HAND INFECTIONS
I. GENERAL CONSIDERATIONS
A. Risk factors
1. Diabetes
2. IV drug abuse
3. Immunocompromised state
4. Alcoholism
B. Most common organisms
1. *Staphylococcus aureus
a. *80% of all infections
b. Rising incidence of methicillin-resistant Staphylococcus aureus (MRSA)
2. Streptococcus species
3. Many infections (Intravenous drug abuse, farm injuries, bite wounds, immunocompromised pts) are polymicrobial
C. Antibiotic choice
1. Increasing incidence of MRSA in many regions
a. Vancomycin in severe infections
b. Clindamycin is an alternative (avoid with erythromycin-resistant isolates)
2. Special situations
a. *Human bites: Must cover gram negative for Eikenella corrodens
i. Ampicillin/sulbactam (parenteral)
ii. Amoxicillin/clavulanic acid (oral outpatient)
iii. Clindamycin plus fluoroquinolone (PCN allergic)
b. Gram-negative bacterial infections
i. Fluoroquinolones
ii. Piperacillin tazobactam
II. FELON
A. Definition: Deep infection of the pulp of the distal aspect of the fingers or thumb
B. Numbers: 15% to 20% of all hand infections.
C. Causative agents: Staph. aureus
D. Indication for surgical treatment: Fluctuance within the pulp of the finger requires I&D
E. Treatment
1. It is critical to fully explore the pad to disrupt septations between the distal phalanx and finger pad. This allows for adequate drainage of the abscess.
2. Gauze packing can be used in the wound to prevent re-accumulation of purulent material
3. BID soaks using a dilute hydrogen peroxide solution can be initiated 12 to 24 hours after surgery
4. Antibiotic therapy should be started empirically and tailored based on wound cultures. Initially, IV antibiotic therapy is sometimes warranted depending on severity or presentation.
______________
*Denotes common in-service examination topics
A. Definition: Infection of the soft tissues around the nail fold
B. Presentation
1. Acute: Swelling and erythema around the nail bed with or without abscess formation
2. Chronic: Long-standing infection with inflammation of soft tissues of nail fold that can result in intermittent drainage and nail changes (ridges, thickening, discoloration)
C. Numbers: Most common soft-tissue infection of the hand
D. Causative agents
1. Acute: Staph. aureus
2. *Chronic: Candida albicans
E. Treatment
1. Acute without abscess formation
a. Warm soaks TID
b. Oral antibiotics
c. Protection of affected digit
2. Acute with abscess formation
a. Abscess drainage: Use a Freer or other small periosteal elevator to elevate fold in area of inflammation
b. Use a scalpel to open any abscesses taking care to avoid damage to the nail bed; send fluid for culture and sensitivity
c. Partial or complete nail removal may be required in some cases. Be sure to stent open the nail fold to allow for organized nail regrowth.
3. Chronic
a. Marsupialization of peronychium
b. Excise a 3-mm-wide crescent of skin only from the base of the nail
c. Avoid removal of subcutaneous tissues
d. Nail removal
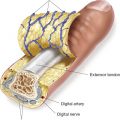
IV. FLEXOR TENOSYNOVITIS
A. Definition: Infection involving the flexor tendon sheath
B. *Kanavel’s signs
1. *Pain with passive extension (earliest and most sensitive sign)
2. Flexed posture of finger
3. Fusiform swelling of entire digit
4. Pain along the course of flexor tendon
C. Treatment
1. True flexor tenosynovitis is an urgent surgical issue.
2. Be aware of the horseshoe abscess (infection of the thumb and small finger tendon sheaths communicating via Parona’s space)
3. Broad-spectrum IV antibiotics should be started once cultures have been obtained or sooner if the operating room is not immediately available.
4. Surgical techniques
a. Irrigation of the flexor tendon sheath
i. Mid-lateral incision at the distal aspect of the A4 pulley
ii. Transverse incision in the palm proximal to the A1 pulley
iii. Initial thorough irrigation of the tendon sheath in the operating room
iv. Catheter can be left in place for continuous or intermittent irrigation postoperatively.
b. Open debridement
i. All wounds overlying the flexor tendon should be opened and aggressively debrided
ii. If advanced infectious changes like sinus tracts or necrotic tissue are present, a Bruner incision should be made over the flexor tendon sheath.
iii. The flexor tendon sheath should be opened preserving the A2 and A4 pulleys. All purulent and necrotic material should be removed.
iv. Wounds can be left to heal by secondary intention with appropriate wound care/dressings.
1. Predictors of poor outcomes
a. Age over 43
b. Medical comorbidities: Diabetes, peripheral vascular disease, or renal failure
c. Subcutaneous purulence
d. Digital ischemia
e. Polymicrobial infection
2. Amputation rates
a. No purulence or digital ischemia → no amputations, 80% return of total motion
b. Subcutaneous purulence → 8% amputation, 72% return of total motion
c. Subcutaneous purulence and digital ischemia → 59% amputation, 49% return of total motion
V. DEEP SPACE INFECTIONS
A. Numbers: 5% to 15% of all hand infections
B. Deep spaces within the hand
1. Subaponeurotic space: Dorsum of the hand deep to the digital extensor tendons and superficial to the metacarpals.
2. Thenar space: Bordered by index finger profundus tendon volar, fascia over-lying the adductor pollicis dorsal, the thumb metacarpal and proximal phalanx radial, and the midpalmar or oblique septum ulnar.
3. Midpalmar space: Bordered by the flexor tendons volar, the third, fourth, and fifth metacarpals dorsal, the midpalmar or oblique septum radial, and the hypothenar septum ulnar.
4. Hypothenar space: Bordered by the hypothenar muscular fascia volar and ulnar, the hypothenar septum radial, and the fifth metacarpal dorsal
5. Interdigital spaces
6. Parona’s space: Bordered by the flexor tendons volar and the pronator quadratus dorsal.
C. Communications
1. Between thenar and hypothenar spaces via Parona’s space.
2. Between the dorsal and volar aspects of the interdigital spaces “collar-button abscess”.
3. Between midpalmar and either thenar or hypothenar compartments.
D. Treatment
1. Incision and debridement
2. IV antibiotics
3. Avoid limited incisions
4. Avoid incisions in web space
E. Postoperative care
1. Wound packing
2. Healing by secondary intention
3. Failure to improve within 24 to 48 hours of surgery likely signals the need for re-exploration
VI. SEPTIC ARTHRITIS
A. Mechanism: Typically penetrating trauma
B. Presentation: Pain, erythema, and swelling of the affected joint
C. Diagnosis
1. Aspiration of the joint for cell count, gram stain, and culture
2. Cell count greater than 50,000 white blood cells (WBCs) with greater than 75% polymorphonuclear cells.
D. Treatment
1. Requires urgent surgical treatment to salvage joint motion. Irrigation and debridement of joint with wound left to heal by secondary intention.
2. IV antibiotics usually for a 4- to 6-week course
A. Mechanism: Direct trauma or contiguous spread after a trauma
B. Organisms: Staph. aureus and Streptococcus most common
C. Diagnosis
1. Can be difficult as X-ray findings arise late in the disease process
2. Erythrocyte sedimentation rate and C-reactive protein are often normal
3. X-ray findings
a. Osteolysis (70%)
b. Osteopenia (10%)
c. Osteosclerosis (10%)
d. Periosteal reaction (10%)
e. Sequestrum or involucrum (5%)
4. Diagnosis made with bone biopsy: Gold standard
D. Treatment
1. Surgical debridement of necrotic bone
2. Culture-guided antibiotic therapy
VIII. BITE WOUNDS
A. Human bites—“Fight bite”: All wounds over the metacarpal head must initially be treated as though the joint has been violated
2. Organisms: S. pyogenes, S. aureus, and *E. corrodens
3. Treatment
a. Irrigation and debridement
b. IV antibiotic therapy with coverage for Gram-negative bacilli
B. Animal bites
1. Organisms: Staphylococcus, Streptococcus, oral anaerobes, and *Pasteurella multocida (cats)
2. Dog bites
a. Rarely become infected (4%)
b. Incidence: 1 million bites/year
c. Characteristics
i. Avulsion: Torn structures
ii. Crush injury
iii. Devitalized tissue
iv. Can have larger zone of injury than initially appreciated
d. Bugs: P. multocida (50% of domestic dogs), Staph. aureus, Streptococcus viridans, and Bacteroides
e. Treatment
i. Consider extending wound for drainage
ii. Thorough irrigation
iii. May close some wounds (face), otherwise loosely approximate
iv. Tetanus
v. Augmentin/timentin with close follow-up
vi. 10-day surveillance of animal if suspicious for rabies
3. Cat bites
a. Often become infected (50%).
b. Bugs: P. multocida most common (two-thirds of domestic cats)
c. Characteristics: Puncture wound with deep inoculum
d. Treatment
i. Irrigation and debridement, elevation, splinting, physical therapy (PT)
ii. IV antibiotics for infected wounds
IX. HERPETIC WHITLOW
A. Causative agent: Herpes simplex 1 and 2
B. Transmission: Direct contact with infected individuals. Healthcare workers are at increased risk if proper gloves are not used.
C. *Presentation: Throbbing pain followed by vesicles that ultimately drain and resolve over a 1- to 2-week period. Can also be associated with a viral prodrome. Can also mimic paronychia.
D. Diagnosis: *Clinical but can be confirmed on Tzanck smear and viral cultures.
E. Treatment
1. *Observation
2. Acyclovir can shorten the course if administered within 48 to 72 hours of the start of the illness
3. Avoid debridement
X. OTHER INFECTIONS REQUIRING EMERGENT SURGERY
A. Necrotizing fasciitis
1. Mechanism of infection
a. Small or large trauma
b. More than 60% of infections caused by self-injection into the upper extremities
2. Presentation
a. *Pain out of proportion with exam
b. Bullae
c. Sloughing of skin
d. Crepitus or gas in tissues
e. Symptoms of septic shock with an otherwise unimpressive soft-tissue infection.
3. Organisms
a. Streptococcus pyogenes (group A Streptococcus) is most common
b. Anaerobes as well as Clostridium spp., other Streptococcus spp., and Staphylococcus spp. have also been identified.
4. Treatment
a. Broad-spectrum empiric IV antibiotics including clindamycin which targets toxin production.
b. Surgical debridement via extensile incisions to remove all necrotic tissues. Survival depends on a thorough debridement.
c. Send samples for culture as well as pathology
B. Clostridial myonecrosis: “Gas gangrene”
1. Mechanism of infection: Generally following a trauma or elective surgery. Farm injuries are at especially high risk.
2. Presentation: Edema within hours of inoculation followed by necrosis of fat, muscle, and subcutaneous tissue. Hydrogen sulfide and carbon dioxide gases are produced resulting in crepitus in limb.
3. Organisms
a. Clostridium perfringens is most common
b. C. novyi, C. speticum, C. histolyticum, and others
4. Treatment: Similar to that for necrotizing fasciitis. Hyperbaric oxygen has been shown to be a useful adjunct in treatment.
XI. FUNGAL INFECTIONS
A. Cutaneous infections
1. Examples
a. Tinea corporis (glabrous)
b. Tinea manuum (palm)
c. Onychomycosis (nails)
2. Diagnosis: Fungal culture via potassium hydroxide preparations
3. Treatment
a. Topical antifungals
b. Systemic oral griseofulvin or ketoconazole
B. Soft-tissue infections
1. Sporotrichosis
a. Trauma from plants, particularly rose thorns
b. Presentation: Superficial ulceration that spreads along lymphatic tracts
c. Treatment: Oral potassium iodide or itraconazole
C. Deep infections
1. More often seen in immunocompromised hosts
2. Presents as septic arthritis, tenosynovitis, or osteomyelitis
3. Organisms can include histoplasmosis, blastomycosis, Cryptococcus, coccidioidomycosis, and aspergillosis, among many others
4. Treatment: Surgical debridement followed by IV antifungals.
XII. ATYPICAL HAND INFECTIONS
A. Presentation: Unusually presenting often slowly progressive infections that can often be misdiagnosed. Immunocompromised hosts are at greater risk.
B. Causative agents
1. Mycobacterium marinum: Found in both freshwater and saltwater
2. Mycobacterium kansasii: Soil
3. Mycobacterium avium complex
C. Diagnosis
1. Biopsy
2. Culture at 31°C and 37°C for extended period of time (sometimes months)
D. Treatment
1. Debridement of wounds including thorough synovectomy
2. Chest X-ray to look for systemic disease
3. Antibiotics: Extended (3 to 6 m) course of a combination of oral antibiotics, including rifampicin, isoniazid, ethambutol, and clarithromycin.
COMPARTMENT SYNDROME
I. GENERAL CONSIDERATIONS
A. Definition: Elevation of hydrostatic pressure within a closed anatomic compartment that impairs oxygen delivery to tissues
B. Causes
1. Blunt trauma
2. Fractures
3. Burns
4. Penetrating trauma
5. Vascular injury
6. Injection injury
7. Electrical injury
II. COMPARTMENTS OF THE UPPER EXTREMITY
A. Arm
1. Anterior
2. Posterior
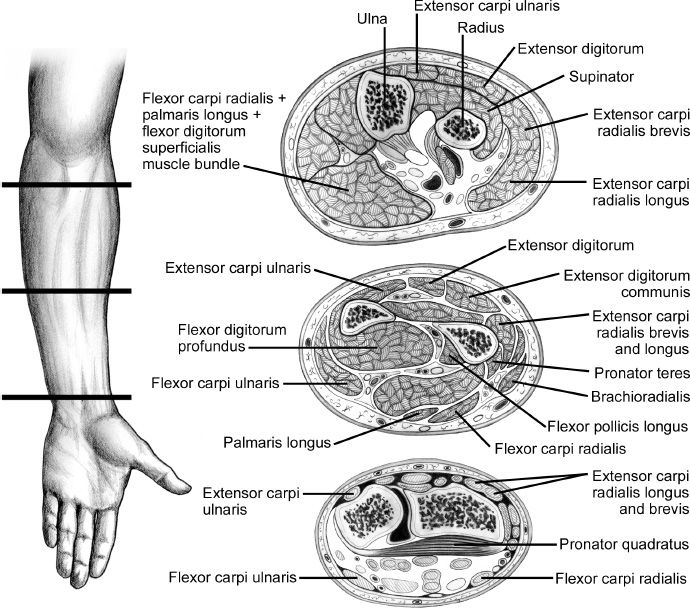
B. Forearm (Fig. 48-1)
1. Flexor compartment (superficial and deep)
2. Mobile wad (brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis)
3. Dorsal compartment
C. Hand
1. Thenar
2. Hypothenar
3. Adductor pollicis
4. Four dorsal interosseous
5. Three volar interosseous
III. DIAGNOSIS
A. History
1. Trauma
Figure 48-1. Cross-sectional anatomy of the forearm compartments. (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
2. Fractures
3. Casts, dressings
4. Coagulopathy
B. Physical exam
1. *Six Ps
a. Pain out of proportion to injury
b. Pain on passive stretch of muscles in affected compartment
c. Pallor (uncommon finding)
d. Paralysis
e. Paresthesias
f. Pulselessness (last finding, usually a sign of irreversible muscle necrosis)
2. Palpation: Unreliable means of determining compartment pressures
3. Measuring compartment pressures
a. Stryker compartment pressure monitor
i. Depress syringe until a drop of fluid appears at the bevel of needle
ii. Zero the instrument with its syringe parallel to the floor
iii. Insert and slightly depress the plunger of syringe
iv. Read compartment pressure after about 5 seconds
v. Stryker monitor is not designed for hand compartments and may give inaccurate readings.
b. Arterial line setup with manometer may be used otherwise
a. Compartment pressure >40 or >30 mmHg with clinical symptoms
b. Difference between diastolic pressure and compartment pressure of <30 mmHg.
c. Important to follow the trend of compartment pressures, not one value in time only (when possible).
IV. TREATMENT
A. Immediate surgical release of affected compartments
B. Prophylactic fasciotomies in certain cases
1. Obtunded patient with equivocal findings
2. Revascularized extremities after prolonged ischemia time
3. *Electrocution
4. Circumferential burns
C. Surgical approaches
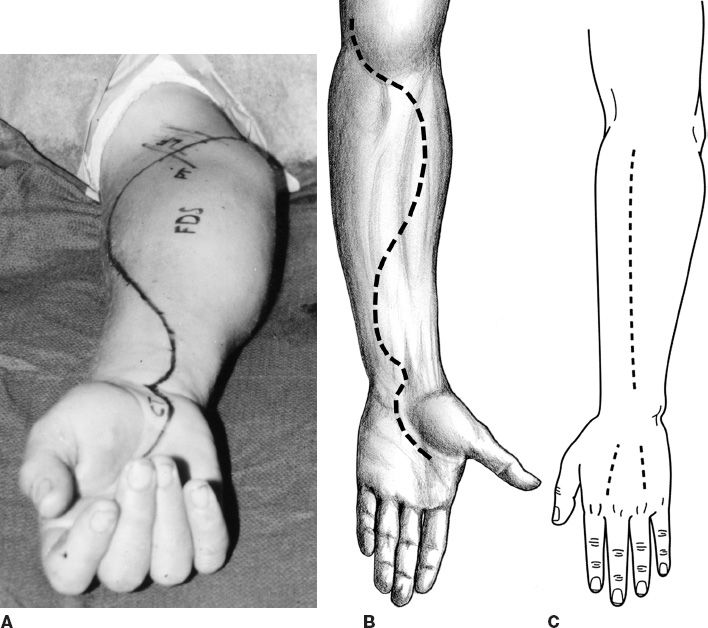
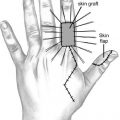
1. Forearm (Fig. 48-2)
a. Variety of approaches can be made—preference to start at carpal tunnel and end at medial epicondyles.
Figure 48-2. Fasciotomy of the forearm. A and B: One design for a volar incision for fasciotomy. Many have been used. The volar fasciotomy incision should be designed to permit decompression of the volar forearm muscles and the carpal tunnel, and it should be angled over the wrist crease to avoid formation of a constricting scar band at the wrist. C: Incisions for dorsal fasciotomy should permit decompression of the extensor muscles of the forearm and also the intrinsic muscles of the hand. (A and B from Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
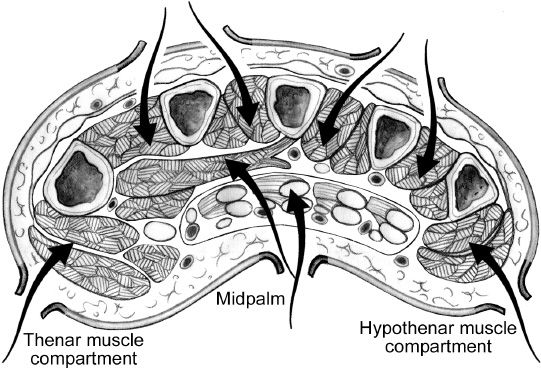
Figure 48-3. Fasciotomy of the hand. Cross section through the mid-palm that demonstrates the pathways (arrows) that are used to release the dorsal interosseous, palmar interosseous, the adductor pollicis, thenar, carpal tunnel, and hypothenar compartments. The dorsal incisions, which are 3 to 4 cm in length, are centered over the mid-portion of the metacarpals. (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
b. Ulnar approach comes between flexor digitorum superficialis (FDS) and flexor carpi ulnaris (FCU), releasing deep and superficial flexor compartments between FDS and flexor digitorum profundus (FDP).
c. Dorsal compartments released through a linear incision over muscle mass
d. Pitfalls
i. Inadequate release of compartments
ii. Failure to explore deeper aspects of volar compartment
iii. Poor flap planning can lead to exposure and desiccation of nerves and vessels
2. Hand (Fig. 48-3)
a. Parallel longitudinal incisions over second and fourth metacarpals
i. All interossei
ii. Adductor pollicis
b. Thenar space: Longitudinal incisions along first metacarpal
c. Hypothenar space: Longitudinal incision along fifth metacarpal
V. UNTREATED COMPARTMENT SYNDROME
A. Muscle fibrosis and death: Volkmann ischemic contracture usually takes 6–12 hours to develop. Most likely to affect deep compartment muscles such as FDP and FPL.
B. Nerve injury and dysfunction: Median nerve often affected more significantly than the ulnar nerve
C. Typical posture of the involved hand and forearm
1. Elbow flexion
2. Forearm pronation
3. Wrist flexion
4. Metacarpophalangeal extension
5. Interphalangeal flexion
D. Classification (Tsuge)
1. Mild
a. Only FDP involvement
b. No nerve injury
a. Involvement of FDP, flexor pollicis longus, PT, and to a lesser extent FDS and FCU
b. Sensory neuropathy of median and ulnar nerves
3. Severe
a. Involvement of all flexors and variable extensor involvement
b. Severe neurologic injury
E. Treatment
1. Mild: Splinting
2. Moderate
a. Flexor pronator slide
b. Tendon transfers
3. Severe
a. Muscle debridement
b. Neurolysis
c. Tendon transfers
d. Free muscle transfers
HIGH-PRESSURE INJECTION INJURIES
I. GENERAL CONSIDERATIONS
A. Mechanism: Paint guns, power washers, hydraulic hoses, grease guns all have the capability to inject large volumes under high pressures
B. Chemicals frequently introduced
1. Paint
2. Cleaning solutions
3. Hydrocarbons
4. Water
II. PRESENTATION
A. Innocuous wound or point of entry
B. Relatively few symptoms including mild pain
III. HISTORY AND PHYSICAL EXAM
A. Agent injected
B. Pounds per square inch of tool being operated
C. Timing of injury
D. Location of wounds
E. Assessment of compartments
IV. TREATMENT
A. Initiate broad-spectrum antibiotic coverage
B. Water or air injections: Observation
C. Other agents
1. Decompress involved compartments
2. Debride foreign material
3. Repeat debridements may be needed every 48 to 72 hours to maximally remove the offending substance
4. Region affected often larger than initially appreciated
V. OUTCOMES
A. Overall amputation rate: 30%
1. Amputation by location of injection
a. Finger: 47%
b. Thumb: 15%
c. Palm: 25%
a. Organic solvent injections did better with earlier (less than 6 hours from injury) debridement with a 38% amputation rate
b. Organic solvent injections debrided greater than 6 hours after injury resulted in a 58% amputation rate
PEARLS
1. Hand infections often need surgical management: For obvious abscess or failure to improve from antibiotics
2. Splint and elevate hand infections to help with edema and pain relief
3. Avoid limited incisions as infections can track from one deep space to another relatively easily. Also avoid incisions in the web spaces as contractures can develop.
4. Flexor tenosynovitis is a clinical diagnosis, made using Kanavel’s signs. Most patients do not have all of them, but pain with passive extension is most sensitive/specific.
5. Necrotizing infections require serial debridements every 24 to 48 hours until wound appears stable
6. Compartment syndrome as a diagnosis requires an index of suspicion
7. Prophylactic fasciotomies are reasonable in patients who are obtunded or have a high likelihood of developing compartment syndrome
8. Injection injuries—particularly those with hydrophobic substances like oil paint—are often much worse than they appear at first presentation. Patients must be counseled on possibility of amputation.
QUESTIONS YOU WILL BE ASKED
1. What is the most common offending organism in a human bite? In a cat bite?
Streptococcus.
2. What must you always cover with antibiotics in a human bite? In a cat bite?
a. Eikenella corrodens.
b. Pasteurella multocida.
3. What are Kanavel’s signs? And which is most sensitive?
a. Pain with passive extension (earliest and most sensitive sign).
b. Flexed posture of the finger.
c. Fusiform swelling of the entire digit.
d. Pain along the course of flexor tendon.
Recommended Readings
Compartment Syndrome
Ouellette EA, Kelly R. Compartment syndromes of the hand. J Bone Joint Surg Am. 1996;78(10):1515–1522. PMID: 8876579.
Shuler FD, Dietz MJ. Physicians’ ability to manually detect isolated elevations in leg intracompartmental pressure. J Bone Joint Surg Am. 2010;92(2):361–367. PMID: 20124063.
Tsuge K. Treatment of established Volkmann’s contracture of the forearm. Nihon Seikeigeka Gakkai Zasshi. 1967;40(13):1569–1584. PMID: 6070221.
Injection Injuries
Hogan CJ, Ruland RT. High-pressure injection injuries to the upper extremity: a review of the literature. J Orthop Trauma. 2006;20(7):503–511. PMID: 16891944.
Infection
Aghababian RV, Conte JE Jr. Mammalian bite wounds. Ann Emerg Med. 1980;9(2):79–83. PMID: 7356213.
Bednar MS, Lane LB. Eponychial marsupialization and nail removal for surgical treatment of chronic paronychia. J Hand Surg Am. 1991;16(2):314–317. PMID: 2022845.
Brutus JP, Baeten Y, Chahidi N, Kinnen L, Ledoux P, Moermans JP. Atypical mycobacterial infections of the hand: report of eight cases and literature review. Chir Main. 2001;20(4):280–286. PMID: 11582905.
Chuinard RG, D’Ambrosia RD. Human bite infections of the hand. J Bone Joint Surg Am. 1977;59(3):416–418. PMID: 849960.
Gonzalez MH. Necrotizing fasciitis and gangrene of the upper extremity. Hand Clin. 1998;14(4): 635–645, ix. PMID: 9884900.
Keyser JJ, Eaton RG. Surgical cure of chronic paronychia by eponychial marsupialization. Plast Reconstr Surg. 1976;58(1):66–70. PMID: 935281.
Louis DS, Silva J Jr. Herpetic whitlow: herpetic infections of the digits. J Hand Surg Am. 1979;4(1): 90–94. PMID: 759512.
Neviaser RJ. Closed tendon sheath irrigation for pyogenic flexor tenosynovitis. J Hand Surg Am. 1978;3(5):462–466. PMID: 556478.
Pang HN, Teoh LC, Yam AK, Lee JY, Puhaindran ME, Tan AB. Factors affecting the prognosis of pyogenic flexor tenosynovitis. J Bone Joint Surg Am. 2007;89(8):1742–1748. PMID: 17671013.
Reilly KE, Linz JC, Stern PJ, Giza E, Wyrick JD. Osteomyelitis of the tubular bones of the hand. J Hand Surg Am. 1997;22(4):644–649. PMID: 9260620.
Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 2003;85-A(8):1454–1460. PMID: 12925624.
< div class='tao-gold-member'>