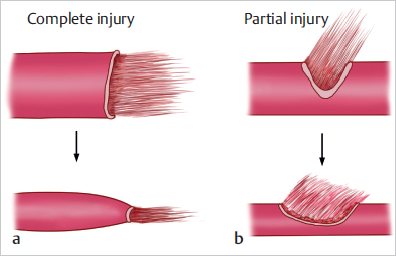
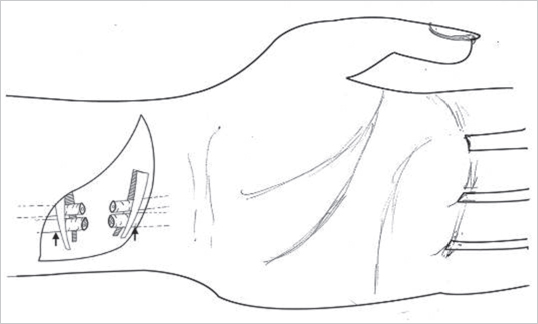
 Fig. 21.5). In such cases, it is safer to inflate a tourniquet proximal to the level of injury. The tourniquet should be inflated beyond the systolic pressure and the time of application must be noted. Patients with an unanesthetized arm can tolerate a tourniquet for about 20 minutes, which would be adequate to seek the needed help. Even in such instances, a well-applied direct pressure will help control bleeding. The one measure that should not be done is to blindly plunge in hemostats to catch the bleeders. Important structures like nerves and tendons go along major vessels in the hand and this step has the risk of injuring them, making direct repair impossible (
Fig. 21.5). In such cases, it is safer to inflate a tourniquet proximal to the level of injury. The tourniquet should be inflated beyond the systolic pressure and the time of application must be noted. Patients with an unanesthetized arm can tolerate a tourniquet for about 20 minutes, which would be adequate to seek the needed help. Even in such instances, a well-applied direct pressure will help control bleeding. The one measure that should not be done is to blindly plunge in hemostats to catch the bleeders. Important structures like nerves and tendons go along major vessels in the hand and this step has the risk of injuring them, making direct repair impossible ( Fig. 21.6).
Fig. 21.6).
21.4 Identification of the Injured Structures
21.4.1 Vascular Supply
21.4.2 Tendons
 Fig. 21.7).
Fig. 21.7).
21.4.3 Nerves
 Fig. 21.8). These are the minimum areas of overlap of sensory innervation between the three major nerves in the hand. The commonly used classification of nerve injuries is given in
Fig. 21.8). These are the minimum areas of overlap of sensory innervation between the three major nerves in the hand. The commonly used classification of nerve injuries is given in  Table 21.1. Edema following closed compression injuries and electrical burns could cause compression of the median nerve in carpal tunnel. Hypoesthesia of the tips of the radial three fingers should raise suspicion of carpal tunnel compression, which if undetected could result in permanent sensory loss and intrinsic muscle paralysis.
Table 21.1. Edema following closed compression injuries and electrical burns could cause compression of the median nerve in carpal tunnel. Hypoesthesia of the tips of the radial three fingers should raise suspicion of carpal tunnel compression, which if undetected could result in permanent sensory loss and intrinsic muscle paralysis.
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine